Patients with eyelid lesions often present in the primary care setting, with the majority of eyelid lesions indicating benign pathology. Rarely, eyelid lesions can indicate malignant disease, which has the potential for metastatic spread and associated mortality. Pattern recognition plays a key part in accurate diagnosis and, combined with careful history-taking and clinical examination, allows for prompt management or further investigation as required. This article will cover common eyelid lesions and the approach to investigation and management, as well as key red flag signs and rare conditions not to miss.
Types of benign lesions
Lesions arising from glands
There are three types of glands located in the eyelids: Meibomian, Zeis and Moll. Blockage of any of these glands results in corresponding focal collections/cysts, and these are commonly encountered in general practice. Figure 1 shows some common benign lesions that occur around the eyelid.

Figure 1. Common benign eyelid lesions: Translucent cyst of Moll (upper left), cyst of Zeis filled with sebaceous material (upper right), epidermal inclusion cyst filled with keratin (lower left) and molluscum contagiosum (lower right)
- Cysts of Moll arise from blocked apocrine sweat glands found on the margin of the eyelid. They are solitary dome-shaped papules or nodules filled with clear fluid, making transillumination a key feature.
- Apocrine hidrocystomas are common smooth cysts that are considered adenomas of the secretory cells of Moll rather than classic retention cysts but clinically look similar and may have a bluish colour.
- Cysts of Zeis arise from blocked sebaceous glands, also found on the eyelid margin. These tend to be filled with yellow oily secretions and do not transilluminate.
- Chalazions represent focal granulomatous inflammation due to retained Meibomian gland secretions from a blocked duct and are the most common lid lesion. Meibomian glands are modified sebaceous glands present throughout the upper and lower eyelid, in and around the tarsal plate. Chalazions present as painless nodules within the tarsal plate (posterior aspect of lid) or at the lid margin and can vary in size. Associated blepharitis is common, and clinical signs include eyelid margin telangiectasia, erythema and lash crusting. Symptoms tend to reflect ocular surface discomfort and can include dryness, gritty sensation and/or epiphora (watery eyes). Treatment involves hot compress, massage and eyelid margin hygiene at least twice per day. Antibiotics are not required unless there is evidence of superimposed bacterial infection. Conservative treatment is recommended for at least 1–2 months prior to referral for consideration of incision and drainage.
- Hordeolums (styes) are acute bacterial infections of any of the above blocked glands and are classified as either internal (Meibomian gland) or external (Zeis or Moll). Associated preseptal cellulitis is common and can be treated with a course of oral antibiotics in addition to hot compress and massage. Orbital cellulitis is a rare but potentially sight-threatening and even life-threatening complication that occurs when infection breaches the orbital septum. Differentiating preseptal from orbital cellulitis involves examination of visual acuity, pupils, extraocular movements and the eyelids. A drop in visual acuity, relative afferent pupillary defect or sluggish pupils, painful and limited eye movements, proptosis and chemosis are suggestive of orbital cellulitis and require prompt referral to a tertiary centre emergency department for imaging and antibiotic treatment.
Epidermal lesions
Cysts of the epidermis are the second most common type of benign periocular lesion encountered.
- Epidermal inclusion cysts arise from the infundibulum of the hair follicle and are primarily due to occlusion. These lesions are slow-growing, firm, elevated, round and often have a central pore. Epidermal inclusion cysts are filled with keratin (despite being sometimes called sebaceous cysts), and rupture can incite an inflammatory foreign body reaction. Secondary infection is also possible. Referral for surgical excision is generally recommended.
- Molluscum contagiosum is caused by the molluscum contagiosum virus, a member of the Poxviridae family. Immunocompetent young children and patients who are immunosuppressed are more commonly affected.1 Lesions are characteristically 1–3 mm white, pink or flesh-coloured nodules with a central umbilication. Molluscum contagiosum may also cause a follicular conjunctivitis because of shedding of the molluscum virus into the tear film. Treatment is usually not required as the lesions will spontaneously resolve over time. For rare cases that are very symptomatic (eg those that cause local irritation), cryotherapy or curettage can be used, but referral to an ophthalmologist may be warranted given the locally destructive treatment modalities.
- Xanthelasma are lesions in the superficial dermis and subdermal tissue containing lipid-laden macrophages. These are sometimes associated with raised cholesterol or congenital disorders of lipid metabolism requiring further investigation and management. Surgical excision can be considered for cosmetic reasons.
Benign tumours
Benign tumours are also known as epidermal proliferations. The term papilloma refers to a group of various benign epithelial proliferations that can affect the eyelid skin. Figure 2 shows common benign eyelid lesions.

