This article presents some of the more recent evidence for the identification and management of idiopathic frozen shoulder in the primary care setting. The majority of patients with shoulder pain are seen and treated in primary care settings,1 placing the primary care physician in a pivotal role for the diagnosis and management of this condition.
Epidemiology
Shoulder pain, aching or stiffness is a daily problem for almost a quarter of the Australian population.2 Of those who have shoulder pain, aching or stiffness, there is a significant proportion who have recognised risk factors that predispose them to idiopathic frozen shoulder, such as diabetes, thyroid dysfunction, hypercholesterolaemia and hypertension.3 Frozen shoulder is thought to have an incidence of 3–5% in the general population and up to 20% in individuals with diabetes.4 The peak age is 56 years, and the condition occurs slightly more often in women than men.5 It is a rare diagnosis before the age of 35 years and is unusual in patients aged over 70 years.5,6
What is frozen shoulder?
Idiopathic, or primary, frozen shoulder is defined as ‘a condition characterized by functional restriction of both active and passive shoulder motion for which radiographs of the glenohumeral joint are essentially unremarkable except for the possible presence of osteopenia or calcific tendonitis’;7 the osteopenia results from limb and shoulder disuse. Primary frozen shoulder is a specific condition with an International Classification of Diseases, 10th Revision, code of M75.0; its aetiology is unclear,8 and it requires a management plan very different from other shoulder conditions such as osteoarthritis, rotator cuff pathology and subacromial bursitis.8
In line with many other shoulder conditions, a symptom of frozen shoulder is pain; however, it differs in that it also has mechanical restriction in all planes of movement of the glenohumeral joint. The limitation is due to glenohumeral capsular tightness and restriction without any evidence of adhesions. It occurs when the capsule, or the soft tissue envelope, becomes scarred and contracted, making the shoulder tight, painful and stiff.9
What is the natural history?
It is a general belief that frozen shoulder resolves spontaneously after 1–3 years,9 although there is a paucity of long-term follow up data to support this.10 Up to 40% of patients may have persistent symptoms, with 7–15% having some degree of permanent loss of movement.6,11 On the basis of a study of patients with frozen shoulder with a mean follow-up of 4.4 years, only 59% of patients had normal or near-normal shoulders as defined by no or minimal symptoms.6 Another study with a mean follow-up of seven years showed 50% of patients still had some mild pain and 60% had some ongoing stiffness.12 Subsequently, the potential chronicity of this problem is a burden to the patient and also a considerable cost to society in terms of health dollars,13 lost productivity and quality of life.
Should investigations be performed for frozen shoulder?
Frozen shoulder is predominantly a clinical diagnosis.8 Most imaging modalities and pathology testing that aim to confirm the diagnosis are usually unhelpful and may result in the wrong diagnosis being made.8,14 Investigations performed to exclude other pathologies may only occasionally be indicated, although the finding of a serious alternative diagnosis is rare.15
Once a diagnosis of frozen shoulder is made, it may be appropriate, with certain patient groups, to exclude the possibility of other conditions such as diabetes, thyroid dysfunction, hypercholesterolaemia and hypertension for which there is an increased incidence of idiopathic frozen shoulder.3
The focused history
Given that frozen shoulder is a clinical diagnosis, having a standardised and systematic focused history and focused examination strategy will be of significant advantage in differentiating frozen shoulder from other shoulder pathologies.16
Having a structured approach using appropriate questions is essential.16 Box 1 is an example of a suggested format to help rule in frozen shoulder and rule out alternative pathologies.
| Box 1. Focused pain history for frozen shoulder |
Onset: The pain of idiopathic frozen shoulder is insidious, and there is no history of trauma.
Location: Frozen shoulder pain is classically perceived around the region of deltoid insertion.
Duration: The pain associated with frozen shoulder is persistent and may be chronic.
Character: The pain associated with frozen shoulder is most often dull and aching.
Aggravating and relieving factors: Pain is often worse at night and with extremes of movement; nonsteroidal anti-inflammatory drugs are often ineffective.
Radiation: Pain may radiate down the arm but rarely passes beyond the elbow.
Timing: Pain is variable depending on the phase, although it may persist longer than four years.
Severity: Pain is often severe in phase one and varies throughout the phases, progressively decreasing (although pain may not completely resolve). Using a visual analogue scale is useful to determine progress and as a baseline. |
The patient presenting with idiopathic frozen shoulder is characterised by the spontaneous onset of pain with significant restriction of both active and passive range of movement of the shoulder.8 Confirming that external rotation is not possible with both active and passive movement is important in making the diagnosis. A key element in making the correct diagnosis is being able to differentiate limitation of shoulder movement secondary to pain, which is very common in most musculoskeletal conditions, versus limitation secondary to actual physical or mechanical restrictions. Differentiating between the two may be best achieved by performing passive movement of the glenohumeral joint. Limitation secondary to pain will be volunteered by the patient. Limitation due to capsular restriction will be felt by the examiner and patient, usually in the absence of pain. Missing this very subtle yet important difference is a clinical pitfall and is likely to result in overdiagnosis and misdiagnosis17 and subsequently an incorrect management plan.
