For many years, exercise has been seen as a healthy lifestyle pursuit but not a central part of medicine. There are now many conditions, particularly chronic diseases, for which exercise needs to become a critical first-line medical treatment to follow evidence of effectiveness.1,2 These conditions include osteoarthritis, back pain, diabetes, cardiovascular disease, depression and cancer, including breast cancer.3,4 Such chronic diseases now account for one-third or more of the entire health budget in modern Western society,5 all of them being named as ‘health priorities’ in Australia and collectively representing a high proportion of a general practitioner’s (GP’s) caseload.6,7
Exercise is particularly important as the first-line treatment for osteoarthritis and back pain, as emerging evidence in favour of exercise has coincided with strong evidence that many of the traditional medical treatments are actually not helpful.8,9 Opioid prescription is now to be avoided as a management strategy for osteoarthritis and back pain because of the potential for addiction and other serious side effects in the long term.10 While non-steroidal anti-inflammatory drugs (NSAIDs) are still recommended as a treatment option for osteoarthritis and back pain, they confer a 30% increase in major cardiovascular events in users;11 therefore, they are unsuitable for patients who are in the high-risk group for a cardiovascular event. Some of the traditional surgical procedures in musculoskeletal medicine, such as knee arthroscopy for degenerative knee conditions12 and spinal fusion for chronic back pain associated with disc degeneration,13 have now also been downgraded as management options because of their inability to perform better than placebo or comparison treatment in randomised controlled trials.
This evidence has rapidly expanded in the past decade; therefore, many family practitioners may not have been taught how to best prescribe exercise during either their medical school or postgraduate training.14 Referral to an exercise physiologist, physiotherapist or sport and exercise medicine physician15 is an available option (Box 1), but the need to include exercise prescription as part of the management plan for such an array of conditions means that a basic skill set is now an important part of primary care.
| Box 1. Exercise-based practitioners for secondary referral |
Allied health
- Exercise physiologists are partially funded by the Medicare Benefits Schedule (MBS) and regulated by their own collegiate body, Exercise and Sports Science Australia. The advantage of referring patients to exercise physiologists is that they will always provide the desired treatment (exercise prescription) and, being based on function, they will tend to avoid the biomedical paradigm that can make practitioner treatment counterproductive for conditions/patients that require increased exercise as the primary management. Exercise physiologists are now used as the primary allied health group for managing exercise programs for cancer patients in Australia.
- Physiotherapists are regulated by the Australian Health Practitioner Regulation Agency (AHPRA) and their own collegiate body, Australian Physiotherapy Association. Physiotherapists have training in musculoskeletal diagnosis and management, so they are an ideal allied health choice when there is a pain diagnosis that requires consideration of biomechanics. There is variation between philosophies among physiotherapists, although active (exercise-based) treatment is becoming relatively more common than passive treatment as evidence increasingly supports the former treatment type.
- Some other allied health practitioners can be exercise-based and a suitable referral for patients if they adopt this philosophy (eg podiatry, some chiropractors). Allied health referrals can be made for eligible patients under Chronic Disease Management (CDM) plans, although there may be out-of-pocket payments due to rebate limits.
Medical
- Sports and exercise medicine (SEM) physicians are AHPRA-recognised medical specialists under the auspices of Australasian College of Sport & Exercise Physicians (ACSEP), whose practitioners require a general practitioner referral to be seen under the MBS. SEM physicians are trained both in exercise prescription and diagnostics (as specialists they are able to order magnetic resonance imaging scans under the MBS) and other medical management. SEM physicians are ideal for community-based patients who have complex issues and a medical condition that responds to exercise-based treatment, or elite athletes or high-demand workers who need to manage high loads. Currently, SEM physicians are not eligible to see patients under the CDM scheme, so patients must expect substantial out-of-pocket expenses.