Figure 2. Benign proliferative lesions: Amelanotic naevus (upper left) in comparison to pigmented naevus (upper right), seborrheic keratosis (lower left) and squamous papilloma (lower right)
- Seborrheic keratosis is the most common benign lesion that affects elderly patients and carries no risk of malignant transformation.2 It is most commonly described as a well-demarcated, waxy, pigmented lesion with a ‘stuck on’ appearance. However, on the eyelid, seborrheic keratoses may be lobulated or pedunculated. Excision can be considered for cosmetic purposes or if the seborrheic keratosis is large enough to interfere with vision. If there are no concerns about the eyelid structure or function being affected, excision may be performed by the general practitioner (GP).
- An acrochordon is also known as skin tag, fibroepithelial polyp and squamous papilloma. These lesions are clinically in appearance: classical narrow-based pendunculated; broad-based sessile; hyperkeratotic similar to cutaneous horn.
- Verruca vulgaris (viral wart) is caused by epidermal infection with human papillomavirus, typically type 6 or 11. These lesions are most commonly found at the eyelid margin as non-pigmented papules with digitations. Cryotherapy can be used to prevent viral spread, but this should be performed cautiously around the eyelid area.
Benign melanocytic lesions
Pigmentation can be seen in both benign and malignant lesions and does not necessarily imply melanocytic origin. Conversely, lesions of melanocytic origin may not be visibly pigmented (eg amelanotic naevus).
- Naevi are flat or raised lesions that arise from melanocytes and are common on the eyelid. Naevi progress through three stages, starting in childhood as a junctional naevus that is a flat, pigmented macule located in the dermoepidermal junction. It then becomes an elevated compound naevus in the second decade, involving both the dermoepidermal junction and dermis, before involuting later in life and losing pigmentation by the seventh decade. Third-stage naevi are known as dermal naevi and involve the dermis only. Transformation to melanoma is rare, but can occur in junctional or compound naevi.
Vascular lesions
- Infantile haemangiomas, previously known as strawberry or capillary haemangiomas, are lesions with a classic red/pink appearance that are common in children. The vast majority of these lesions involute and self-resolve by the age of 10 years. Rarely, they can cause ptosis, refractive error and amblyopia. All children with eyelid infantile haemangiomas should be referred to a paediatric ophthalmologist to assess for potential refractive error and monitor for amblyopia.3
- Port wine stains are permanent capillary malformations that are present from birth. They are variably sized macular lesions that can be dark red to blue in colour. The lesion grows in proportion with the child and may also gradually become raised and thicker. Port wine stains involving the eyelid may be associated with glaucoma; approximately 18% of children are affected,4 particularly patients with bilateral port wine stain or involvement of both upper and lower eyelids. The prevalence is further increased when associated with Sturge-Weber syndrome,5 with glaucoma affecting 40–60% of these patients.6,7 It is therefore important for the patient to be referred to a paediatric ophthalmologist for monitoring and regular follow-up.
Benign lesions summary
Benign lesions that should be referred include:
- hordeolum with signs of orbital cellulitis – emergency department
- enlarging pigmented eyelid lesion with suspicious features – urgent oculoplastics ophthalmology outpatient referral
- eyelid infantile haemangioma or port wine stain – urgent paediatric ophthalmology outpatient referral
- chronic chalazion that is persistent despite 2–3 months of conservative treatment – non-urgent ophthalmology outpatient referral
- benign lesion that is cosmetically concerning – non-urgent ophthalmology or dermatology outpatient referral.
Sinister signs: When to suspect a malignant lesion
Most eyelid lesions are not malignant, but careful history-taking and examination will reveal important clues when suspecting a more sinister lesion. Skin cancer is Australia’s most common cancer, with two-thirds of Australians being diagnosed with a skin cancer before the age of 70 years.8 The eyelids are involved in 10% of cases of skin cancer,9 and the vast majority are basal cell carcinomas (BCC). Risk factors for developing skin cancers, as with systemic cutaneous skin cancer, include: fair skin, history of previous skin cancer, excessive sun exposure, previous radiation, immunosuppression and smoking.10
Clinical signs that should arouse suspicion are listed in Table 1. Anatomically, lesions of the medial canthus are known to be more aggressive because of proximity to the lacrimal drainage system, increasing the risk of tumour spread.11 Eversion of the upper eyelid during examination can reveal lesions otherwise missed with an external-only exam or a more extensive lesion than initially expected (Figure 3). Loss of lashes and/or destruction of eyelid architecture is often a telltale sign of malignancy. Central ulceration, especially if associated with ‘flaky’ skin, can represent the more aggressive squamous cell carcinomas (SCCs). When suspecting a malignant lesion, it is essential to examine the regional lymph nodes (preauricular in particular), as well as check sensation around the periocular area, particularly in the distribution of the infraorbital nerve for lesions of the lower eyelid or lateral canthus. Any loss of sensation may indicate perineural invasion.
