Asthma is a major public health concern, affecting an estimated 4.3–8.6% of adults globally, and prevalence in Australia (21.0%) is among the highest in the world.1 Asthma was added as one of Australia’s National Health Priority Areas in 1999, reflecting the magnitude of the problem. Despite the introduction of a range of initiatives designed to improve asthma care over the past 20 years, it continues to be a major source of health, social and economic burden. In 2015, the total cost of asthma to Australia was $27.9 billion, with the largest portion of this cost attributable to the burden of disease experienced by those living with the condition.2 Asthma remains a significant contributor to morbidity and mortality in Australia, and accounted for almost 40,000 hospital separations and 421 deaths in Australia in 2015–16.3
National guidelines in Australia,4 and internationally,5–7 recommend that all patients with asthma have a current asthma management plan. This recommendation is provided in the context of the more general principle that tools and support for self-management be provided to all patients with asthma, including, but not limited to, a written asthma action plan, which should be reviewed at least annually.4 The National Asthma Council Australia handbook recommends offering self-management support appropriate to the person’s preferences and suggests ‘text message reminders’ as an example.4 Recommendations regarding asthma action plans are supported by evidence linking their use with reductions in asthma symptoms, decreased mortality from asthma, and improved quality of life.8,9 Although limitations in clinical trial design and reporting have contributed to the current paucity of robust evidence for effects on specific clinical outcomes,10 asthma action plans remain a cornerstone of current best-practice management. Despite this, only 21% of patients with asthma in Australia have a current asthma management plan, and this proportion falls to just 14% when paediatric patients are excluded.11
The recent National Review of Asthma Deaths (UK) reported that only 23% of those who died from asthma had a personalised asthma management plan; moreover, less than half had attended an asthma review in the year before their deaths.5 The report has substantial implications for healthcare professionals working in primary care, and highlights once again the crucial importance of engaging with patients opportunistically to ensure asthma care needs are appropriately addressed.12
Mobile health has been proposed as a way to increase communication and engagement in healthcare delivery.13 There is growing evidence that mobile-based reminders and interventions may be useful in a variety of health behaviour contexts, from medication adherence in cardiovascular disease,14 to contraception use15 and smoking cessation.16 To our knowledge, however, the only published studies to date that have examined the use of SMS technology in asthma management have been limited to evaluations of the use of SMS technology for improving asthma medication use17 and reducing appointments.18 The use of SMS to improve patient recall in the adult asthma management context has yet to be tested.
The aim of this study was to test the effect of SMS reminders for active patients with asthma who do not have a current asthma action plan, by sending an SMS prompt to attend their usual family practice clinic for an asthma review. Specifically, we hypothesised that a greater proportion of the intervention group would have 1) a written asthma plan and 2) spirometry completed during the study follow-up period, compared with the control group.
Methods
A randomised controlled trial study design was used. Ethics clearance was obtained from The University of Queensland Medical Research Ethics Committee (#2015001477). This trial was conducted in a suburban Brisbane general practice servicing a standardised whole patient equivalent population of 8225 patients. The practice employs 7.8 full-time equivalent (FTE) general practitioners (GPs), and is larger than the average Australian general practice (5.5 FTE GPs).19 The Socio-Economic Indexes for Areas (SEIFA) index for the suburb places it at the 51st centile, close to the mean for economic disadvantage in Australia,20 and the demographics of the local population are similar to those of the broader Australian population in terms of sex, age, income, employment and proportion of Aboriginal and Torres Strait Islander residents.21
Recruitment took place from May to July, 2016. The primary care patient database was interrogated for eligible patients based on a previous diagnosis of asthma and no current asthma management plan. Patients were eligible to participate if they 1) had asthma recorded as a diagnosis in their active past history, 2) were active patients of the practice (defined as attending at least twice in the past two years), 3) were aged ≥18 years, 4) had not had an asthma management plan completed in the preceding 12 months, 5) had a mobile phone number attached to their clinic record and 6) had previously consented to receive SMS reminders from the practice.
Procedure
Eligible patients were mailed detailed written study information, a consent form and a reply-paid envelope, and were directed to complete and return the consent form if they wished to participate. An SMS reminder, followed by a phone call, were used to contact non-responders after two and four weeks, respectively, to assess willingness to participate and obtain written consent. Fully automated participant randomisation was performed by purpose-designed computer software (Reminder Plus, Literra Health), which used a random-number generator to achieve simple randomisation without stratification, randomly allocating participants to either the intervention or control group and ensuring the researchers who assessed the outcomes and analysed the data (BLM, JC, AEM) remained blinded to group allocation. The software was also used to send the automated SMS reminders to participants allocated to the intervention group while preserving researcher blinding. Only once data analysis was complete were the data unmasked by investigators.
Intervention
Approximately 30 days after enrolment, patients in the intervention group were sent a brief SMS:
‘Hello. The doctors at [Name] Clinic have recommended that you attend for an asthma health check & management plan. Please phone [contact number] to arrange your appointment. With kind thanks, [Name] Clinic.’
