Chronic non-cancer pain (CNCP) is commonplace and costly. In 2018, 3.24 million Australians were living with CNCP, costing the country $73.2 billion.1 In planning resource efficiency, it is noteworthy that CNCP often occurs in the midst of multimorbidity (Figure 1). A Scottish primary care study found that 23% of patients had multimorbidity and 46% of those presenting with CNCP had three or more long-term conditions.2
Metaflammation has been postulated as an underlying mechanism contributing to many chronic conditions.3 This may partly explain the overlap of effective lifestyle-based treatment strategies. For example, increasing physical activity improves multiple chronic conditions. There are potential efficiencies in generic lifestyle-based approaches to chronic conditions. Overinvesting in chronic condition–specific programs may lead to unintended inefficiencies and costs.
This article summarises current approaches to CNCP treatment and considers areas of specificity and overlap with generic chronic condition management (Figure 2).
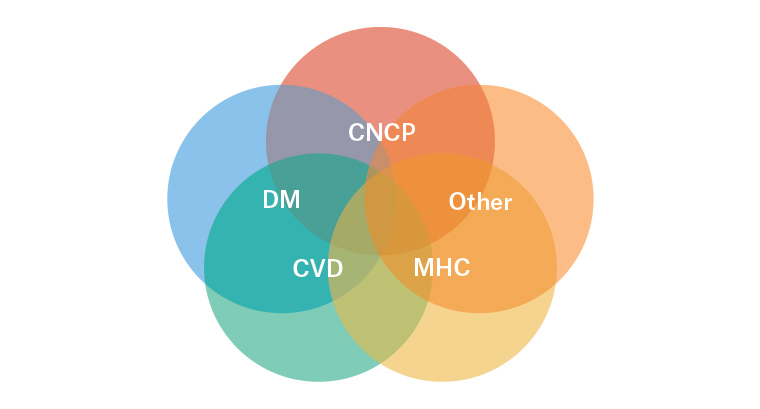
Figure 1. Conceptual illustration of the co‑occurrence of chronic conditions
CNCP, chronic non-cancer pain; CVD, cardiovascular disease; DM, diabetes mellitus; MHC, mental health conditions
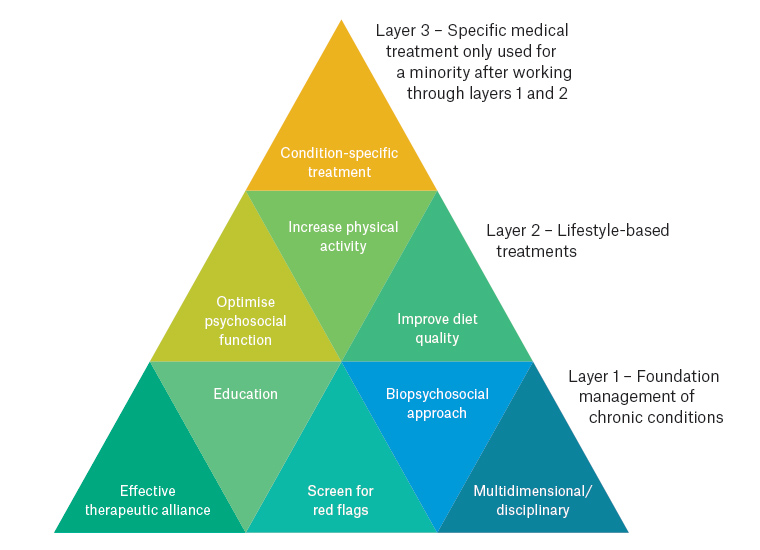
Figure 2. Reconceptualising chronic condition management: From broad to specific
Lessons from chronic pain management
A major lesson from CNCP is that a predominant focus on biomedical treatment is unlikely to be effective in the long term.4 ‘Red flag’ conditions need to be screened for, then treatment typically involves medication deprescription, or non-initiation, and transition to multidimensional supported self-management.5
In this transition, the relationship between health professional and patient is crucial. Empathy supports the therapeutic alliance, which is counterbalanced with therapeutic boundaries. ‘Connect’ first, then ‘redirect’ into evidence-based care.6
Targeted reassurance7 that ‘red flag’ conditions have been excluded and that the person is safe to move facilitates exit from often harmful and ineffective investigations, procedures and medications.