- Rehabilitation medicine physicians are AHPRA-recognised medical specialists under Australasian Faculty of Rehabilitation Medicine within The Royal Australasian College of Physicians. They treat both community- and hospital-based cases for rehabilitation of both chronic conditions and post-operative cases. They are ideal for referrals for hospital- or community-based patients who need to be seen under the CDM scheme.
|
Key concepts in exercise prescription
Exercise and all-cause mortality
Very strong cohort evidence from multiple studies shows that baseline exercise levels are highly predictive of all-cause mortality in both men and women,16,17 and are also predictive of cardiovascular disease18 and cancer.19,20 The correlation between exercise (at moderate levels or higher) and all-cause mortality is higher than the correlation between body weight and all-cause mortality.21–23 From a health outcomes viewpoint, it would therefore be beneficial to move away from a focus on body weight in favour of measuring physical activity. Although exercise is difficult to define and measure precisely when compared with body weight, body mass index (BMI) and other measures such as blood pressure, wearable step-counting technology (included in all late-model smartphones) makes accurate estimation of baseline exercise more simple than it previously was.24 Consumer wearables are rated as being accurate enough for self-monitoring but not yet the gold standard for research into physical activity.25
Physical activity as a vital sign
It has been suggested that doctors should record physical activity levels as a ‘vital sign’ (accorded similar prominence to, for example, blood pressure).26–28 A basic physical activity ‘vital sign’ questionnaire can take the form of:
- patient questions, such as
- ‘On average, how many days per week do you engage in moderate-to-strenuous physical activity (such as a brisk walk)?’
- ‘On average, how many minutes do you engage in exercise at this level?’
- days/week × minutes/day = minutes/week can be used to calculate reported weekly minutes of moderate physical activity.
Self-reporting can provide important information about whether exercise levels are adequate, with the increase in wearable technology having the potential to add even more detailed information.
Measuring step counts using wearable technology
The ubiquitous uptake of smartphones means that many patients have the opportunity to count daily steps.29 Although walking (and running) is not the only way to avoid being sedentary, the ease of measuring walking dose makes exercise prescription easier. However, not everyone has a modern smartphone (particularly elderly patients), and not everyone keeps their smartphone on them at all times during the day (particularly women, who may choose clothing that does not include pockets and instead keep their phones in a handbag that they do not always carry). Furthermore, the sensible belief that overuse of screen time and social media, and being in ‘24/7’ contact, is challenging for mental health means that some people will deliberately avoid having a mobile phone on them at all times. For those people who do not wish to count steps using a mobile phone, there are plenty of wearable options (usually worn on the wrist, but sometimes on a belt or around the ankle) that can also count steps. Most of these require Bluetooth or other download to a device in order to visualise data. It is worth noting that wrist wearables are slightly less accurate at counting steps than a device connected to the lower limb, as pushing a shopping trolley or stroller may not count steps via a wrist wearable. Conversely, some upper limb tasks (such as playing the piano) will register steps, although it could be argued that upper limb activity is beneficial enough to warrant inclusion anyway. The cheapest wrist wearables are now available for less than $30, but increased functionality is offered by more expensive brands, all the way up to devices that can play music, measure heart rate, record a single-lead electrocardiogram and function effectively as a second mobile phone. Overall accuracy of step counters is quite good, but it is not perfect and may be slightly less accurate for elderly people when compared with younger age groups.30 There is now moderately strong evidence that wearable technology increases physical activity in terms of active minutes per day and step counts.31
To date, the marketing of wearable step counters has focused on people with high activity levels who are wanting to track high-level performance-orientated training (with 10,000 daily steps seen as the entry-level aspirational goal). There is even more potential to use wearable technology to shift sedentary people (<4000 steps/day) to moderately active (6000–7000 steps/day if walking, or 60 active minutes). Shifting people from ‘sedentary’ to ‘moderately active’ transfers most of the benefits of exercise.
In the future, upper limb and lumbar spine wearable load monitors may become commercially available as well, which will improve the management of musculoskeletal disorders for these regions. Until then, recording of minutes of upper limb/lumbar loading activity (+/– a modifier for perceived exertion) will be the best way to monitor load for these body areas.
