Airway foreign bodies (AFB) are an important cause of morbidity and mortality in the paediatric population. AFB account for approximately 1000 paediatric deaths per year and 80% of all unintentional deaths in children under the age of one year.1–10 Although life-threatening airway obstruction is easily recognisable, the presentation of AFB is most commonly subacute and often results in presentation to general practice. AFB are a diagnostic challenge even for experienced general practitioners (GPs), often presenting with subtle or no aerodigestive/respiratory symptoms and signs.11 To prevent delays in diagnosis and subsequent complications, it is important that a high level of clinical suspicion is maintained when patients present with a vague history or symptoms that may represent AFB. The therapeutic relationship GPs have with the families of young patients allows them to provide an important educational role regarding both the prevention of AFB and appropriate first response to paediatric airway obstruction.12
Epidemiology
AFB occur most commonly in young children, with 80% occurring under the age of three years, and a peak incidence between one and two years of age.1–10 This is because of age-associated oral fixation, increased mobility (eg crawling and walking), development of fine motor control, incomplete molar development impeding chewing, superiorly placed larynx and immature swallow. Fortunately, the protective cough reflex expels a majority of foreign bodies.12,13 However, when aspiration does occur, a majority (>80%) of foreign bodies lodge in the bronchial tree. The right main bronchus is the most common site for an AFB to lodge, as its lumen is wider and it has a more vertical orientation.14 The most common AFB are organic materials such as food and nuts; however, it is the authors’ anecdotal experience that almost any small object can be aspirated.15–17 Younger children are more likely to aspirate foods/organic material when compared with older children, who are more likely to inhale non-food objects.18,19
Presentation and diagnosis
The most crucial diagnostic tool in AFB is history. An in-depth history is mandatory for all suspected AFB and chronic respiratory complaints that may occur secondary to AFB.11 Studies suggest that close to 50% of patients who have an AFB present completely asymptomatically. However, >90% will have a history of aspiration or choking, reinforcing the importance of history in evaluating patients for AFB.20 An AFB classically presents in three phases. The first phase is impaction of the foreign body, resulting in acute coughing, choking, stridor, respiratory distress and potentially cyanosis. Patients then commonly progress to an asymptomatic phase, secondary to the AFB settling in a stationary location in the tracheobronchial tree and a reduction in the respiratory tract reflexes over time. The third phase involves complications secondary to chronic AFB, which can present as infections such as recurrent pneumonia, chronic cough, unilateral wheeze or symptoms that mimic asthma. Further delays in diagnosis can result in bronchiectasis and permanent damage to the pulmonary tissue.11
By the time a patient presents to their GP, they will commonly be in the second or third phase. Any patient with a suspected inhalation/choking episode warrants in-depth evaluation and workup (Figure 1). It is important to elicit the timing, presence or absence of acute airway symptoms such as stridor, increased work of breathing, cyanosis or apnoea and subsequent respiratory symptomatology such as wheeze, cough and signs of respiratory compromise. Eliciting whether a pre-existing upper respiratory tract infection or illness has been present is also important. Upper respiratory tract illness alters the sensation of the supraglottis, reducing the efficacy of the airway protective reflexes. However, it may also complicate the diagnostic process, with many symptoms of AFB overlapping with common respiratory viruses.11,21
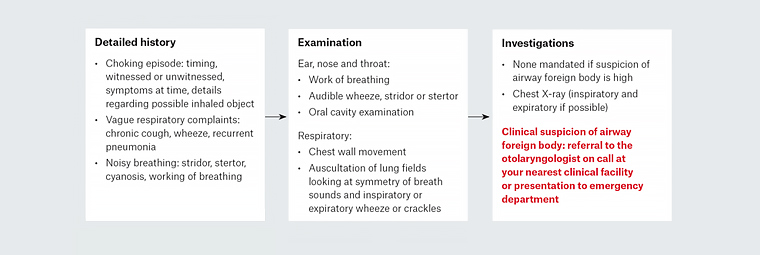
Figure 1. Suggestive algorithm for general practice presentation of suspected airway foreign body
Physical examination includes a complete ear, nose and throat and respiratory examination. Alteration of vital signs is rare but can include tachypnea and hypoxemia. The most common clinical findings include cough and unilateral chest findings such as wheeze, reduced breath sounds and prolonged expiratory phase of respiration.15 A normal physical examination in the setting of a convincing clinical history should not delay referral to a tertiary otolaryngology service for specialist evaluation, as it is common for a patient with an AFB to have normal physical examination findings.
