Surgical management of lacerations refers to those techniques that necessitate perforation of adjacent uninvolved tissue in order to achieve primary would closure.
The principal objective of surgical wound closure is to expedite the healing process with good haemostasis and excellent approximation of dermis and epidermis, preferably with eversion of wound edges. This configuration assures optimal cosmesis.
Once the wound has been assessed, cleaned and/or debrided, and the need for surgical management identified, decision making is largely centred on the choice of suture techniques and materials. Subsequent aftercare must also be prescribed.
The essentials of wound assessment and preparation, and the criteria for specialist referral, have been outlined in a companion article on the non-surgical aspects of management.1 This article outlines the principles of surgical repair techniques for simple linear lacerations.
Suture types
In most situations, interrupted sutures provide the capacity to make fine adjustments to wound edge approximation and eversion as closure progresses. This technique also enables selective early suture removal to allow drainage if a segment of the wound becomes infected, thus obviating a complete wound dehiscence. Useful types of interrupted sutures include:
- Simple interrupted (Figure 1). This is the most commonly employed suture type for the repair of cutaneous defects. Although more time-consuming than continuous sutures, they afford better precision when aligning wound edges.
- Subcutaneous interrupted (Figure 2). For deeper wounds, closure of subcutaneous dead space is generally desirable to optimise cosmesis and minimise the risk of wound infection. This must be done with an absorbable suture in a configuration in which the knot points into the depths of the wound rather than protruding from it. This is achieved by passing the needle from deep to superficial then superficial to deep. If possible, the superficial component of the suture should pass through the dermis, as this is the collagen-rich layer on which scar integrity depends. If these sutures can efficiently approximate the dermis, a subsequent layer of cutaneous sutures will be under minimal tension, thus reducing the risk of an expanded scar. In some cases, it may suffice simply to apply adhesive strips to the epidermal layer.
- Vertical mattress (Figure 3). These cutaneous sutures effectively force wound edges into eversion. Because they are more time-consuming to perform than simple interrupted sutures, they need only be used for segments of the wound where there is a natural tendency to invert.
- Figure-of-eight (Figure 4). This cutaneous suture is particularly useful for slightly tense wound edge approximations, as the tension is distributed between two line segments rather than two points. It also serves well for haemostasis in highly vascular wounds such as on the scalp, as a result of any small bleeding vessels being gathered up within the encircling figure-of-eight. The figure-of-eight suture can also be applied to small or ill-defined bleeders in subcutaneous fat when electrocautery is not available.
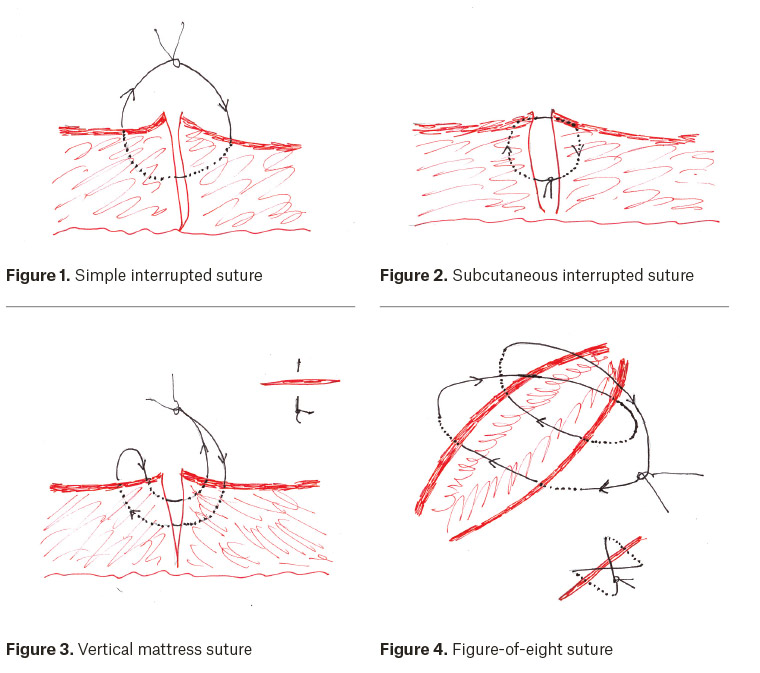
With appropriate experience, equally satisfactory wound closure can be achieved with continuous (running) sutures. The two basic types are:
- Cutaneous continuous (Figure 5). These are useful for rapid haemostatic closure of linear lacerations. A degree of care is required to ensure good wound edge eversion and minimal gaps in closure. For longer wounds, an assistant may be helpful to hold the suture with each pass of the needle to maintain the necessary tension. This process is known as following.