The 10% rule
In sports such as track running, swimming and cycling, it has long been known that weekly training load should only be increased by 5–10% at a time. Evidence is now starting to emerge in both elite sport32–34 and for amateur activity35 that small weekly increases in load are generally tolerated, whereas higher weekly increases are likely to cause specific injury or pain flare-ups. When a patient is directed to increase the load of daily steps, the rate of increase should be ideally limited to 10% per week. This means it will take approximately two months to double the weekly step load, and such a method will minimise the risk of injury (refer to Cases 1 and 2). Walking and running, for which steps can now be directly measured, are not the only forms of activity that constitute acceptable exercise, with some people preferring group activities or upper limb–focused exercise. The need to increase gradually to avoid the risk of injury applies to other pursuits as well, with minutes of activity the primary unit, rather than steps. This gradual increase in activity sometimes presents logistical challenges, but the risk of injury/pain will be increased if a patient starts a new activity with a 45-minute or one-hour session. In addition to considering which forms of exercise will be enjoyable/accessible for the patient, planning needs to include a gradual build-up of sessions. Ten minutes is a reasonable starting length for an unaccustomed activity, with increases planned once sessions have been tolerated. Choice of exercise type for middle age onwards should involve not only enjoyment, but also consideration of which exercise types can be formatted to allow gradual build-up of load.
The ‘U-shaped’ curve for musculoskeletal pain
While there are certain conditions (eg cancer prevention and treatment) for which exercise has only beneficial outcomes; for musculoskeletal pain, both low activity and high activity are risk factors (Figure 1).36 It is known that sedentary people, manual workers and high-demand athletes are at increased risk for osteoarthritis and back pain, with those having regular and/or moderate loads at lower risk.37–39 All these relationships have a common U-shaped curve relationship, as seen in Figure 1.15,32,36 The bottom of the curve (lowest risk for musculoskeletal pain and injury) is sometimes referred to as the ‘Goldilocks zone’.40–43 Many of the differences in daily physical activity between adults can be explained by occupation.44
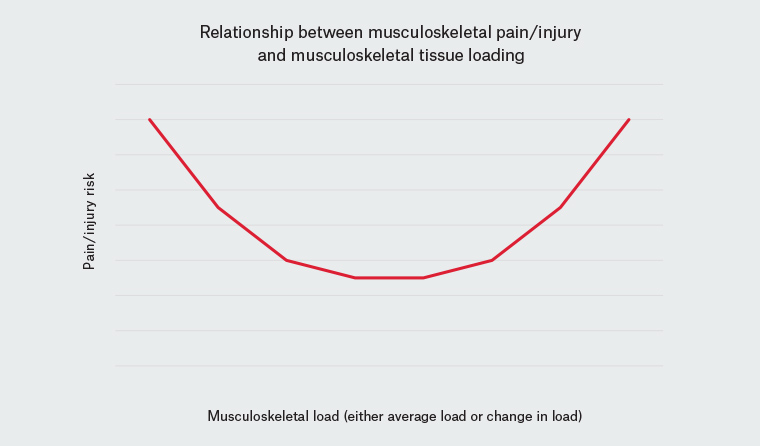
Figure 1. The relationship between musculoskeletal pain/injury risk and musculoskeletal loading (consistent with average lifetime load36–38 or change in load32,36,46)
Can you push through pain when increasing exercise?
It is essential to push through some pain when increasing exercise, as ‘soreness’ is an expected consequence of tissue overload, which is necessary for strengthening. The key consideration is to what degree pain indicates a health adaption versus ongoing failure to cope with load. Some of the principles that can be used as a guide are:
- For young athletes and the entire population from middle age onwards, soreness/aching/low-grade pain is a regular part of life and should be accepted as normal rather than feared.
- Pain levels that are self-rated as <5/10 are more likely to be associated with adaption, whereas pain levels rated as ≥5/10 are more likely to be associated with damaging overload; however, because pain is subjective, personality needs to be taken into account. A self-rating of pain of ‘11/10’ is a red flag not of severe tissue damage but of a patient who is not coping well with pain and may actually need counselling to try to understand why pushing through some pain can be beneficial in the long run.
- It is easier to determine whether pain is adaptive or counterproductive in the absence of painkillers. Although painkillers have the ‘advantage’ in the short term of decreasing pain, in the long term they have the disadvantage of removing the body’s appropriate feedback regarding adjustment to load.