Patient education plays a central part in treating chronic conditions. In CNCP, an overview of nervous system plasticity informs patients that they can change their trajectory.8,9 Understanding that pain is generated by the brain, and that nervous system sensitisation can produce severe symptoms that are real but not generally due to structural issues, can be both confronting and liberating.9
Another lesson is that condition-specific services see only a small subgroup of patients. Only 0.2% of people experiencing CNCP are seen by specialist multidisciplinary pain services in any given year.10 A recent call to double these teams1 would allow only one extra patient per general practitioner (GP) per year to be seen. Therefore, there is a need to adapt specialised chronic condition treatment strategies for use in general practice. GPs can provide serial lifestyle-based care as well as refer selectively to multidisciplinary colleagues in primary care and condition-specific specialist services, including pain management teams, in a shared care model.
The biopsychosocial model provides a useful framework for treatment of all chronic conditions. The ‘whole person approach’ to CNCP is an application of this and consists of five components: biomedical, mind–body, connection, activity and nutrition.3 The biomedical component may be condition-specific. However, mind–body, connection, activity and nutrition components of treatment entail significant overlap and can be helpful across a range of chronic conditions. The challenge lies in appropriately weighting non-biomedical components of care. An overemphasis on passive biomedical treatment may undermine patient engagement with more active components.11
Biomedical
In CNCP, evidence for long-term effectiveness of biomedical monotherapies is lacking.4 There are exceptions, such as joint arthroplasty, but for many people, medications and interventional procedures are likely to produce more harm than benefit.
Previous guidelines recommended long-term opioids as a treatment for CNCP; however, this is no longer supported by the literature. In 2018, a 12-month randomised controlled trial compared opioid to non-opioid medication for chronic back, hip or knee pain.12 Patients in the opioid group reported more pain and more adverse effects. Another pivotal 2018 study found that after opioid discontinuation pain intensity either did not change or improved slightly.13 Therefore, the general rule is not to initiate opioids for CNCP and to consider deprescribing for patients who are already using opioids. Exceptions to this rule should be discussed with a pain medicine specialist. Some people with CNCP have comorbid opioid use disorder. In this case, maintenance opioid therapy via methadone program–like strategies can be considered in addition to psychosocial interventions.14
CNCP can present challenges in appropriately balancing biomedical treatment and lifestyle change. The same challenge is present for other chronic conditions, such as type 2 diabetes15 and hypertension16, as the harder fought and slower-onset lifestyle gains may be less motivating for patients than the faster gains of passively received medical treatments.
Mind–body
Many people with CNCP have heard the message ‘it’s all in your head’.9 This is invalidating and stems from an incorrect, yet widely held, mind–body dualism. To approach pain from a mind–body perspective can be sensitive ground. The belief that pain means something is damaged is instinctual and conditioned. The therapeutic challenge is to help the person recognise that mind, brain, nervous system and body are all linked, and that thoughts and emotions can profoundly influence pain.