| Table 1. When to suspect malignancy |
| History |
Exam |
- Risk factors: prior skin cancer, fair skin, previous radiation, immunosuppression
- Gradual enlargement
- Painless
|
- Ulceration
- Induration
- Irregular or ‘pearly’ borders
- Destruction of eyelid margin
- Loss of lashes (madarosis)
- Telangiectasia
- Reduced sensation
|
Rarely, eyelid lesions can indicate highly malignant disease with potential for distant spread. Melanoma of the eyelid is extremely rare, accounting for <1% of eyelid lesions. More common but less well known is sebaceous carcinoma, a clinical and histological ‘masquerader’ with up to a 30% five-year mortality.12 Sebaceous carcinoma often presents as chronic eyelid inflammation or a non-resolving chalazion that gradually increases in size. Figure 3 describes a case of sebaceous carcinoma initially misdiagnosed as a chronic chalazion.

Figure 3. Importance of eyelid eversion: An extensive upper eyelid sebaceous carcinoma, the full extent of which can be better appreciated with eversion. This patient presented with chronic upper eyelid changes initially misdiagnosed as chalazion.
If a malignant lesion is suspected, the patient should be referred to either an oculoplastic ophthalmologist or to a tertiary care hospital for further evaluation. Where possible, a biopsy of the lesion will be performed for preoperative planning, and intraoperative margin control is preferred for any malignant lesion. Although the majority of lid lesions encountered have low metastatic potential, larger lesions are associated with more difficult reconstruction and associated ocular morbidity. Early diagnosis is key. Malignant lesions encountered are described in the following section, and Figure 4 shows commonly encountered malignant and premalignant lesions.
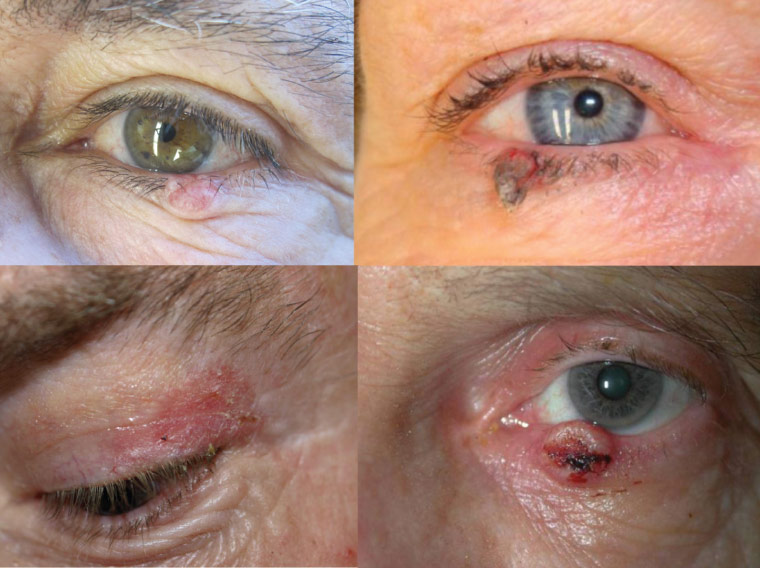
Figure 4. Malignant eyelid tumours: A basal cell carcinoma presenting as an isolated nodule with associated telangiectasia and loss of lashes (upper left), keratoacanthoma (upper right), actinic keratosis (lower left) and invasive squamous cell carcinoma with central ulceration (lower right)
Types of malignant lesions
Basal cell carcinomas
BCCs are the most common eyelid malignancy, accounting for 80–90% of cases, and are typically found on the lower eyelid or medial canthus.13 These are typically slow-growing, locally-destructive skin cancers with a low propensity for metastatic spread. A classical presentation of a BCC is the nodular type – a smooth, pearly-edged nodule with telangiectasia. As the tumour enlarges and outgrows its nutrient supply, central tumour necrosis may occur, leaving a central ulcer. Multiple other histological subtypes of BCC have been described including morphoeic, superficial, infiltrative, micronodular and linear.14 Most cannot be distinguished clinically, but if initial biopsy reveals an aggressive subtype, surgical planning can be adapted accordingly.14 Complete surgical excision with intraoperative margin control is the gold-standard treatment for eyelid BCC, regardless of histological subtype, and is associated with low rates of recurrence.
