Microbial keratitis develops when the ocular defences have been compromised, making the cornea prone to infection. Although this is an uncommon presenting condition to general practitioners (GP), it is potentially vision-threatening if not managed and treated appropriately.1 Careful history and examination are vital for the prompt recognition of this condition. Urgent referral for ophthalmic review is required for management.2
Case
A female office worker, aged 22 years, presented with a three-day history of a painful, red left eye (Figure 1). She reported associated blurred vision, photophobia and yellow purulent discharge. She had worn soft contact lenses for many years with no previous eye issues. She wore two-weekly disposable lenses during waking hours and stored them overnight in a contact lens container with proprietary storage solution. Further history revealed that she slept overnight in her lenses a week ago and often overwore them by up to a month. She did not own a pair of glasses and was still wearing a contact lens in her right eye.
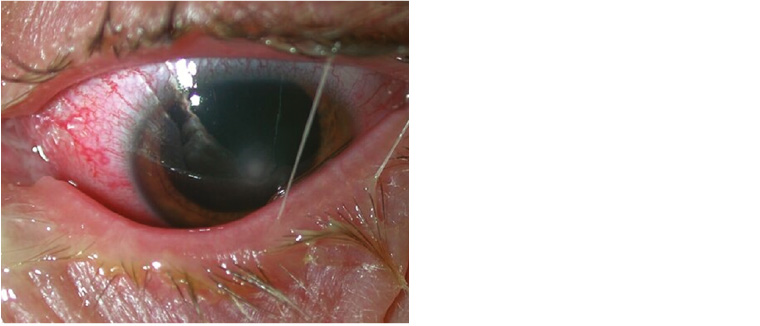
Figure 1. External photograph of bacterial keratitis, showing yellow purulent discharge on the eyelids, intense conjunctival hyperaemia and central opacity in the cornea
Patient risk factors for microbial keratitis include contact lens wear, underlying ocular surface diseases (such as herpetic keratitis, chronic blepharitis or dry eyes), trauma and local or systemic immunosuppressive states.3–5 Patients’ occupations and hobbies should also be explored. Welders, stonemasons, construction workers and farmers have an increased risk of ocular foreign body injuries. Farmers may also be potentially exposed to contaminated water. These factors all increase the risk of developing microbial keratitis.
The major patient risk factor is contact lens wear, especially overnight wear. Overnight wear causes corneal hypoxia and tear stagnation, leading to corneal epithelial compromise.3,6 Patients’ wearing habits – such as the number of hours worn per day, the number of days worn per week and the replacement schedule – should be elicited. The frequency of contact lens aftercare consultation, including cleaning agents and methods used, and online purchase of cosmetic lenses should be explored. Careless lens handling and poor hand hygiene further increase the risks of infection. Formation of microbial biofilms on the lens surface as well as entrapment of microorganisms within the lens itself can occur.4 Storage cases and disinfecting solutions can become contaminated and be a source of infection; therefore, questions relating to replacement of both are warranted.6 However, it must be noted that microbial keratitis can occur with meticulous lens care and even in people who wear daily disposable lenses. Patients should own a pair of glasses in case they are unable to wear their contact lenses.
Symptoms
Early ocular symptoms include general ocular discomfort, dry or irritated eyes and foreign body sensation. Increased eyelid swelling and lacrimation may occur, with the patient reporting difficulty opening their eyes and/or a decrease in vision. Later symptoms include severe pain, photophobia and noticeable eye discharge with significant decrease in visual acuity (Table 1). For patients with microbial keratitis, the pain usually increases with time, unlike a mechanical abrasion, which tends to have pain resolution within 24–48 hours. In general, pain out of proportion to the size of the defect can be due to acanthamoebae, while pain less than expected from the size of the defect may be herpetic in nature.
| Table 1. Causes and key features of the acute, painful, unilateral red eye |
| Differential diagnosis |
Key features |
Conjunctivitis
- Bacterial
- Viral (eg adenovirus)
|
Mild pain, purulent discharge
Mild pain, watery discharge |
Keratitis
- Bacterial/fungal
- Acanthamoebal
|
Severe pain, loss of vision, corneal infiltrate, purulent discharge
Mild-to-moderate pain, loss of vision, ring-shaped infiltrate |
| Scleritis |
Severe pain, loss of vision, extreme hyperaemia |
| Acute glaucoma |
Severe pain, loss of vison, fixed mid-dilated pupil |
| Trauma |
History of trauma including superficial foreign body, intraocular foreign body, chemical burn, blunt, penetrating |
Case continued
On examination, the patient’s visual acuity in the right eye was 6/6 with her contact lens, and in her left eye 6/36 unaided. Through a pinhole, her vision improved to 6/18. The eyelids showed slight swelling and a yellow purulent discharge (Figure 1). On closer examination of the eye, the cornea showed a central 3 mm epithelial defect with a deeper white infiltrate. The conjunctiva was diffuse and intensely injected. Her anterior chamber was quiet, with no obvious hypopyon.
