Case
An otherwise healthy man aged 31 years presented after returning two weeks earlier from a 10-day holiday in Bali, Indonesia. Five days ago he developed subjective fevers, generalised arthralgia, fatigue, vomiting, diarrhoea and a headache. He also had a few days of retro-orbital pain, which resolved prior to his appointment with the general practitioner. On the day of his appointment, he noticed a rash covering his torso and limbs. He did not receive any vaccinations or malaria prophylaxis prior to travel. There was no sexual contact or intravenous drug use during his holiday.
On examination he was afebrile and there were no remarkable findings except the reported rash (Figure 1). Urgent investigations showed normal haemoglobin and haematocrit; mild neutropenia (2.8 × 109 cells/L), lymphopenia (0.96 × 109 cells/L) and thrombocytopenia (121 × 109 cells/L); mild transaminases derangement and an elevated C-reactive protein of 13 mg/L.

Figure 1. The fine macular rash covering the torso and limbs
Question 1
Besides dengue, what differentials need to be considered in a returned traveller from South-East Asia?
Question 2
What is the epidemiology of dengue in Australia?
Answer 1
Dengue is the most common cause of fever in returned travellers from South-East Asia.1 Other causes of fever accompanied by rash include chikungunya, zika, rickettsial infections, measles, acute human immunodeficiency virus infection and enteric fever.2 Malaria needs to be excluded in patients who are febrile. Viral hepatitis, influenza, infectious mononucleosis and locally acquired Ross River virus and Barmah Forest virus are also important differentials.
Answer 2
Dengue virus is not endemic in Australia.3 Imported cases are reported in all states and territories.4 The primary mosquito vector Aedes aegypti is limited to northern Queensland, where yearly outbreaks occur because of vector spread from imported index cases.3 There were 1030 confirmed cases in 2017.5
Travel to Indonesia is associated with the highest risk when compared with all other destinations, with peak acquisition occurring between December and April.4,6
Case continued
The patient’s initial serology results were:
- dengue non-structural protein 1 (NS1) antigen: positive
- dengue groups 1–4 immunoglobulin (Ig) M: positive
- dengue groups 1–4 IgG: negative.
Chikungunya alphavirus IgM was positive but failed to demonstrate a rise in IgG over two weeks. Malaria DNA amplification and serologies for hepatitis A and B were negative.
The patient improved clinically with conservative management. Thrombocytopenia deteriorated slightly to 97 × 109 cells/L and the transaminases increased significantly, both recovering spontaneously on repeat testings.
Repeat dengue groups 1–4 IgG serology was positive after two weeks, consistent with primary dengue infection.
Question 3
What is the natural history of dengue?
Question 4
How is the diagnosis of dengue confirmed?
Question 5
How should dengue be managed in a primary setting?
Answer 3
Dengue infections can be asymptomatic.7 In significantly symptomatic patients there is an incubation period of 3–10 days after the bite, followed by one of the two main forms.8
Non-severe dengue is self-limiting and characterised by sudden onset high fever usually lasting 5–7 days, with constitutional symptoms and occasional haemorrhagic manifestations.
Severe dengue is less common in Australia as it is associated with repeated infections by different serotypes.6,9 It is characterised by abnormal haemostasis and plasma leakage, typically commencing on day 4–5 of illness, after the fever defervesces (Figure 2). Warning signs include severe abdominal pain, persistent vomiting, lethargy or restlessness, hepatomegaly, reduced oral intake, oliguria, postural hypotension and mucosal bleeding. Laboratory findings include increased haematocrit and concurrent rapid decrease in platelet count.
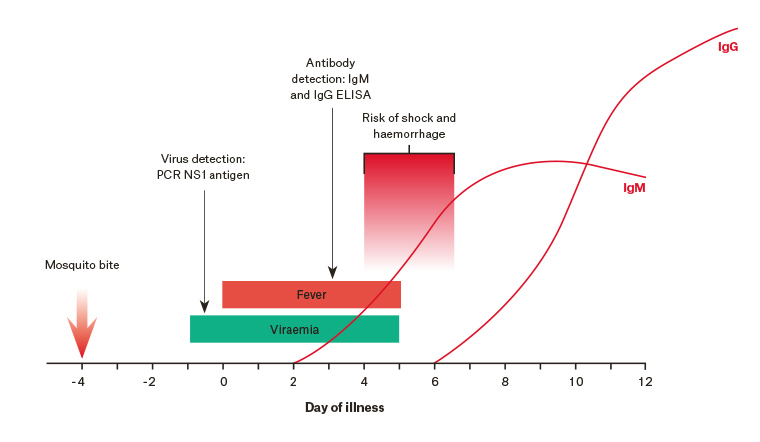
Figure 2. Timing of serology tests and high-risk period in primary dengue
Reproduced with permission from Queensland Dengue Management Plan 2015–2020, Queensland Health.9
ELISA, enzyme-linked immunosorbent assay; Ig, immunoglobulin; NS1, non-structural protein 1; PCR, polymerase chain reaction
Answer 4
The serum viral RNA polymerase chain reaction (PCR) is sensitive and specific within days 1–5 of symptom onset, after which it becomes negative. Similarly, the NS1 viral antigen is detectable up to day nine. The preferred test may vary between pathology providers.
Dengue IgM is detectable from day six of illness, and IgG from day eight. Cross-reactivity with other viruses such as chikungunya can occur, and paired samples taken 10–14 days apart may be required to confirm IgG seroconversion.9
Dates of travel and symptom onset should be clearly noted on the serology request form to aid interpretation.3
Answer 5
Prompt notification to the local public health unit is mandated on probable or confirmed diagnosis.10 In tropical north Queensland in particular, urgent household and community prevention measures may be required, with patients advised to stay indoors and the household recommended to use insect repellent.3
Treatment for dengue is supportive. Patients without clinical warning signs and a near normal blood count can be treated as an outpatient with oral rehydration and paracetamol. Non-steroidal anti-inflammatory medicines are not recommended because of the risk of increased bleeding.8 Patients should be provided with oral and written instructions to attend hospital if the warning signs of severe dengue occur, or symptoms fail to improve during transition to the afebrile phase. Guidelines suggest daily clinical review and blood count until the critical period passes.8,11
It is recommended that patients with warning signs or risk factors such as pregnancy, chronic medical conditions and extremities of age be admitted to hospital for observation and consideration of intravenous fluid replacement.8,11
Key points
- Dengue is a common cause of fever and rash in returned travellers from South-East Asia.
- NS1 antigen or PCR assay is valuable early in the course of illness; if negative or baseline IgM is positive, convalescent serology may be useful to confirm IgG seroconversion.
- Management is conservative, with an emphasis on patient education regarding warning signs, close monitoring and public health measures.
- Patients with comorbidities, difficult social circumstances or warning signs for severe dengue should be referred to hospital.