High body mass index (BMI; ≥25 kg/m2) is now a problem in every country,1 and the prevalence of high BMI in Australia is one of the highest in developed nations.2 In 2017–18, 67.0% of Australian adults (12.5 million people) had a high BMI, and 31.3% (5.8 million people) were obese (BMI ≥30 kg/m2).3 This is a substantial increase from 1995, when only 56.3% of Australians had a high BMI, and represents a trend that is global and growing.3
In 2016, high BMI was estimated to be responsible for over 8% of deaths in the world and nearly 6% of the total disability adjusted life years (DALYs) lost. High BMI was ranked the third-highest risk factor in Australia for all-cause mortality (75 out of 100,000) and the highest risk factor for overall burden of disease, responsible for approximately 8% of the total DALYs lost.1
It is time for the discourse about obesity in clinical medicine to be broadened and informed by emerging evidence of the environmental determinants that affect obesity. Given the aforementioned statistics, relying on the formula of ‘eat less and do more exercise’, although it has some merit when treating obesity in the individual, has not halted the emerging crisis of obesity in modern human populations.
Additionally, the current largely individualistic approach represented in the media, research and clinical interventions has contributed to ‘weight stigma’ – the personal responsibility people feel for their being overweight. This is amplified by weight stereotypes and social attitudes that frame obesity as a ‘personal failure’4 and only serve to increase the stress on people who are overweight, thus risking further weight gain and harm to their health.5 Unfortunately, this stress is augmented by negative bias that has also been shown by some health professionals when treating people who are overweight.5–8
It is not possible to explain the sharp and continued rise in obesity throughout the world purely on individual grounds, whether genetic or behavioural.9 Obesity is a much more complex problem that extends far beyond individual choice, and is affected by multiple interrelated influences: social, such as level of education, employment and income;10 and environmental, such as the design of residential environments and the impact this has on access to healthy food and ability to be physically active.11
This complexity can be shown using a spray diagram, as is used in systems theory (Figure 1). Rather than a ‘simple’ personal behaviour (eg ‘eat less and exercise more’), this diagram shows multiple elements that interact to affect the epidemiology of obesity. Many of these forces are outside the direct control of individuals yet are critical to promoting healthy communities.
The importance of recognising ‘upstream’ factors to public health issues was well demonstrated by the history of tobacco smoking. Interventions outside the individual’s direct control – such as restriction of access to cigarettes, increased cost and regulations decreasing smoking in public spaces – played a vital part in decreasing smoking rates in Australia.12
The approach to obesity is slowly evolving in a similar way. Interventions including raising sugar taxes, improving nutrition in schools and reducing advertisements and exposure to high-calorie foods, especially for minors, is starting to be increasingly discussed and implemented. However, an area that requires more attention is that of the environment, especially the built environment – the environment constructed by humans as opposed to occurring naturally. The built environment is where nearly all humans live, work, play, eat and exercise. It includes housing, means of transport, worksites, schools, retail centres and recreation areas that are part of the large rural and urban networks around the globe.