Signs
At the initial consultation, corrected monocular visual acuity at distance should be measured and recorded in both eyes. This should be done with glasses or contact lenses, if the patient is still wearing them. Topical anaesthetic drops (eg oxybuprocaine hydrochloride 0.4%) can be used to relieve ocular discomfort and aid in clinical examination. If there is a decrease in vision, pinhole acuity should be measured with a pinhole occluder that corrects for refractive errors. If no letters can be seen at far or near distances, vision can be recorded as count fingers (CF), hand movement (HM), perception of light (PL) or no perception of light (NPL). It is important to document the visual acuity for medical and potentially legal reasons.
The patient’s lids and ocular surface need to be examined with magnification such as a head loupe and good illumination from a direct ophthalmoscope, pen torch and/or a slit lamp if available (Box 1). Note signs of swelling, redness, discharge, trauma or lid malposition such as ectropion. Inspect the conjunctiva for swelling and/or intense injection, particularly if diffuse rather than sectorial. In the cornea, inspect for any foreign bodies, haze, infiltrates or ulceration. An epithelial defect can be enhanced with the instillation of fluorescein dye and the use of a cobalt blue light. It is important to note the size and location of any corneal ulcers. Any epithelial defect with an infiltrate increases the likelihood of keratitis. Protrusion of the iris indicates perforation of the cornea, requiring urgent emergency referral. The fornix under the upper lid can be further examined by lid eversion, specifically looking for foreign bodies, particularly a retained contact lens (which also stains with fluorescein). Lid eversion can be uncomfortable for the patient and is not possible if the eyelid is very swollen.
| Box 1. Tools for eye examination in general practice |
- Snellen chart
- Pinhole occluder
- Topical anaesthetic eye drops (eg oxybuprocaine hydrochloride 0.4%)
- Head loupe
- Direct ophthalmoscope, pen torch or slit lamp
- Fluorescein solution or strips and cobalt blue light (on direct ophthalmoscope or pen torch filter)
|
The anterior chamber of the eye is inspected for any signs of hypopyon. This may be sterile and therefore an inflammatory reaction to the keratitis, or may indicate intraocular spread of the infection into the eye (endophthalmitis). It is an indicator for more severe keratitis. Irregularity of the pupils may indicate posterior synechiae (adhesion of the iris to the anterior capsule of the lens) due to anterior uveitis. The intraocular pressure may be elevated as a result of blockage of the trabecular meshwork; however, this is difficult to measure without the use of a tonometer. Digital assessment of the intraocular pressure is generally unreliable and also uncomfortable for the patient.
Types of microbial pathogens
The most common infective pathogens in keratitis are bacterial; however, infections can also be fungal, viral or acanthamoebal (Table 2).2
In practice, it is impossible to be certain whether the cause of keratitis is bacterial, fungal (Figure 2) or acanthamoebal. This requires further investigation with corneal scraping, microscopy that may involve special stains and determination of sensitivities to various antimicrobials.
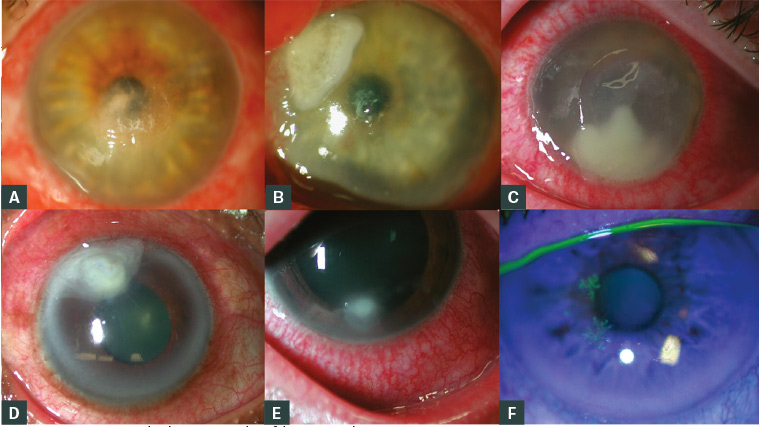
Figure 2. Slit lamp photomicrographs of the varying appearances of keratitis a–c. Bacterial; d,e. Fungal; f. Herpes simplex
| Table 2. Potential pathogens in microbial keratitis |
Staphylococcus spp.