A second SMS was automatically sent four weeks later to the intervention group participants who had not yet made an appointment. The control group received care as usual, which may have included opportunistic asthma care. Following usual clinic practice, patients in either group who specifically requested an appointment for asthma care were seen by a practice nurse in the dedicated asthma clinic as well as by a GP, whereas patients who booked an appointment without citing a reason were given an appointment only with their GPs, who performed usual care. Treating clinicians were blinded to allocation unless the patient disclosed that their visit had been prompted by an SMS reminder; however, no clinicians reported this type of disclosure from patients. No adverse effects, harms or unintended consequences of the intervention were identified.
Outcomes
The primary outcome was recorded completion of a current asthma management plan during the three-month follow-up period. The secondary outcome was recorded completion of spirometry during the three-month follow-up period. At study conception, it was intended that attendance at the clinic for asthma care would be recorded as a primary outcome measure; however, data for attendances specifically for asthma care were unable to be retrieved, as the practice software was unable to reliably distinguish between asthma-related and non–asthma related attendances. Instead, we chose spirometry as a second important indicator of asthma care. Primary and secondary outcome data were collected from participants’ clinic records by JC at the end of the three-month follow-up periods (August–September, 2016). Data for other patient characteristics (age, sex, smoking status, relationship status, medication use) were collected from the clinic database at the time of study enrolment.
Statistical analyses
Data were analysed using SPSS statistical software version 24. Outcome data were collected from the primary care database and manually entered; 50% of data were compared to the source database to verify accuracy. Chi-squared tests were used to compare differences in proportions of the outcome variables between the intervention and control groups. To detect a medium effect (Cranmer’s φ = 0.30) with a type one error of 5% (α = 0.05) and power of 80% (β = 0.80), we required 44 participants in each group (n = 88 for this two-group study). As this number was close to our estimates of maximum likely enrolment, we chose to recruit as many participants as possible. There were no missing data on primary or secondary outcome measures. Analyses were conducted using an intention-to-treat approach. There was no loss to follow-up, and no cross-over of participants between intervention and control groups.
Results
Of 588 eligible patients, 138 consented to participate in the study (response rate 23%) and none were lost to follow-up. Progress of participants through the study is detailed in Figure 1. Participant characteristics are described in Table 1.
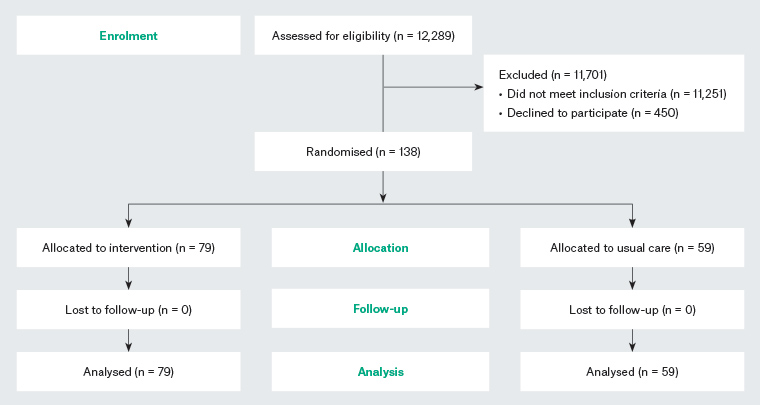
Figure 1. Participant progress through the randomised controlled trial
| Table 1. Participant characteristics |
| Characteristic |
Usual care (n = 59) |
Intervention
(n = 79) |
| Mean ± standard deviation |
Mean ± standard deviation |
| Age (years) |
|
53.14 ± 15.58 |
52.29 ± 17.00 |
| BMI* (kg/m2) |
|
32.38 ± 7.75 |
28.32 ± 5.45 |
| |
|
% (n) |
% (n) |
| Age by group (years) |
18–34 |
5.1 (3) |
13.9 (11) |
| |
35–49 |
40.0 (23) |
29.1 (23) |
| |
50–64 |
32.2 (19) |
31.6 (25) |
| |
≥65 |
23.7 (14) |
25.3 (20) |
| BMI (kg/m2) by category* |
<18.50 |
– |
2.9 (2) |
| |
18.50–24.99 |
18.5 (10) |
22.9 (16) |
| |
25.00–29.99 |
44.4 (24) |
40.0 (28) |
| |
≥30.00 |
55.5 (30) |
34.3 (24) |
| Sex |
Male |
30.5 (18) |
34.2 (27) |
| |
Female |
69.5 (41) |
65.8 (52) |
| Smoking status |
Current |
20.3 (12) |
14.3 (11) |
| |
Past |
23.7 (14) |
23.4 (18) |
| |
Never |
55.9 (33) |
62.3 (48) |
| Relationship status† |
Married/de facto |
54.5 (30) |
58.1 (43) |
| |
Divorced/separated |
3.6 (2) |
9.5 (7) |
| |
Widowed |
5.5 (3) |
6.8 (5) |
| |
Single |
36.4 (20) |
25.7 (19) |
*Data are missing for five usual care group cases and nine intervention group cases; underweight: <18.50 kg/m2,
normal: 18.50–24.99 kg/m2, overweight: 25.00–29.99 kg/m2, obese: ≥30.00 kg/m2.
