The United Nations High Commissioner for Refugees (UNHCR) has called the Syrian conflict the ‘biggest humanitarian and refugee crisis of our time’. More than five million Syrians have crossed international borders and are registered as refugees. The majority have been hosted by neighbouring countries including Turkey, Lebanon and Jordan.1 In September 2015, the Australian Government agreed to settle 12,000 Syrian and Iraqi refugees in addition to the existing humanitarian intake (13,750 in 2016).
Refugees arriving under the Commonwealth’s Humanitarian Program in Australia have access to healthcare via the public health system and the Medicare Benefits Schedule (MBS). Comprehensive health assessments for refugees are funded under the MBS.2 The Australasian Society for Infectious Diseases (ASID) and the Refugee Health Network Australia (RHeaNA) released Recommendations for comprehensive post-arrival health assessment for people from refugee-like backgrounds in 2016. These recommendations inform what is included in a comprehensive refugee health assessment, with specific recommendations by country of origin and risk.2
Refugee Health Service (RHS), formerly known as Migrant Health, is the state-funded specialist health service for refugees in Adelaide, South Australia. The RHS supports new arrival clients with complex health issues. These complexities include large families, chronic disease, disability, trauma and difficulty accessing mainstream services. Clients are referred to RHS by the humanitarian settlement service or by family members, or they may self-refer.
It is likely that the health status and needs of Syrian refugees will differ from other refugee cohorts arriving in Australia. Refugee populations have traditionally come from low-income countries, often spending extended time in refugee camps, and had poor access to health services, even prior to their displacement. More than 90% of Syrian refugees have settled in the host country community and only a small proportion in refugee camps.1 Prior to the Syrian conflict, the country was undergoing an epidemiologic transition, with the bulk of the nation’s disease burden moving from infectious diseases to chronic and non-communicable diseases (NCD).4
While the complete disruption of the health system in Syria has resulted in several outbreaks including polio,5 measles5,6 and leishmaniasis,7 the major issue facing refugees living in neighbouring countries is the discontinuation of treatment for their chronic diseases.8 Healthcare in a humanitarian crisis is generally poorly equipped to deal with chronic disease management.9,10 NCDs are prevalent in Syrian refugees living in Lebanon, Turkey and Jordan, and access to healthcare was reported as a major issue for this population.8,11,12 It is likely that the Syrian refugee population in Australia will have a high prevalence of NCDs, and these conditions may have been affected by poor access to healthcare.
While acute malnutrition is a growing issue in many areas of Syria itself, especially areas under siege,4,6 it was not found to be an issue for Syrian refugees living in neighbouring countries.14 A large study in Jordan found that Syrian refugee children, on average, were slightly overweight. However, anaemia was still prevalent both in the camps and in refugees settled in the community; >40% of women and children in Zaatari camp and almost 30% of women and children living in the community were anaemic. This has implications for the screening of anaemia, iron and vitamin B12 in Syrian refugees arriving in Australia.
There is little evidence to guide recommendations regarding infectious disease screening in Syrian refugees. The prevalence of hepatitis C in Middle Eastern countries is reported at approximately 1%.15 Evidence suggests chronic hepatitis B rates are approximately 5% in Syria.16,17 Tuberculosis (TB) prevalence in Syria is reported to be 19 per 100,000, which is lower than many European countries and the European average.18
There is scant data available regarding parasite prevalence, including strongyloides, schistosomiasis and soil-transmitted helminths in Syria.21 Cutaneous leishmaniasis is reported to affect the Syrian refugee population in parts of Syria and is spreading to Lebanon.7,22 There is little data regarding the prevalence of sexually transmitted infections in the Middle East or in Syrian refugee populations.