Diagnostic imaging
Normal diagnostic imaging, similar to normal clinical evaluation, does not rule out the presence of AFB. Several studies have shown that as many as 25% of children with bronchoscopy-proven foreign bodies can present with a normal chest X-ray.15 However, imaging can be a helpful tool in diagnosing AFB and subsequent complications. Frontal and lateral chest radiographs are the imaging tools of choice for AFB. These would ideally be performed in the inspiratory and expiratory breath phases, although this is often impractical in young children. Radiopaque AFB are easily diagnosed on chest X-rays but are relatively uncommon, with a recent review showing that only 11% of AFB are radiopaque.22 A majority of AFB are organic and therefore radiolucent, and subtler radiographic findings should be considered. Unilateral hyperinflation, air-trapping, atelectasis or infiltration are classically associated with AFB.21
Referral and tertiary management
Any child with a suspected AFB should be promptly referred to a tertiary otolaryngology service. There is little debate regarding the management of AFB, with clinical suspicion warranting an airway examination under anaesthesia. In the authors’ tertiary paediatric institution, this is a multidisciplinary approach in conjunction with respiratory and anaesthetic colleagues. Patients are booked for both flexible and rigid bronchoscopy to facilitate a complete airway examination. In patients with no acute airway embarrassment, flexible bronchoscopy is performed first because it is less traumatic and allows evaluation of the distal tracheobronchial tree. Rigid bronchoscopy is only performed if AFB is confirmed on flexible examination or if acute respiratory symptoms are present, to allow airway control. Patients may also be booked for rigid oesophagoscopy if there is any historical suggestion of oropharyngeal obstruction. Complications of airway endoscopy are rare, seen in 1–8% of airway endoscopy. Most AFB retrieval is uncomplicated, with children discharged from hospital in the subsequent 24 hours. The most common complications include pulmonary infection and atelectasis, especially in the setting of delayed AFB diagnosis. More rarely, laryngeal oedema, airway obstruction, airway perforation or failure to retrieve the foreign body can occur.23
Prevention and education of the public
Children are naturally inquisitive, and despite careful parental supervision, AFB can still occur. GPs are uniquely positioned, given their therapeutic relationships with patients, to provide education in a way that other specialist services cannot. GPs can provide potentially life-saving advice to the parents and caregivers of young children that can undoubtedly prevent some of the catastrophic outcomes secondary to AFB that are seen by tertiary centres. The role of education is supported by the American Academy of Pediatrics, which recommends that education regarding aspiration/choking be provided to all caregivers of children aged >6 months.12
Discussion with parents/caregivers about the importance of age-appropriate foods and safe meal habits cannot be overemphasised. As discussed previously, the majority of AFB are foods. Therefore, parents and families should be educated by GPs to withhold certain foods until a child is old enough to chew and swallow them. The Royal Children’s Hospital, Melbourne recommends that no child aged <15 months should be offered commonly aspirated foods such as popcorn, hard lollies, raw carrot or apples. Additionally, it recommends that children should not be offered nuts or food containing nuts before the age of four years. Nut butters/pastes are a safe alternative to introduce nut protein into young children’s diet to reduce the risk of food allergy. Children should be encouraged to sit quietly while eating. Multitasking such as walking, talking and running in the setting of an immature swallow increases the risk of aspiration. As often as possible, children aged <2 years should be offered one piece of food at a time, and food should be cut into large pieces to encourage the child to chew and decrease the risk of accidental aspiration.24
Strict consumer protection guidelines were introduced in Australian in 2008 regarding toys for children <36 months of age. However, toys and other items with small pieces will inevitably be present in any household. Families should be aware of the importance of ensuring all small items are out of reach of young children to lower the risk of potential aspiration.25
In the case of acute airway obstruction secondary to AFB, caregivers should be aware of the appropriate first response. Ideally, all families with young children should have cardio-pulmonary resuscitation (CPR) training; however, this is not the reality. In the event of an acute choking episode, parents should be educated on Australian Resuscitation Council’s guideline on first aid management of airway obstruction secondary to AFB (Figure 2). If parents/caregivers suspect airway obstruction in a conscious child, up to five sharp back blows should be delivered while awaiting emergency services. Back blows are performed with the heel of the palm, directly between the shoulder blades. If back blows do not resolve the airway distress, then a subsequent five chest thrusts should be performed. Chest thrusts are delivered in a similar location and technique to chest compressions. If airway obstruction persists after both manoeuvres, then an alternating pattern of back blows and chest thrusts should continue until the attendance of emergency medical services. If the patient is unresponsive, then an oral cavity sweep can be used to clear solid material from the oropharynx/supraglottis and CPR should be commenced.26 These manoeuvres may be potentially lifesaving in the event of acute paediatric airway obstruction secondary to AFB.
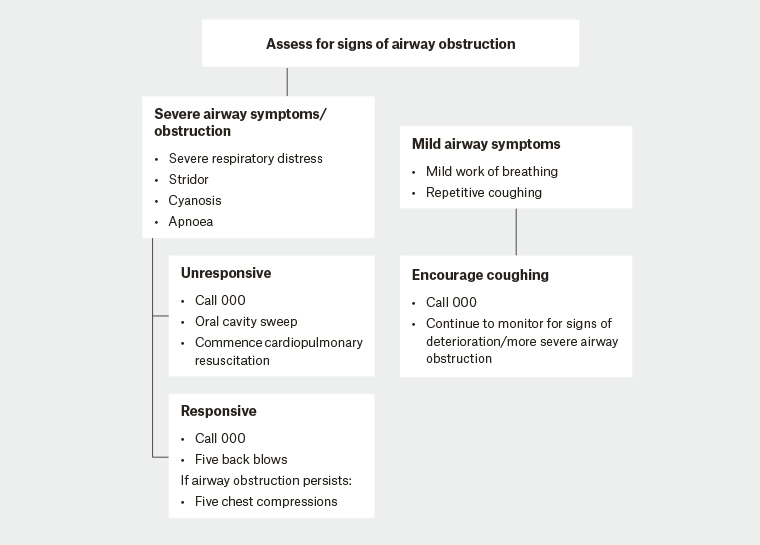
Figure 2. Management of foreign body airway obstruction (choking) algorithm25
Conclusion
Paediatric AFB presents more commonly to GPs than represented in the literature. Patients will often present asymptomatic or with subtle pulmonary findings, with the suggestive history the only diagnostic tool. Nevertheless, these patients require acute tertiary otolaryngology review and management, with potentially lifelong pulmonary complications resulting if diagnosis is delayed. GPs have an important, often lifelong, holistic and therapeutic relationship with patients and families that other specialists often do not. GPs provide an invaluable educational role in the prevention and first response to AFB that has the potential to drastically reduce morbidity and mortality in these patients.