†Data are missing for four usual care group cases and five intervention group cases.
BMI, body mass index; –, no data |
Intervention effects are summarised in Table 2. In the usual care (control) group, five of 59 (8.47%) participants had a completed asthma plan by the end of the follow-up period, compared with 35 of 79 (44.30%) participants in the intervention group (odds ratio [OR]: 8.59; 95% confidence interval [CI]: 3.10, 23.78; P < 0.0001). This represents a number needed to treat (NNT) of three (95% CI: 2.00, 4.60). Similarly, there were significant differences between groups for the proportion of participants who had spirometry performed during the follow-up period (OR: 5.62; 95% CI: 2.36, 13.36, P = 0.0001). Effect sizes for asthma action plan and spirometry completion (based on chi-squared statistics) were moderate (φ = 0.39 and 0.35, respectively).
| Table 2. Effect of SMS reminders on asthma action plan and spirometry completion |
| Outcome |
Usual care (n = 59) |
Intervention (n = 79) |
Difference in % [95% CI] |
χ2 |
P value |
| n |
% |
n |
% |
| Completed action plans |
5 |
8.47 |
35 |
44.30 |
35.83 [21.46, 47.79] |
20.91 |
<0.0001 |
| Completed spirometry |
8 |
13.56 |
37 |
46.84 |
33.28 [18.01, 45.98] |
16.90 |
<0.0001 |
| CI, confidence interval |
Discussion
We report one of the first studies to test the efficacy of an SMS reminder service for improving attendance at a general practice clinic for two important aspects of routine asthma care – completion of an asthma action plan and spirometry. One other study, by Holton et al in 2010, has evaluated a systematic approach to care of asthma in Australian general practice,22 which incorporated a postcard reminder system followed up with a phone call (if required) to prompt patient attendance for an asthma review. In contrast to the present study, Holton et al’s study tested a wider intervention including clinician education, service incentives and setting up a practice register; thus, the reminder was only one part of a multicomponent intervention. While they reported an increase in the provision of asthma management plans over a 12-month follow-up period, their rate of completed action plans was lower than in our study, suggesting that SMS reminders may be a more effective method of increasing attendance. In fact, our study showed a clinically significant difference of 35.83% in the proportion of completed asthma action plans, representing an NNT of three. While our study did not test the implementation of a multifaceted intervention per se, it did show a translation from planned appointment to provision of asthma action plan, suggesting that planned visits allow the time needed for GPs to develop or update action plans as part of asthma management. Our study engaged existing practice nurses to provide asthma care, and this aspect of our asthma care service is likely to be similar across other practices in Australia.
This study has several limitations. First, we included only participants who consented to participate, introducing potential for selection bias as patients who refused participation might also be less likely to respond to this type of intervention. Moreover, a relatively low response rate (23%), while comparable with other research in the general practice context, limits the generalisability of our results. However, our target population comprised only those who did not have a current asthma action plan, and so probably included people with milder asthma and/or those who are not engaged in their asthma care, demonstrating the potential for this type of intervention to engage hard-to-reach patients who do not present for routine asthma care. Diagnosis of asthma was based on previous assessments by treating doctors and was not confirmed at enrolment with further clinical assessment; asthma severity assessment was also beyond the scope of the current study. Outcomes for this study were limited to asthma care plan and spirometry completion; future studies could assess effects on other patient-relevant endpoints such as asthma control, number of asthma flares and hospital visits. Finally, this study targeted patients at a single suburban general practice and may not be generalisable to other practices with different populations; however, suburban demographics are comparable to the average Australian suburb, suggesting results are likely replicable in the broader population. There was also a slightly larger proportion of participants who were current smokers and/or had a body mass index ≥30.0 kg/m2 in the control group, and the effect of this on our results is unknown. Replication of results in larger trials, with more sociodemographically diverse samples, is required to support the generalisability of results, and larger samples would allow for regression analyses to identify factors (eg age, smoking) influencing intervention efficacy.
Conclusion
We are witnessing a rapid shift towards more sophisticated mobile health interventions for respiratory disease management, including eHealth23 and mobile-based apps that require further testing but also development and maintenance. SMS reminders are cheap, use existing infrastructure and are acceptable to patients.24 Many practices and health services use SMS for recalls and appointments already.25 Our results suggest that SMS reminders may be an effective intervention to increase rates of asthma care plan and spirometry completion for adult patients with a history of asthma but no current asthma management plan. Future research should aim to replicate these findings but also aim to see if differences in patient-relevant outcomes can be achieved.