Streptococcus spp. |
Opportunistic pathogens particularly in the compromised cornea |
| Pseudomonas aeruginosa |
Aggressive keratitis causing >60% of contact
lens–related keratitis |
| Moraxella spp. |
Associated with decreased host immune defences (malnutrition, alcoholism, diabetes) |
Neisseria spp.
Corynebacterium diptheriae
Haemophilus influenzae |
Can penetrate intact corneal epithelium |
Candida albicans
Fusarium solani
Aspergillus spp. |
Can cause fungal keratitis; acquired from contaminated water sources, including contact lens solutions |
Herpes simplex virus (type 1 or 2)
Varicella zoster virus |
Can cause viral keratitis from previous viral exposure |
Acanthamoebae
|
Can cause protozoal keratitis; acquired from contaminated water sources, including contact lens solutions |
Fungi
Filamentous fungi (Aspergillus and Fusarium spp.) and yeasts (Candida albicans) are two types of fungi that can infect the cornea.7 Fungal keratitis usually occurs in an already compromised eye with an epithelial defect. Immunocompromised patients or those with a history of long-term corticosteroid use are at increased risk. Filamentous fungi are more common in tropical climates, and infection can lead to corneal perforation.7 Once colonised, fungal keratitis is difficult to eradicate, requiring prolonged use of antifungals and occasionally corneal transplantation to clear the infection.Fungi
Acanthamoebae
Acanthamoebae are commonly found in soils, streams, lakes, chlorinated tap water or swimming pools.8 They exist in two forms, an active (trophozoite) form and a very resistant dormant (cystic) form. Risk factors include swimming in contact lenses, exposure to spa water or storing contacts in homemade saline solutions.8 These organisms derive nutrition from normal bacterial flora and can persist indefinitely in a microbe-rich ocular environment. Patients who present with pain disproportionate to clinical signs or are non-responsive to the usual antibiotics require further investigation with scraping and microscopy specifically for acanthamoebae.
Differential diagnosis
Non-infective differential diagnosis includes marginal keratitis, sterile inflammatory corneal infiltrates associated with contact lens wear, peripheral ulcerative keratitis or toxic keratitis. In practice, it can be difficult to clinically differentiate these infiltrates from a microbial cause and may require corneal scraping. The major infective differential diagnosis is herpetic viral keratitis (Figure 2F), either herpes simplex (type 1 or 2) or herpes zoster ophthalmicus. These lesions tend to be dendritic in shape when involving the epithelium; however, they can appear as an infiltrate if there is stromal involvement. Often there is a history of previous keratitis or cold sores around the lips. Uncommonly, this can occur in conjunction with microbial keratitis, with management required to treat both infective causes.
Management
Microbial keratitis is a medical emergency and should be managed promptly. If the infection is inadequately treated, keratitis will result in scarring of the cornea or even endophthalmitis with permanent loss of vision. Perforation of the cornea can also occur in more severe infections with potential total loss of the eye. Discontinuation of contact lens wear is mandatory for the immediate time and patients should be advised to wear glasses instead. The advice and decision of the GP at the initial presentation is crucial for optimal management, with urgent referral potentially sight-saving for the patient.
It is best to avoid commencing antibiotics until the patient is reviewed by an ophthalmic practitioner, as scrapings of the ulcer will need to be performed and sent for microscopy and sensitivities. If antimicrobials are commenced, the yield from scrapings is greatly diminished and the appropriate therapy delayed unnecessarily. Patients should be advised to bring in their contact lens(es), storage case and solution bottles, as these may also be sent for culture. Once tests have been performed, intensive topical broad-spectrum antibiotics may be commenced, with dilation of the pupil and glaucoma medications if indicated. Less-severe keratitis can be treated on an outpatient basis; however, sight-threatening lesions require hospital admission. Once the microbial infection is identified, antibiotics can be directed towards the specific organism.
Key points
- A red eye with a corneal infiltrate is suspicious of microbial keratitis.
- Patients who wear contact lenses are at greatest risk of developing microbial keratitis.
- Recognition of microbial keratitis can be done in the general practice setting; however, diagnosis may be difficult without the facilities for investigations. There should be a high index of suspicion.
- Management includes urgent referral for ophthalmic review in a hospital emergency department or private clinic.