- Subcuticular (Figure 6). This is a running suture effected in a horizontal plane, entirely within the dermis. Lacerations should be linear, with clean wound edges and a well-defined dermal layer. It is especially useful in children where suture removal would prove traumatic. To avoid gaping or puckering in wound closure, successive passes of the suture should be set slightly back from (rather than directly opposite) the exit point of the preceding suture pass on the opposite wound edge. This configuration also facilitates wound edges holding together with the desired suture tension as closure proceeds; following by an assistant is usually not necessary. To complete closure, the needle is brought out through the skin beyond the apex of the wound, passed back in immediately adjacent to the exit point and brought out at an angle of <90 degrees to the line of the wound. This enables the suture to be locked in position while maintaining its desired tension. The emerging suture is then cut flush with the skin. An alternative means of completing a subcuticular suture is the so-called Aberdeen knot.2
Choice of suture materials
Commonly preferred suture materials for cutaneous lacerations are summarised in Table 1, which lists their characteristics and uses.
Non-absorbable suture materials are preferred for cutaneous wound closure. They maintain tensile strength for prolonged periods. Absorbable sutures are necessary for subcutaneous use, where suture removal from the healed wound would not be possible. Unlike non-absorbable sutures, absorbable sutures start to lose tensile strength after 1–2 weeks and may take several months to reabsorb fully.
Monofilament sutures are usually synthetic polymers, which have a slightly increased tendency to loosen or slip due to ‘memory’. However, the advantage of this is that a knot too loosely applied initially can be tightened with successive throws. Conversely, multifilament or braided sutures will hold securely with the first throw, but no further adjustment of tightness is possible thereafter. Despite its useful handling qualities, silk has largely been surpassed by synthetic monofilaments because of the theoretical risk of increased bacterial adherence.
For optimal cosmesis, the finest possible suture calibre that will accommodate the tensile forces on the wound should be chosen. This depends on body location, but a general guide is: 5-0 or 6-0 for face; 4-0 or 5-0 for limbs and scalp; 3-0 or 4-0 for torso.
| Table 1. Types, characteristics and uses of common suture materials |
| Type |
Characteristics |
Use |
| Nylon |
Non-absorbable, monofilament |
Any type of cutaneous suture |
| Polypropylene |
Non-absorbable, monofilament |
Any type of cutaneous suture |
| Silk |
Non-absorbable, polyfilament |
Any type of cutaneous suture |
| Polyglactone |
Absorbable, polyfilament |
Subcutaneous sutures |
| Poliglecaprone |
Absorbable, monofilament |
Subcuticular sutures |
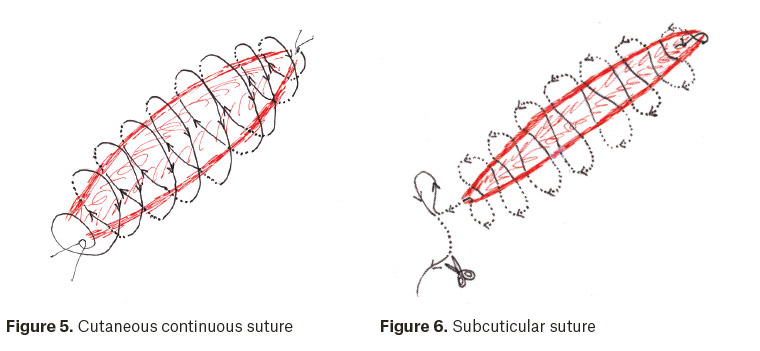
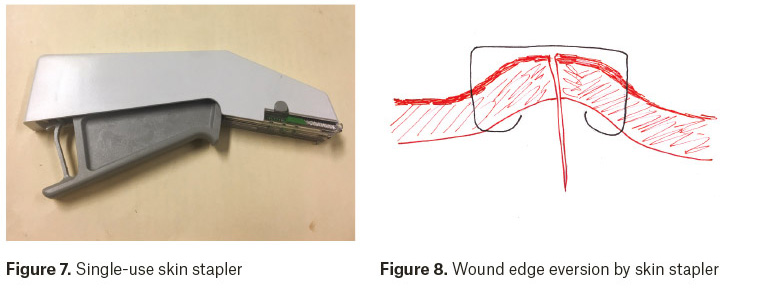
Staples
Commercially available single-use stapling devices (Figure 7) may be an alternative to simple interrupted sutures where rapid wound closure is needed. Staples are made of stainless steel, which does not react with tissues. Application involves less tissue trauma than regular sutures, thereby theoretically reducing the risk of wound infection. Another advantage is the action of the stapler itself, which tends to promote wound edge eversion (Figure 8). A purpose-designed device, which is usually reusable, is required for staple removal.