For CNCP, strategies aim to wind down nervous system sensitivity. Multiple approaches have shown effectiveness, including cognitive behavioural therapy (CBT), mindfulness-based stress reduction (MBSR) and acceptance and commitment therapy,17 while emotional awareness and expression therapy and other embodied self-awareness practices show early promise.9,18 Much common ground exists in these approaches, with relaxation and breathing exercises, as well as targeted reassurance to address unhelpful cognitions, often valuable starting points.17,19
There is significant overlap in the psychological treatment of CNCP and other chronic conditions. Psychological strategies to enhance behaviour change and create healthy habits are applicable to any chronic condition. CBT has shown efficacy for a range of psychiatric disorders as well as irritable bowel syndrome and cancer pain, while MBSR has been shown to improve mental health of patients with a range of chronic illnesses.17
Connection
Emerging evidence suggests there is an overlap in neural pathways between physical and social pain.20 Social factors may contribute to CNCP through both focal traumatic events and chronic social stress.20 The experience of CNCP may then increase the frequency of social conflict and interpersonal stress.20 Many patients with chronic conditions can relate to isolation and a loss of connections.21 Connection includes having meaning and purpose in life, connecting with culture and engaging with people in many contexts. Research has shown that positive social connections are a predictor of general health.22
Restoring healthy connections can be a valuable intervention. Asking patients about who and what they feel connected to and supporting them to enhance meaningful social ties provides a collaborative and compassionate foundation for behaviour change.20,23 Group-based exercise programs and volunteering24 have shown benefits for emotional and physical health.
Activity
Physical activity is important in the prevention and treatment of many chronic conditions including CNCP. Pain is a commonly cited barrier to participation in physical activity. Understanding that pain in this context is not a sign of further tissue damage is crucial to feeling safe to undertake continued activity despite pain. Regular planned physical activity results in long-term adaptations leading to hypoalgesia via activation of opioid, serotonin and other mechanisms,25 as well as improved physical function.26
No single type of physical activity has proven to be superior, both in CNCP and chronic conditions generally.27,28 Walking is free, accessible and functional and should arguably be the default. However other forms of exercise may be more appropriate depending on patient preference – the best type of exercise is the one that is done. Incorporating strategies to increase adherence, such as positive reinforcement and feedback, is important.29
For all chronic conditions, the dose recommended is 150–300 minutes of moderate physical activity per week.30 However, as it is important that physical activity is carried out regularly and indefinitely, the volume of physical activity must be sustainable. For people with CNCP, ‘starting low and going slow’ can be helpful. Activity can then be gradually increased on a time-contingent basis. This avoids both the instinctual ‘boom and bust’ and ‘let pain be your guide’ approaches, instead aiming to increase function.
Strength-based exercise is also important for many chronic conditions. Guidelines recommend strength exercises at least twice per week.30 Sit-to-stand training is an accessible and functional way to build leg strength. It is easy to assess with the five-times-sit-to-stand test, with those taking longer than 15 seconds at high risk of recurrent falls.31
Nutrition
Globally, poor diet is the leading cause of mortality and top modifiable risk factor for morbidity.32 Both chronic conditions and CNCP share relationships with elevated weight status and poor diet quality.32
The role of nutrition in CNCP overlaps with generic chronic condition management. Optimising dietary intake enhances the function of nervous, immune and endocrine systems, with a direct effect on the pain experience33 and other conditions. A focus on weight loss can be beneficial to reduce load on joints and metaflammation.
The Australian Guide to Healthy Eating focuses on vegetables, fruits, legumes, nuts/seeds, low glycaemic index, high fibre, antioxidants and high-quality fats.34 It is also important to reduce consumption of energy-dense, nutrient-poor foods.
A recent systematic review investigating nutritional interventions for CNCP33 showed that all nutrition interventions were associated with significant pain reduction.
Motivators and barriers that influence eating behaviour should also be considered. There may be increased consumption through comfort eating or reliance on convenience foods, or, alternatively, restrictive eating patterns.
GPs are well positioned to provide messages centred on the Australian Guide to Healthy Eating34 that will benefit multiple chronic conditions.29
Conclusion
The contemporary treatment of CNCP incorporates some condition-specific approaches but there is much overlap with the treatment of other chronic conditions. From a health system perspective, there is value in reconceptualising chronic condition management and expanding generic chronic condition lifestyle interventions in primary care. The place of specialist multidisciplinary condition-specific programs then needs to be re-evaluated and referral criteria tightly defined.
Key points
- CNCP frequently occurs amid multimorbidity.
- Treatment strategies for many chronic conditions overlap (eg increase physical activity).
- There is potential gain in system efficiency and treatment outcomes by investing in generic lifestyle-based management applied across conditions.