Case
On a home visit, a woman aged 95 years was observed to have a right-sided head tilt. The patient recalled that her head tilt had been present for the majority of her life. Early childhood photographs confirmed this. At rest, the patient adopted a head tilt towards the right (Figure 1). In this position, she did not have any diplopia. There was facial asymmetry, with hypoplasia of the right face.

Figure 1. Patient in primary gaze
Examination of extraocular muscles found that the patient had vertical diplopia. This was marked on upward gaze and to the right, when her left eye was observed to show limited adduction and elevation with vertical strabismus (Figure 2). No pain was present on eye movements.

Figure 2. Patient in right gaze
Ophthalmological review concluded that the head tilt was due to left congenital fourth cranial nerve palsy, causing weakness of the left superior oblique. No intervention was recommended given the patient’s age and lifelong adaptation. Examination of each eye (when covering the other eye) did not show diplopia in either eye.
Question 1
What is the differential diagnosis of irreversible torticollis?
Question 2
What is the aetiology of superior oblique palsy (SOP)?
Question 3
What is the incidence of SOP?
Question 4
How does SOP present and how is it diagnosed?
Question 5
What is the management of SOP?
Answer 1
The differential diagnosis of irreversible torticollis includes the following conditions:
- Congenital muscular torticollis is the most common cause of torticollis. It can be due to birth trauma or intrauterine malpositioning.1
- Ocular torticollis. Superior oblique palsy (SOP) is the most common type of ocular torticollis.1
- Other rarer forms of non-paroxysmal torticollis are osseous torticollis, peripheral or central nervous system torticollis and non-muscular soft tissue torticollis.1
Answer 2
The cause of this patient’s SOP is most likely congenital neuromuscular pathology (ie hypoplasia of the fourth cranial nerve).2
Other possible causes are:
- traumatic (eg cranial trauma, haemorrhage)2
- microvascular events due to underlying hypertension or diabetes (however, third or sixth cranial nerve palsies are more common in these cases)2
- intracranial space-occupying lesions, although these are rarer causes.2
Answer 3
SOP has an incidence of 5.73 per 100,000 per year.3 However, it is clinically relevant to general practice as the majority of cases will present with diplopia or other visual symptoms, such as difficulty reading.3
Answer 4
Presentation of SOP is most often in the second to fourth decades of life, despite the majority of cases being of congenital origin.3 Delayed clinical manifestation of congenital fourth nerve palsy is due to compensatory mechanisms that control symptoms until later in life, while acquired palsies generally present sooner after the inciting event.3
Fusional vergence amplitude testing uses prisms to assess the patient’s ability to maintain binocular single vision. Large vertical fusional amplitudes indicate chronicity, as does torticollis and facial asymmetry.4
Clinical presentations include:
- diplopia (58%)3
- other problems of visual acuity (24%)3
- SOP on routine eye examination (9%)3
- unspecified strabismus (5%)3
- primarily head tilt (1%).3
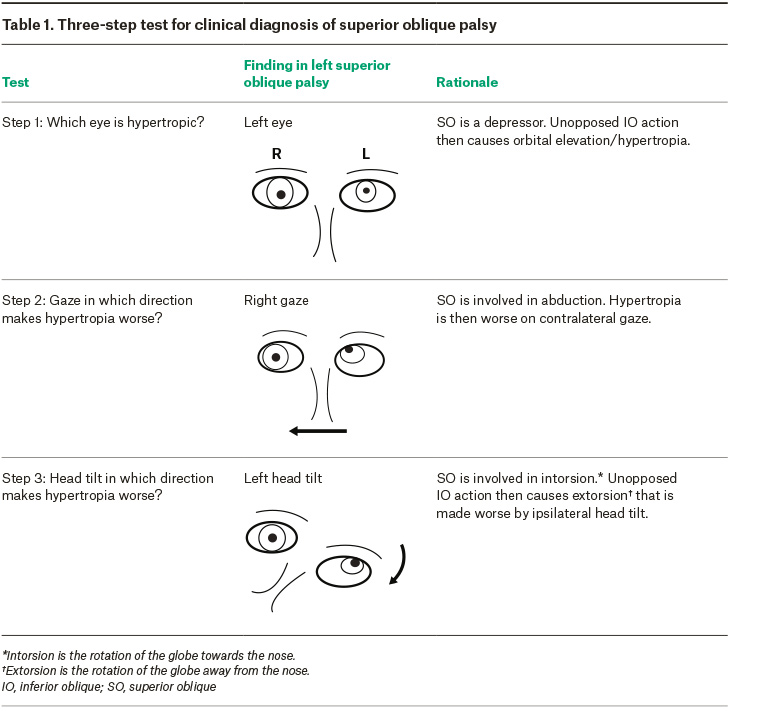
SOP is a clinical diagnosis using the Parks–Bielschowsky three-step test as described in Table 1.5 The three-step test has been found to have a sensitivity of approximately 70%.6
Ophthalmologic referral is required for assessment of visual acuity, and neuroimaging is able to show fourth cranial nerve hypoplasia/absence, superior oblique atrophy and other possible causes.7
Answer 5
If this patient’s SOP had been diagnosed earlier, timely treatment would have improved visual acuity and corrected torticollis.
Non-surgical management, which may be appropriate for mild comitant strabismus, is achieved through the use of refractory prisms or botulinum toxin injection into the ipsilateral inferior oblique muscle.1,7
Surgical intervention is indicated by significant visual symptoms or abnormal head posture.6 Surgery may involve strengthening of superior oblique action or weakening of inferior oblique action to balance muscle action.1,7
Without correction, long-term abnormal head posture can result in permanent contraction of neck muscles and facial asymmetry.1 Permanent torticollis may require a multidisciplinary approach involving ophthalmological, orthopaedic and neurological assessments.8
Key points
- Screening for extraocular muscle palsies using the three-step test should be considered in children with visual problems.
- Early diagnosis should be made to allow for management and avoidance of permanent complications.
- Arrange ophthalmology review when ocular torticollis is diagnosed.