While outside the purpose of this study, it is important to consider mental health issues when caring for people of refugee backgrounds. The World Health Organization predicts that up to 20% of people will develop mild-to-moderate mental health disorders in a humanitarian emergency setting. A larger proportion will demonstrate signs and symptoms of distress and normal reactions to high stress without having a diagnosable disorder.23
Many Syrian refugees report experiencing conflict-related violence and high levels of stress related to displacement such as poverty, food insecurity, fears for safety, discrimination, loss of family, isolation and uncertainty.24 The most common mental health disorders reported in the Syrian refugee population are depression, prolonged grief reactions, post-traumatic stress disorder and anxiety disorders.25
The objective of this study was to describe the health status of Syrian refugees seen at RHS in terms of demographics, prevalence of infectious diseases, nutritional deficiencies, NCDs and non-specific complaints, mental illness, distress and physical disabilities. Findings will help to inform future screening of Syrian refugees, screening guidelines and health service provision and planning.
Methods
Study design
A cross-sectional study was conducted based on a retrospective medical records audit.
Setting
RHS is the state-funded specialist refugee health service in Adelaide, South Australia. The study period was between 1 January 2016 and 31 December 2016.
Participants
Study participants were all new arrival Syrian adults and children who attended RHS within the study period. Participants were referred to RHS by the state settlement service provider. All patients were seen with a qualified interpreter.
Data collected
Data were collected from electronic medical records software (Medical Director) and hard copy records and subsequently populated into a Microsoft (MS) Excel spreadsheet. A list of collected variables is included in Table 1.
| Table 1. Refugee Health Service screening tests and criteria |
| Variable |
Test |
Refugee Health Service screening criteria |
Demographics:
Date of birth/age at assessment
Sex
Country of transit |
N/A |
All participants |
Schistosomiasis – P/N
Strongyloides – P/N
Giardia lamblia
Dientamoeba fragilis
Helicobacter pylori P/N
Human immunodeficiency virus – P/N
Hepatitis C – P/N
Hepatitis B
Chronic hepatitis B
Immune (vaccinated)
Non immune
Past infection
Core antibody positive
|
Serology
Serology
Stool MCS, OCP, NAAT
Stool MCS, OCP, NAAT
Stool antigen
Serology
Serology
Hepatitis B surface antigen, hepatitis B surface antibody, hepatitis B core antibody |
All
All
Age <18 years or abdominal symptoms
Age <18 years or abdominal symptoms
Abdominal pain
Age >15 years
All
All |
| Vitamin D
Normal ≥50 nmol/L
Mild deficiency 30–49 nmol/L
Moderate/severe deficiency <30 nmol/L
Vitamin B12 (active)
Normal ≥31 pmol/L
Deficiency 0–30 pmol/L
Iron studies
Normal ≥31 pmol/L
Deficiency in adults ferritin <30 uG/L
Deficiency in children ferritin <20 uG/L
|
Serum level nmol/L
Serum level
If total vitamin B12 <260 pmol/L, then active vitamin B12 reported
Serum ferritin |
All
All
All |
| Chronic disease
Diabetes
Hypertension
Cardiovascular disease
Chronic respiratory illness (chronic obstructive pulmonary disease or asthma)
|
Patient/clinician reported |
Age >18 years |
| Mental health
Pre-existing diagnosed mental health disorder
Referral to counselling/mental health service
|
Patient/clinician reported |
Age >18 years |
| General symptoms
Chronic headaches
Gastrointestinal symptoms
Musculoskeletal symptoms
|
Patient reported |
|
| Smoking status |
Patient reported |
Age >18 years |
| Body mass index |
Clinician calculated |
Age >18 years |
| Physical disability
Congenital/developmental
Conflict-related injury
Other acquired
|
Patient/clinician reported |
All |
| MCS, microscopy, culture and sensitivity; OCP, ova, cysts and parasites; N/A, not applicable; NAAT, nucleic acid amplification test; P/N, positive/negative |
Data analysis
Data were analysed for descriptive statistics, examining the mean and range for continuous variables, and frequency of cases with percentages for categorical variables. Cross-tabulation was used to determine frequencies within subgroups. Data analysis was performed using STATA 15 and MS Excel.
This study was approved by the South Australian Health Human Research Ethics Committee (reference number HREC/16/SAH/119).