Actinic keratosis
Actinic keratosis is a common precancerous skin lesion that has potential to develop into an SCC and is found on sun-damaged skin. The risk of malignant transformation is only 0.24% per year, but over an extended follow-up period, the incidence of SCC in an individual with multiple actinic keratoses is as high as 12–16%.2 Actinic keratoses present as scaly, hyperkeratotic plaques with a sandpaper-like texture. Although they are usually treated with cryotherapy, when located on the eyelid margin, surgical excision is generally recommended. Topical imiquimod is an alternative option that requires dermatology referral.
Keratoacanthoma
Keratoacanthoma has previously been considered a benign lesion but more recently is regarded as a low-grade SCC for which complete excision is recommended. It has a characteristic dome-shape with a central crater filled with keratin and may be associated with surrounding inflammatory changes.
Squamous cell carcinomas
SCCs account for approximately 5% of epithelial tumours of the eyelid but are much more aggressive than the more commonly encountered BCC.15 SCCs develop either spontaneously or from actinic keratosis, Bowen’s disease (SCC in situ), keratoacanthomas or radiation dermatosis. They are more common in immunocompromised patients, particularly following solid organ transplant. SCCs can be difficult to distinguish from BCCs; however, they usually have more scaling and may have an adherent crust or associated ulceration. Prompt referral is required given the higher rates of regional nodal (24%), perineural (8%) and distant metastatic (6%) spread.16 For this reason, margin-controlled excision is the gold-standard treatment, although newer targeted therapy involving the hedgehog pathway and epidermal growth factor receptor have been promising in patients with advanced metastatic disease.17
Sebaceous carcinoma
Sebaceous carcinoma is a rare but frequently misdiagnosed tumour (Figure 3). It accounts for 1.0–5.5% of all eyelid malignancies and was previously thought to be more common in people of Asian ethnicity, although recent evidence suggests more equal incidence across all ethnicities.18 Sebaceous carcinoma arises from the Meibomian glands within the tarsus and presents either as a solitary nodule or diffuse eyelid thickening, often with associated inflammatory changes. Anatomically, given the similarities with chalazion, these lesions are often misdiagnosed initially. Although sebaceous carcinomas are rare, any chronic chalazion associated with a gradual increase in size or persistent, diffuse eyelid inflammation and associated thickening (sometimes only evident with eyelid eversion) should raise suspicion. These tumours are aggressive, with metastatic and mortality rates up to 30%, as well as an associated high risk of recurrence.12 Management generally involves excision with intraoperative margin control and conjunctival mapping biopsies, or Mohs micrographic surgery.
Melanoma
Melanomas account for <1% of all eyelid malignancies.19 The lower eyelid is more commonly involved. Any pigmented lesion that increases in size, has irregular borders or multiple colours or is associated with ulcerating and bleeding warrants further investigation.
Malignant lesions summary
- An enlarging lesion, destruction of eyelid architecture, loss of lashes or induration/ulceration (Table 1) may indicate malignant pathology.
- Urgent referral is required to outpatient pathway to oculoplastic ophthalmologist or tertiary care centre.
- Malignant lesions are generally treated by clinical biopsy followed by surgical excision.
Conclusion
Patients with a variety of eyelid lesions present to the GP (Table 2). The majority of eyelid lesions represent cystic, inflammatory or benign proliferative lesions. Skin cancers involve the eyelid region in up to 10% of cases, with the vast majority being BCCs, which generally have an excellent prognosis when excised completely. An understanding of the basic anatomy of eyelid lesions, targeted history-taking and an eye for key red flag clinical features will ensure that more sinister lesions will not be missed. Any lesion with features of malignancy should be referred to an oculoplastic ophthalmologist for further evaluation and management.
| Table 2. Types of benign and malignant eyelid lesions |
| Benign lesions |
Benign tumours |
Malignant tumours |
|
Cystic
- Cyst of Moll
- Cyst of Zeis
- Epidermoid cyst
Chalazion
Hordeolum (stye)
Molluscum contagiosum
Xanthelasma
Vascular malformation (port wine stain)
|
Papillomas
- Seborrheic keratosis
- Squamous
- Viral wart
Naevi
Vascular
|
Basal cell carcinoma
- Nodular
- Morphoeic
- Superficial
- Others
Squamous cell carcinoma
- Actinic keratosis (pre‑cancerous
- In situ (Bowen’s)
- Keratoacanthoma
- Invasive
Sebaceous carcinoma
Melanoma
|