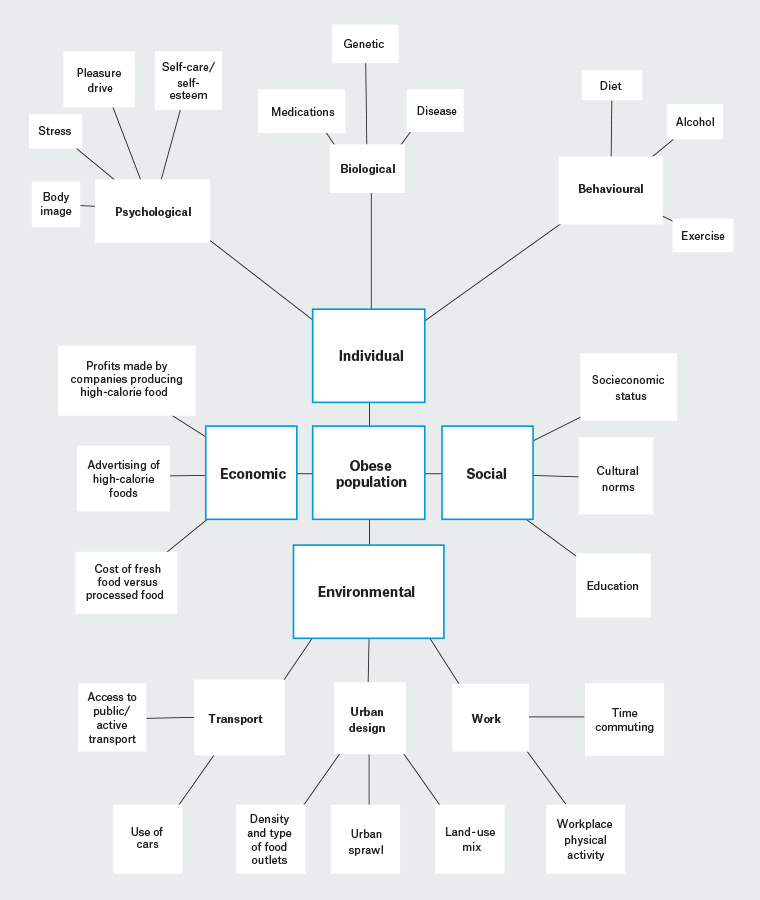
Figure 1. Spray diagram demonstrating elements connected in a system that facilitates obesity in populations
‘Obesogenic environments’: What is the evidence?
Research investigating the association between indices of the built environment and health is still in its early stages, with most being published since the start of this century. As part of this research, there has been accumulating evidence showing an association between obesity and the built environment.13–16 The term ‘obesogenic environments’ was coined as a result of this association. It is a somewhat misleading term, because the environment does not directly cause obesity as much as it provides the conditions encouraging weight gain – ‘most people will struggle to alter their behaviour in environments that promote high energy intake and physical inactivity’.9
One of the earliest associations of a measure of the built environment and obesity was reported by Ewing et al in the USA in 2003. After controlling for demographic and behavioural confounders, a measure of urban sprawl was found to have a significant association with obesity (P <0.001), as well as BMI (P = 0.005), minutes walked (P = 0.001) and hypertension (P = 0.018).17 The association with obesity was reproduced in many other studies that used population density as the measure to determine urban sprawl.18–24
Ongoing research aims to understand the reasons why urban sprawl is correlated with obesity. Data suggest that longer times spent travelling to work are negatively associated with healthy behaviour in general,25–30 possibly because of a trade-off between the time spent travelling and the time spent on healthy behaviour (eg cooking whole food and exercising).29 This is supported by a cohort study from Adelaide showing that the distance of one’s residence from the city centre was associated with abdominal circumference. Participants living ≥20 km from the city centre had a mean abdominal circumference increase of 2.4 cm over four years, in comparison to 1.2 cm for participants who lived ≤9 km away from the city centre.31 Other research has suggested that commuting time is a possible link between urban sprawl and obesity.32–38
Low-density development means that desired destinations (eg work, schools, shopping centres and transit stations) are further away from residences, and therefore are associated with greater use of cars. Wen et al concluded that driving to work was associated with an increased risk (adjusted odds ratio = 1.13; P = 0.047) of having a high BMI.34 Car use is generally associated with less physical activity,39 and the risk of obesity has been estimated to increase by 6% for each hour spent in a car daily.22 Conversely, using public transport has been negatively associated with obesity.40,41 There was a mean decrease in BMI of 0.3 kg/m2 (95% confidence interval: –0.47, –0.13; P = 0.0005) for people who changed from car commuting at baseline to active transport (bicycle/walking) or public transportation in a prospective study of over 20,000 commuters in the UK.37
As well as low-density development, other elements of urban design have been associated with obesity, such as town planning that discourages activity.22 A scarcity of green spaces (parks and trails), lack of footpaths, poor cycling infrastructure, low numbers of safe crossings, poor land-use mix that inhibits residents from walking to shops/schools/work, and building and school design that discourages the use of stairs and walking have all been found to be associated with obesity.42–44
An important sector of the built environment is the workplace. High BMI steadily rises in the working age group, especially in men, peaking at the age of 65 years.45 Decreased time for healthy behaviour because of commuting, an increase in sedentary jobs and the rise of labour-saving technology have all contributed to decreased activity and high BMI in this population.9,42 Additionally, features of the work environment have been suggested to affect physical activity, for example: stair access, connectivity between buildings and shelter from the elements, parking situation and availability of amenities such as gym/gym membership.42 Because of the time-poor nature of the working population, there is a scarcity of research into the workplace environment and obesity.46