Identifying how pain and disability from this condition affects the patient is important in helping to evaluate the patient’s priorities, status, progress and outcome. Subsequently, as part of the focused history, the patient should be requested to perform the Shoulder Pain and Disability Index (SPADI; Appendix 1, available online; also available from most state and territory WorkSafe departments).18,19 The SPADI is a common and accepted assessment tool for shoulder function and pain and is used by many workers’ compensation assessment authorities and rehabilitation services within Australia; therefore, familiarity by the primary care physician is a benefit.
Clinical presentation classically occurs in one of three overlapping phases (Table 1),8,14 and therefore the primary symptoms may vary depending on the phase of presentation.
| Table 1. Clinical phases of frozen shoulder (each phase is overlapping)* |
| Clinical phase |
Description |
Clinical details |
| Phase one |
Painful phase or pain-predominant phase |
- Lasts 2–9 months
- Progressive stiffening and increasing pain on movement and at night
- No history of shoulder trauma
|
| Phase two |
Stiffening, freezing or stiffness predominant phase |
- Lasts 4–12 months
- Gradual reduction of pain but stiffness persists with considerable restriction in range of motion
- Pain gradually subsides but stiffness remains
- Pain may be apparent only at the extremes
of movement
- Gross reduction of glenohumeral movements, with near total obliteration of external rotation
|
| Phase three |
Resolution or thawing phase |
- Lasts 12–42 months
- Variable improvement in range of motion with resolution of stiffness
|
| *Time frames are approximations and all phases overlap by varying degrees. |
The focused examination
As with the focused history, having a standardised and systematic approach to shoulder examination ensures accuracy in assessment and final diagnosis.16 It is important to be able to identify anatomical landmarks and appreciate both anatomical planes and ranges of movement for the shoulder joint.16 The focused shoulder examination involves the principles of inspection, palpation, movement and measuring (Table 2).5,7,8,16,20
| Table 2. Frozen shoulder examination findings |
| Investigation |
Examination findings |
| Inspection |
- Mild disuse atrophy of the deltoid and supraspinatus may be present.
- It is a normal finding for the dominant shoulder to sit lower than the non-dominant shoulder, subsequently this in itself is not necessarily a pathological finding.
|
| Palpation |
- There may be diffuse tenderness over the glenohumeral joint, which may extend to the trapezius and interscapular region; this is secondary to splinting of the painful shoulder.
- For the musculoskeletal system, pain is poorly localised yet tenderness is well localised, hence the patient has a perceived location of pain at or around the deltoid insertion, yet tenderness is identified over the glenohumeral joint.
|
| Movement and measuring |
- This stage should be performed simultaneously using the unaffected shoulder as the control for normal power and normal range of movement.
- It is at this stage of the examination that limitation of range of movement secondary to mechanical block rather than pain is differentiated.
- With suspected frozen shoulder, both active and passive movements must be performed.
- The pathognomonic sign of frozen shoulder is almost complete loss of active and passive external rotation.
- Limitation to active and passive abduction, forward flexion and/or internal rotation may also be found.
|
The pathognomonic sign of frozen shoulder is almost complete loss of active and passive external rotation.8,20 As mentioned previously, it is essential to be able to differentiate between limited range of movement secondary to a mechanical block due to glenohumeral capsular tightness and restriction, and limitation secondary to pain.
Management principles
Only the conservative management principles of idiopathic frozen shoulder will be discussed in this article, as conservative management is the mainstay in the majority of cases, with surgery reserved for the most refractory.8
Each phase of frozen shoulder is managed differently and is dependent on the predominant signs and symptoms. There are four key management principles that overlap into all phases (Box 2), albeit the emphasis of each will vary depending on the phase.
Patient education regarding the natural history of the condition and proposed management plan are important and should always be included as part of the management plan.8,13 Understanding how the patient is affected by the condition is essential when formulating a management plan, and applying the SPADI is strongly recommended.18,19 The SPADI provides a baseline of current pain and disability, therefore allowing a serial measure of progress and how the condition affects the patient’s quality of life and ability to work and function safely.
| Box 2. Conservative management principles |
- Education
- The nature of the condition
- The natural history
- The potential chronicity of the condition
- Regular and breakthrough analgesia
- Start with simple regular analgesia; care should be taken with regular and prolonged use of nonsteroidal anti-inflammatory drugs if these are used
- Supplement with stronger breakthrough analgesia
- Topical creams, lotions and ointments are ineffective, but their use may be reasonable if the patient perceives there is benefit and no harm is being done
- Physiotherapy
- Involve early
- Intervention strategies will vary depending on the phase
- Intra-articular corticosteroid injection
- More effective the earlier it is given
- Aseptic technique is necessary
- Accuracy can be ensured using anatomical landmarks or image guidance
- Other injection therapies
- Hydrodilatation has been shown to be effective and safe
- The addition of a small amount of local anaesthetic is beneficial
|
In all phases and indeed with all musculoskeletal conditions, optimising pain management is a priority. Without adequate and appropriate pain management, biomechanical changes occur secondary to guarding as a protective mechanism and altered limb use, which may result in muscle atrophy, osteopenia and tendinopathy.