Post-operative wound care
It is generally advised to keep a sutured wound covered and dry for at least 24 hours, although some evidence suggests that leaving it uncovered and wetting it after 12 hours does not increase the infection rate.3 If a protective covering is initially required, light-weight occlusive or semi-occlusive dressings with a non-stick pad are better than dry gauze dressings in terms of faster wound healing and decreased infection rates.4 Once the wound has been uncovered, antibiotic ointment or white petroleum jelly can be applied daily to the sutured wound to prevent desiccation and bacterial contamination.5,6 This is often the preferred aftercare of facial lacerations from the outset, as application of wound dressings may be difficult.
For optimal cosmesis, non-absorbable cutaneous sutures or staples should be removed as soon as the scar can withstand the tensile forces in a particular location (Table 2). This is further rationale for a reinforcing layer of subcutaneous absorbable sutures wherever possible, to avoid the ‘tram-track’ appearance of scars where cutaneous sutures have been left in for too long.
| Table 2. Timing of suture removal |
| Wound location |
Timing of removal (days) |
| Face |
3–5 |
| Scalp |
7–10 |
| Arms |
7–10 |
| Torso |
10–14 |
| Legs |
10–14 |
| Dorsum of hands or feet |
10–14 |
| Palms or soles |
14–21 |
Additional practice tips
The width of suture bites, or the distance from the wound edge to the point of needle entry/exit, should be equal on both sides of the wound. As a general rule of thumb, the total width of the suture pass across the wound edges should be roughly equal to the distance between sutures.
If there is a slight discrepancy in length between wound edges, this can be compensated by slightly wider spacing of needle entry/exit points on the longer side of the wound. This will avoid an unsightly dog-ear at the end of the wound. Some clinicians find this more easily achieved by placing the first suture at the mid-point of the wound and then successively halving wound segments until satisfactory wound edge approximation has been achieved.
Ragged wound edges require scalpel debridement to achieve a more linear closure, as do any sections of the wound that are obviously devascularised. If this results in a slightly gaping wound, closure tension can be relieved by undermining the edges with sharp (scissor) dissection at a level just superficial to the deep fascia. Dissection can proceed away from the wound edges for a variable distance, usually in proportion to the length of the wound.
Tying of knots with instruments typically involves a series of alternating forward and backward throws. Executing the first throw as a double one affords less slippage pending securing of the second throw. Three to four throws usually suffice if using braided sutures, while monofilament sutures usually require five to six because of the greater likelihood of loosening or slippage.
While most simple lacerations can be surgically treated by a single practitioner, an assistant will increase efficiency for larger wounds by cutting sutures once knots are completed or ‘following’ continuous sutures to maintain tension as the wound edges are being brought together.
Key points
- The aim of surgical management of lacerations is to expedite healing with optimal haemostasis and cosmesis.
- A repertoire of specific suture techniques can be acquired to adapt to the requirements of the wound and patient.
- Suture material and calibre should similarly be selected according to the specifications of the wound and its anatomical location.
- Aftercare involving wound dressings and timing of suture removal should be aimed at minimising infection and scarring.