Results
A total of 932 new arrivals registered at RHS in 2016; of these, 455 were Syrian. RHS saw approximately 60% of the Syrians who arrived in South Australia in 2016 (Department of Social Services, Australian Government, email communication, 17 July 2018). All except one individual underwent the new arrival comprehensive health assessment. The health assessment was based on ASID/RHeaNA recommendations for comprehensive health assessment for people from refugee-like backgrounds. The screening pathology tests included full blood count, electrolytes, liver function, hepatitis B serology, hepatitis C antibody, human immunodeficiency virus (for people aged >15 years), schistosomiasis serology, strongyloides serology, iron studies, vitamin D and vitamin B12. All children aged <18 years had stool testing for parasites; stool testing was done for Helicobacter pylori if symptomatic. Adults with gastrointestinal symptoms (pain, diarrhoea) also had stool testing for parasites. While testing for electrolytes and liver function is not included in the ASID/RHeaNA recommendations, calcium and alkaline phosphatase levels assist with interpretation and management of vitamin D deficiency.
Demographic characteristics
Participants ranged in age from <1 year to 81 years, with a mean age of 20.2 years. The population predominantly comprised families with between six and 15 members. Seventy-four Syrian families attended RHS in 2016. More than half were in Lebanon prior to resettlement (Table 2).
| Table 2. Demographic characteristics of Syrian new arrival refugees at the Refugee Health Service, 2016 |
| |
n |
% |
| Sex |
|
|
| Female |
223 |
49 |
| Male |
232 |
51 |
| Age (years) |
|
|
| 0–9 |
145 |
31.9 |
| 10–17 |
123 |
27.1 |
| 18–29 |
49 |
10.8 |
| 30–39 |
66 |
14.5 |
| 40–49 |
44 |
9.7 |
| 50–59 |
17 |
3.7 |
| >60 |
10 |
2.2 |
| Not reported |
1 |
0.2 |
| Children (0–17 years) |
268 |
58.9 |
| Adults (≥18 years) |
186 |
41.1 |
| Transit country |
|
|
| Jordan |
157 |
34.5 |
| Lebanon |
254 |
55.8 |
| Others |
37 |
8.1 |
| Not reported |
7 |
1.5 |
| Total |
455 |
100 |
Infectious diseases
Table 3 shows the prevalence of infectious diseases. Immunity to hepatitis B from vaccination was found in 61.6% of children and 13.4% of adults.
| Table 3. Results of new arrival screening at the Refugee Health Service, 2016 |
| |
Adults (age ≥18 years) |
Children (age 0–17 years) |
| n |
% |
Total |
n |
% |
Total |
| Infectious diseases |
| Schistosomiasis serology* |
18 |
9.7 |
185 |
8 |
3.0 |
265 |
| Strongyloides serology |
20 |
10.7 |
186 |
11 |
4.1 |
266 |
| Giardia lamblia (stools) |
0 |
0.0 |
51 |
17 |
6.5 |
261 |
| Dientamoeba fragilis (stools) |
5 |
9.8 |
51 |
23 |
8.8 |
261 |
| Chronic hepatitis B† |
10 |
2.2 |
455 |
|
|
|
| Hepatitis B immune (vaccination) |
25 |
13.4 |
187 |
165 |
61.6 |
268 |
| Micronutrient and vitamin deficiencies |
| Vitamin B12 deficiency (active vitamin B12 reference range: 0–30 pmol/L) |
| Females |
22 |
36.7 |
60 |
21 |
40.4 |
52 |
| Males |
16 |
22.5 |
71 |
25 |
31.6 |
79 |
| Vitamin D deficiency (vitamin D reference range: 0–49 nmol/L) |
| Mild (vitamin D reference range 30–49 nmol/L) |
| Females |
22 |
23.7 |
93 |
38 |
29.7 |
128 |
| Males |
39 |
41.9 |
93 |
53 |
38.4 |
138 |
| Moderate/severe (vitamin D reference range: <30 nmol/L) |
| Females |
52 |
55.9 |
93 |
50 |
39.1 |
128 |
| Males |
10 |
10.7 |
93 |
19 |
13.7 |
138 |
| Iron deficiency (adults – serum ferritin reference range: <30 uG/L; children – serum ferritin reference range: <20 uG/L) |
| Females |
60 |
64.5 |
93 |
49 |
38.0 |
129 |
| Males |
6 |
6.4 |
93 |
55 |
39.6 |
139 |
| Chronic disease |
| Total (includes cardiovascular disease, hypertension and chronic airways disease)‡ |
| Females |
25 |
26.9 |
93 |
|
|
|
| Males |
37 |
39.8 |
93 |
|
|
|
| Diabetes |
| Females |
1 |
1.07 |
93 |
|
|
|
| Males |
11 |
11.8 |
93 |
|
|
|
| Hypertension |
| Females |
12 |
12.9 |
93 |
|
|
|
| Males |
13 |
14.0 |
93 |
|
|
|
*Nova Lisa enzyme immunoassay; specificity >97%, sensitivity 87%
†Chronic hepatitis B data are reported for total population (combined adults and children) because of very small numbers within each subgroup.