Although patients may be reluctant to use appropriate analgesia, it is essential that analgesia is prescribed regularly, with the availability of alternative additional analgesia for breakthrough pain.8 The involvement of a physiotherapist who has experience in the management of frozen shoulder is essential in each phase of the condition.
Intra-articular corticosteroid injections are safe and effective and have been shown to hasten improvement in pain and function. Many studies show benefit either alone or in conjunction with physiotherapy and/or a home-based exercise program.8,10,21,22
Glenohumeral joint injection performed in the early stages of frozen shoulder by the primary care physician, with the necessary skills and equipment, can provide significant improvement in passive range of movement.8,23 Figure 1 identifies the anatomical landmarks required to ensure the injection is located within the glenohumeral joint. If any doubt exists, the image-guided approach should be performed.
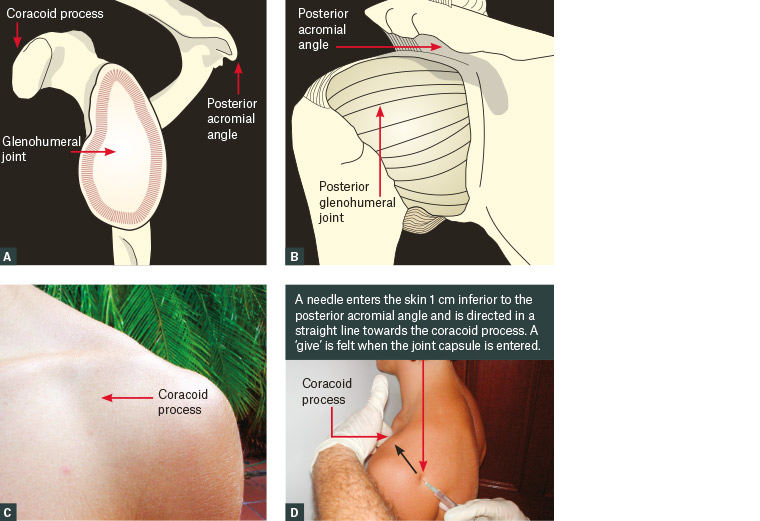
Figure 1. Anatomical landmarks for glenohumeral joint injection
A. Lateral view of glenohumeral joint with glenoid exposed; B. Posterior view of glenohumeral joint with capsule intact; C. Anatomical surface location of coracoid process; D. Surface anatomy depicting needle insertion point and direction with the glenohumeral joint being midway between posterior acromial angle and coracoid process
Another injection-therapy modality is hydrodilatation, which involves injecting the glenohumeral joint capsule with a mixture of sodium chloride (0.9%) and corticosteroid made up to a volume of 40 mL. This procedure results in stretching of the capsule in addition to providing the benefits of the injected steroid. The injection technique is the same as described previously.
Hydrodilatation has been shown to be effective when used alone or in combination with physiotherapy.10,17 The author has found the addition of 5–10 mL of 0.5% bupivacaine, included within the maximum volume of 40 mL, to be effective in providing short-term pain relief and allowing for pain-free physiotherapy and exercises following this procedure. Prior to the procedure taking place, the usual medication administration safeguards must be adhered to including checking for allergies, medication contraindications, medication side effects and dosage recommendations.
The use of intra-articular sodium hyaluronate has been assessed in several randomised controlled trials and has been shown not to be effective in frozen shoulder.22
The use of oral steroids has also been tested; to date, the benefits do not appear to outweigh the potential risk.22,24,25
Conclusion
Idiopathic frozen shoulder is a common presentation. It has three overlapping phases, each comprising pain, stiffness and limited range of movement in varying degrees. Pain and/or stiffness may become a chronic problem. To be able to differentiate between limited range of movement secondary to mechanical restriction and limited range of movement secondary to pain is an important principle. Most patients with idiopathic frozen shoulder are best managed conservatively. Involving a physiotherapist in the management plan is best practice. Appropriate oral analgesia is a mainstay of management. Intra-articular injections of the glenohumeral joint should always be considered in the early phases, especially if analgesia and physiotherapy are providing little-to-no benefit.
Appendix 1