Abstract
Two patients had suspicious pigmented lesions that were partially punch biopsied by their primary care physicians, resulting in sampling error and subsequent pathology misdiagnosis. These cases emphasise that an excision biopsy with a 2 mm margin is recommended as the standard biopsy technique used for suspicious pigmented lesions. Punch biopsies are best avoided. Situations in which standard excisions may not be practical, and the alternative options available, are also discussed.
Case 1
A man aged 68 years was referred for assessment of a 2 cm pigmented lesion, of unknown duration, in the left preauricular region (Figure 1). Punch biopsy of the lesion, performed by the primary general practitioner, identified it was a solar lentiginous naevus.
Pathologic examination revealed melanocytes with mild atypia and without any pagetoid upward spread. However, dermoscopic examination of the lesion showed a chaotic pattern and thick reticular lines as well as a grey hue in the centre, suggestive of a melanoma (Figure 2). A standard excision biopsy with 2 mm margins was performed, which identified a superficial spreading malignant melanoma with a Breslow thickness of 0.3 mm and an associated Clark scale of Level 2. The tumour arose in a pre-existing superficial spreading melanoma in situ with areas of dysplastic naevus.

Figure 1. Clinically suspicious pigmented lesion in the left preauricular region. Note evidence of recent punch biopsies.
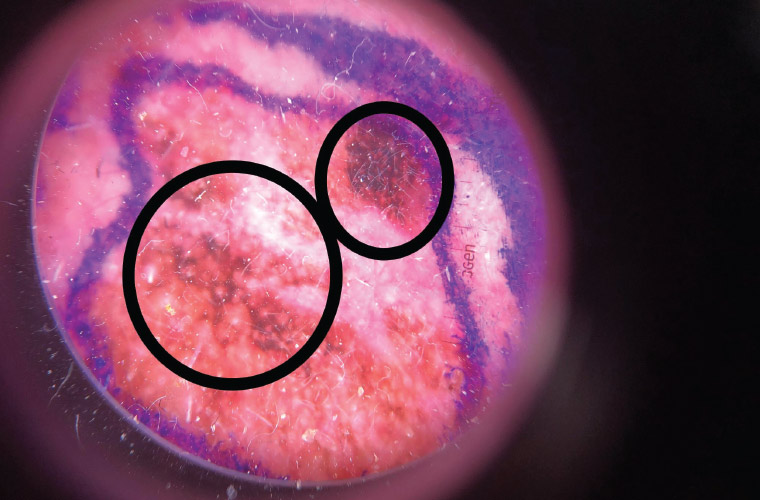
Figure 2. Dermoscopic examination showing a chaotic lesion with thickened network
Case 2
A man aged 72 years was referred for removal of several large basal cell carcinomas from his dorsal trunk. During a skin examination, a suspicious pigmented lesion that had previously been punch biopsied by the general practitioner was noted on his right scapula (Figure 3). Initial pathologic assessment and diagnosis identified it was a junctional naevus that showed a moderate degree of junctional dysplasia. However, because dermoscopic examination of the lesion revealed a chaotic pattern with a segmental thickened network – a clue for malignant melanoma – we performed a standard excision biopsy with 2 mm margins. This revealed a melanoma in situ of lentigo maligna subtype arising in a moderately dysplastic compound naevus.

Figure 3. Clinically suspicious pigmented lesion in the right scapula region. Note evidence of partial punch biopsy.
Discussion
Various guidelines recommend excisional biopsy for suspicious pigmented lesions. Partial biopsy, particularly punch biopsy, risks sampling error as areas of invasive melanoma, otherwise present in a standard excisional biopsy, might be missed.1 In addition, it should be noted that contiguous but histologically different pigmented lesions are commonly seen, and sampling of a benign lesion can lead to misdiagnosis.1
Many melanocytic lesions display heterogeneous histological appearance. There is an associated component of melanocytic naevus in 20–60% of melanomas.2 A partial biopsy may show areas of conventional or dysplastic naevus, while other areas with an evolving melanoma might be missed and not represented in the biopsy sample.2
Punch biopsy is associated with an increased risk of melanoma under-diagnosis. In a study by Ng et al comparing melanoma biopsy methods, the odds ratio for melanoma misdiagnosis with punch biopsy was 16.6 when compared with excisional biopsy.3 The false-negative diagnosis rates for punch, shave and excisional biopsies were 23.3%, 4.5% and 1.7%, respectively.3
According to the clinical practice guidelines for management of melanoma in Australia and New Zealand, excisional biopsy with a narrow clinical margin of 2 mm is the standard approach for clinically suspicious pigmented lesions.4
In conclusion, partial punch biopsy is a poor diagnostic modality for clinically suspicious pigmented lesions. Because this technique samples only a limited section of the pigmented lesion, it is prone to sampling and diagnostic errors. Furthermore, punch biopsy may not provide sufficient tissue, making accurate interpretation difficult for a pathologist, even when the area of melanoma has been appropriately targeted. Hence, punch biopsy is best avoided if there is any possibility of melanoma because of its increased risk of false-negative results. Excisional biopsy with 2 mm margins is the optimal method of biopsy for suspicious pigmented lesions.
In some cases, complete excision of a lesion may not be practical. This includes large lesions, those in difficult locations, or those in cosmetically sensitive areas, such as the face. In these situations, shave biopsy could be considered to avoid deformity and potential cosmetic disfiguration due to excision of lesions that may ultimately be identified as benign. However, it is still critical to ensure an adequate sample has been taken. Dermoscopic assessment or confocal microscopy is recommended to select the appropriate area for biopsy; it is important not to perform a blind partial biopsy. If in doubt, consider referral to a specialist dermatologist.