Case
A man aged 60 years collapsed at home following a short illness characterised by severe vomiting. His heart rate was 30 beats per minute (bpm) and blood pressure was 110/80 mmHg at his residence. He had no chest pain and was not febrile. He was transferred urgently to an emergency department (ED). His electrocardiograph (ECG) on arrival is shown in Figure 1.
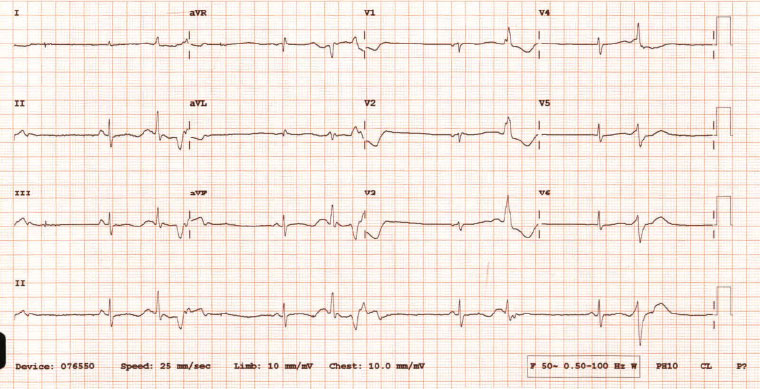
Figure 1. Patient electrocardiograph on arrival at emergency department
Question 1
What abnormalities can be seen in the patient’s ECG?
Question 2
What further patient history should be obtained?
Answer 1
The patient’s ECG reveals:
- absolute QT interval prolongation of 600 ms
- bradycardia
- R on T phenomena, where QRS complexes are falling close to the T wave with the risk of initiation of ventricular arrhythmia.
Answer 2
The patient’s past medical history, current medications and events leading up to his deterioration should be considered. If available, older ECGs should be checked to determine if this is congenital or acquired prolonged QT.
Case continued
The ECG rhythm strip (Figure 2) revealed polymorphic ventricular tachycardia or torsades de pointes (TdP). The patient’s regular medications included methadone 30 mg twice daily as long-term opioid substitution therapy (OST). Weight loss had led to consultation with a naturopath, and initiation of supplements containing liquorice and silymarin seven weeks prior to presentation. Fluconazole was also commenced following general practitioner (GP) consultation for severe tongue pain with an accompanying clinical diagnosis of oral candida. After limited treatment response, fluconazole dose was doubled to 200 mg daily four weeks prior to presentation. Ear, nose and throat specialist consultation on the day of ED presentation had led to a diagnosis of inoperable squamous cell cancer of the tongue, and initiation of oxycodone as analgesia. Severe vomiting began within an hour of the first dose of 20 mg oxycodone. On arrival in the ED, the patient’s electrolytes were normal (K 4.3 mmol/L, Mg 0.74 mmol/L, Ca 2.49 mmol/L).
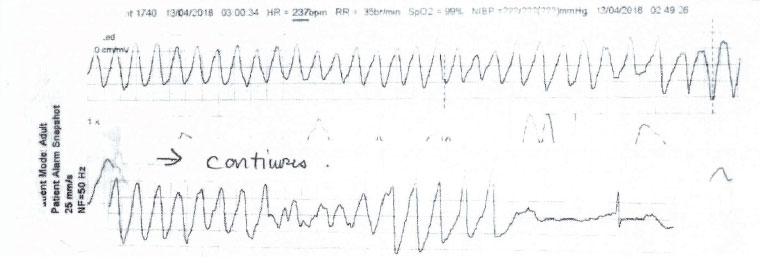
Figure 2. Electrocardiograph rhythm strip from ambulance
Question 3
How do this patient’s medications increase the likelihood of clinically significant QT prolongation?
Question 4
Why does methadone metabolism vary over time and between patients?
Question 5
How prevalent is methadone use?
Question 6
What is the acute management of TdP?
Question 7
How can GPs help patients avoid dangerous interactions?
Answer 3
The association between methadone use and QT interval prolongation is well documented.1 Methadone is largely metabolised by hepatic cytochrome P450 3A4, which is inhibited by liquorice, silymarin and fluconazole, potentially leading to increased serum methadone concentration.2,3 Oxycodone has also been documented to prolong QT interval duration.4 Medications that prolong the QT interval and other concurrent factors (bradycardia, hypokalemia, hypomagnesemia) can put individuals at increased risk of TdP.
Answer 4
The pharmacokinetics of methadone can vary significantly between individuals as a result of significant genetic polymorphisms within DNA encoding these enzymes. CYP 3A4 activity can vary up to 30-fold among individuals. A wide spectrum of medications can inhibit or induce CYP 3A4 activity, leading to variable methadone serum concentration. Many common medications used in cancer treatments can prolong QT interval, including anthracyclines, alkylating drugs and cisplatin, as well as antiemetics, including ondansetron.3
Answer 5
Methadone has been used to treat opiate dependence for many decades in Australia. In 2015, nearly 50,000 people, including those who inject drugs as well as those who are dependent on opiates for chronic non-cancer pain, were using pharmacotherapy for opiate dependence. Of these people, two-thirds were receiving methadone.5 Methadone has reduced mortality among these patients,6 such that they are becoming an older population who are developing comorbidities, including cancer. Hence, patients on methadone are increasingly encountering clinicians other than their primary methadone prescriber.
Answer 6
Management of TdP in patients with preserved perfusion requires intravenous administration of magnesium sulfate to stabilise the cardiac membrane. Pharmacological or electrical cardiac pacing is used to maintain a heart rate >80 bpm, thus reducing R-R interval and the incidence of R on T phenomena causing further TdP. Serum potassium, calcium and magnesium are maintained within normal limits.
Answer 7
Patients with chronic disease, multiple comorbidities and cancer often encounter multiple clinicians and alternative health practitioners during the course of their illness. It is critical that clinicians ensure a thorough medication history is obtained that includes prescribed, over-the-counter and complementary therapies. Information is readily available to clinicians through online resources including the Australian Medicines Handbook. The Natural Medicines Database details evidence-based information regarding drug interactions and mechanisms of action of complementary and over-the-counter preparations.
Summary
- Methadone has been prescribed for OST for many decades in Australia. The concurrent ageing of patients on OST means many are developing comorbidities requiring additional medications. Methadone is associated with QT interval prolongation (and the risk of life-threatening arrhythmias), which may be exacerbated by the introduction of new medications.
- Online databases can assist clinicians to identify and avoid potential drug interactions.