‡Measured in adults only |
Micronutrient and vitamin deficiencies
Table 2 shows the relatively high prevalence of vitamin D, vitamin B12 and iron deficiency. Of the population of adult women, 64.5% were iron deficient (n = 48).
Chronic disease
In the adults, 39.7% of males and 26.9% of females had a chronic disease, including diabetes, hypertension, asthma, ischaemic heart disease and chronic obstructive pulmonary disease (Table 2). Results are based on the patient’s self-reported history, overseas medical documentation, prescribed medication and assessment in Australia.
Smoking and obesity are two of the risk factors for chronic disease. Forty (43.5%) Syrian men were smokers; 19 of these were reformed smokers. The prevalence of smoking was lower in women (Figure 1). The body mass index of Syrian adults showed 129 (72.1%) people were overweight or obese (Figure 2).
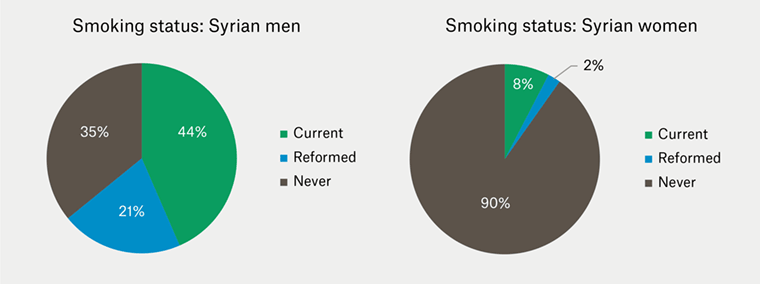
Figure 1. Smoking status of Syrian adults at the Refugee Health Service, 2016
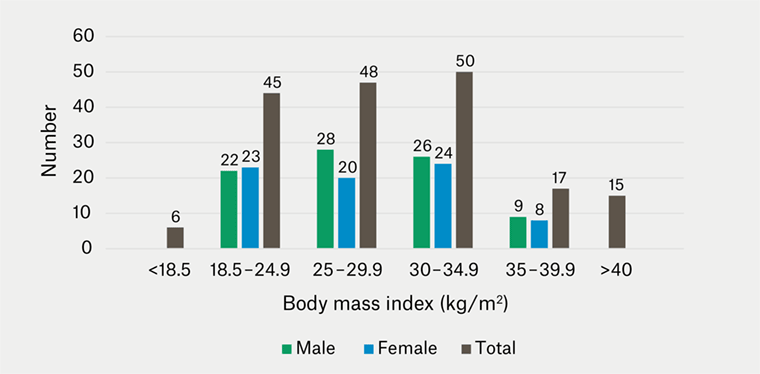
Figure 2. Body mass index of Syrian adults at the Refugee Health Service, 2016
*If n <5, individual frequencies are not reported.
Mental health and disability
Of the 178 adults assessed during the initial health assessment, 48 individuals (26.9%) reported symptoms such as anxiety, depressed mood and poor sleep. Of these, 38 individuals were referred for further assessment. Other commonly reported symptoms in adults included musculoskeletal pain (36.7%) and gastrointestinal (29.1%) complaints (abdominal pain, constipation, diarrhoea).
Seven children and nine adults (3.5%) had some form of disability secondary to previous injury or developmental abnormalities. All required specialist and/or allied health assessment.