- Activity upgrades that can be repeated after 2–4 days with no worsening of pain suggest healthy tissue adaption. A load upgrade that cannot be repeated because the pain is a lot worse during the second attempt suggests that the upgrade was too rapid.
- Imaging should not be rapidly considered when pain is reported in association with increases in exercise. A majority of joint magnetic resonance imaging scans taken from middle age onwards will show standard age-related degenerative changes, and these do not contraindicate exercise.
- A load upgrade that the body does not cope with can result in pain or injury that is somewhat remote (days to weeks) from the excessive load upgrade.45
- Self-managed gradual upgrades (or downgrades then re-upgrades) in which practitioner and patient are prepared to see progress slowly can be managed in primary care (Cases 1 and 2). If this fails, it is ideal to refer patients to a specialist doctor or allied health practitioner (Box 1) for greater assistance with load management/exercise dosing (as opposed to calling this ‘failed conservative treatment’ and then moving automatically to a surgical opinion).
Case 1
A female patient aged 58 years who was overweight (94 kg; BMI 32.5 kg/m2) and had diabetes presented to her GP complaining of ‘bad knee pain’ caused by her bilateral knee osteoarthritis. She asked for something ‘strong’ to relieve her pain, as she was worried about further weight gain due to activity restriction. Her GP cautioned her against using strong painkillers because of lack of efficacy and risk of side effects, and suggested paracetamol for short-term pain relief and measuring daily steps with a wrist wearable. After two weeks it was established that she was only averaging 2000 steps/day. It was planned that she would aim for 2200 steps/day (on average) the following week and to increase by a small amount each week so that in a month she would be taking approximately 3000 steps/day and in two months approximately 4000 steps/day. Because this gradual increase meant that she did not undertake any heavy walking days, her pain levels stayed under control (≤5/10 most days) and she tolerated the very gradual increase. After six months she had managed to reach 6500 steps/day; her pain was less than when she first presented, she was not using any painkillers and she had also noticed that her weight had dropped to 89 kg.
Case 2
A male patient, aged 48 years, who weighed 81 kg (BMI 26 kg/m2) presented with right plantar heel pain. He owned a small café and did 13,000 steps/day on average Monday to Friday at work (counted on the mobile phone he kept in his pocket), with slightly fewer steps on the weekend. His heel pain came on a week after arriving back from a holiday, during which he had tried to run every day for seven days to lose some weight. At the time of presentation, the pain had been present for three months, and the patient found it was worse first thing in the morning and then from lunchtime onwards. He said that he was unable to take any time off work, as the books at work would not balance if he had to pay a new worker to replace himself. The pain was getting worse, and he was taking 6 ×25 mg diclofenac per day to help cope with the pain. He wondered whether a cortisone injection might help him relieve the pain while he kept working. His GP advised against cortisone because of the likelihood that he would continue overloading the heel even if the cortisone did provide short-term pain relief. Instead, the instruction was to try to reduce steps to 9000/day for a few weeks in order to unload. The strategy to do this was discussed, and the patient decided to drive to work rather than catch the train, which cut off 2500 steps. The patient did so and returned after a month, saying the pain was neither worse nor better, but he was taking fewer diclofenac, and some days forgot to take any. Based on improvement (reduced use of non-steroidal anti-inflammatory drugs), the GP allowed him to increase to 10,000 steps/day for two more weeks, then 11,000 steps/day. Two months later, the patient had returned to walking 13,000 steps/day, which was his previous routine. He was not taking any more diclofenac and had only low-level heel pain. He had gained 3 kg, but he was very relieved that he had been able to keep working at his café.
Conclusion
Exercise prescription, although not part of the standard medical school curriculum, is now an essential skill in primary care. Exercise is an evidence-based treatment for osteoarthritis, back pain, tendinopathy, some cancers, depression, diabetes and cardiovascular diseases. It requires more than rudimentary understanding to successfully implement, as patients can become disheartened by temporary pain flare-ups. The need for medicinal and procedural treatment for many conditions can be reduced if proficiency in exercise prescription is developed.