Discussion
The findings of this study illustrate several key characteristics of the demographic and health profile of the new arrival Syrian refugees who attended RHS in 2016. The cohort was relatively young and predominantly consisted of large families. This reflects the population structure in Syria, where more than half are aged <24 years, and the Australian government’s commitment to prioritising vulnerable groups such as children, women and families for resettlement.26,27
Selected parasites and helminth infestations were detected in <10% of the cohort; however, direct comparisons cannot be made with existing data in the literature because of the variation in study populations. Schistosomiasis was treated on the basis of positive serology. Given the reasonably high sensitivity (87%) of the serological test, we are confident that most cases were correctly detected, and the very high specificity (>97%) indicates that very few cases were incorrectly diagnosed and treated. Findings for strongyloides were similar. Schistosomiasis and strongyloides were treated as per ASID/RHeaNA guidelines. These findings reinforce the continued need to test for these easily treatable diseases with potentially significant medical sequelae. The prevalence of chronic hepatitis B in this study cohort was half that previously reported for Syria.16,17
Significant proportions of the study cohort had vitamin and micronutrient deficiencies, which is likely consistent with previous studies identifying high rates of anaemia. Many people stated that food security was an issue during the period of displacement. Vitamin D deficiency is well documented in refugees; as expected, high rates of vitamin D deficiency were found in this cohort.
The study findings support previous reports of the burden of chronic disease in the Syrian population. Chronic disease risk factors such as smoking and overweight or obese body habitus were prevalent in the study cohort, in addition to conditions such as diabetes and hypertension. The mean age of adults with any form of chronic disease was comparable to the general Australian population at 45.6 years.28 Smoking was more prevalent in men in our study cohort when compared with country statistics for Syria – 43%, compared with 21.18%; whereas the proportion of female smokers was similar to that in Syria – 8%, compared with 8.5%.29 There were reports of interruption to medication supply and limited access to chronic disease follow-up prior to resettlement.
Screening for latent TB infection is conducted by the Chest Clinic in South Australia, thus not reported in this study. It should be noted that active TB is excluded by pre-departure screening, and children aged 2–10 years undergo latent TB testing prior to departure.
It is likely that the findings underestimated the burden of mental health issues. Anecdotally, many individuals have presented with mental health symptoms in the 3–12 months post-arrival. A combination of post-settlement stressors have an impact on presentations, including job-seeking obligations and attending English-language classes while having to fulfil family and carer responsibilities. Additionally, the trauma of escaping an acute war zone, separation and concern regarding safety of family and friends remaining in Syria, continued exposure to the ongoing Syrian crisis through the media and social media, and communication with relatives all contribute to significant mental health burden. These factors also affect children and adolescents; however, this was not within the scope of this study and warrants a separate study.
In terms of disability management, despite the small numbers, there were challenges in obtaining services and support. These were more promptly accessed for children as referral and diagnostic pathways for services catering to adults with disabilities are less clear. The phased rollout of the National Disability Insurance Scheme also contributed to difficulty accessing services at the time of the study.
This study had several limitations. Data collected was based on the initial appointment and up to three months post-arrival. Symptoms of mental distress were noted; however, a validated mental health screening tool was not used. This, along with the latency of these presentations, may not have accurately captured data on mental health issues or may have resulted in missed presentations.
Study findings are not strongly generalisable to the Syrian population given that the settlement service provider allocates those with more complex health and social needs to receive primary healthcare at RHS. Nevertheless, the large sample size and few missing data for each variable examined produced robust estimations of prevalence of selected health conditions, adding to existing knowledge on the health profile of this population.
Conclusion and implications for general practice
Study findings are consistent with the transitioning burden of disease from communicable to non-communicable and chronic diseases in the Syrian population.
The results highlight the importance of comprehensive health screening for new arrivals of refugee background in line with ASID/RHeaNA recommendations. It is recommended that health screening includes screening for infectious disease, nutritional and vitamin deficiencies and chronic disease. Further studies are needed to look at mental health screening in new arrival refugees. It is recommended that health professionals are aware of the evolving nature of psychological distress, which often results from a combination of the trauma of escaping an acute conflict area and the stressors unique to resettlement. This warrants ongoing monitoring and early identification to allow for prompt intervention.