Finally, ‘food security’, or reliable access to affordable healthy, fresh food, is important for maintaining healthy weight. Food security can vary according to area; for example, the cost of fresh food has been found to be greater in remote areas and neighbourhoods with fewer economic resources.47,48 The density and hence proximity of food outlets to homes, work and schools can affect the choice of food sourced and can vary according to area. In general, neighbourhoods of fewer economic resources have a higher density of smaller convenience stores and fast-food outlets, which have been associated with increased BMI.47,49 A study in the USA reported that a one standard deviation increase in the density of fast-food outlets was associated with a 7% increase in overweight/obesity.50
Conclusion
The large body of evidence, summarised in Table 1, is compelling and must be included in any public health strategy to tackle obesity. In the clinical setting, the evidence assists to develop a more holistic understanding of the difficulties that a person faces to achieve a healthy weight. This will decrease the guilt and stress of being overweight, improve rapport and potentiate the development of specific strategies such as using public transport or active transport where possible.
| Table 1. Elements of the built environment associated with weight gain |
| Sector of built environment |
Factors thought to affect weight gain |
| City growth |
Urban sprawl:
- more time commuting
- greater use of cars
- less active commuting (walking/bicycle)
|
| Transport |
Adequacy of public transport service:
- number and affordability of trains/buses
- distance to public transport stations
- destination accessibility
- facilities for bicycles
|
| Neighbourhood infrastructure |
Town planning:
- amount of green space
- footpaths
- street connectivity
- cycling infrastructure
- safe crossings
|
| Land use |
Land-use mix:
- greater variety (education, shops, employment, residence) in one area encourages walking to access destination instead of driving
|
| Food environment |
Density of convenience stores
Density of fast-food outlets
Affordable fresh-food outlets |
| Work/education place |
Sites that encourage walking:
- close to public transport
- stairs
- covered walkways
Dedicated areas for exercise:
|
As with most social and environmental drivers, general practitioners (GPs) can have a vital role in advocating for the health of patients, through participating in health research that informs the development of built environments. Among the many examples are the Ingham Institute for Applied Medical Research in Liverpool, New South Wales, which launched the Urban Incubator in 2018; and the RMIT University for Urban Research in Melbourne, Victoria. These insitutes provide platforms for researchers to disseminate public health evidence and to engage with landscape architects, health district executives, councils and the community to evaluate health and wellbeing aspects of developments.
Community groups are also opportunities for GPs to advocate for healthier environments; ‘Healthy Cities Illawarra’ is one example that has grown out of the World Health Organization’s ‘Healthy Cities’ movement. Finally, professional bodies such as the Australian Medical Association, The Royal Australian College of General Practitioners, Doctors Reform Society, Rural Doctors Association and Doctors for the Environment are well placed to develop position statements and media releases, and lobby for healthy built environments.
The way we build our cities, towns and rural environments affects our health. Our ability to access healthy food and participate in physical activity is contextual to the built environment. Unplanned and unsupported growth of cities means that populations who are already at risk of obesity, by having fewer economic resources, are pressured to find residences further away from centres of employment. They therefore rely more on cars and have less time to participate in healthy behaviour, thus increasing their risk of obesity and chronic disease. To help our patients, it is a matter of urgency that we move beyond our current approach. Increasing knowledge or advice on losing weight is not enough if the individual does not have enough time, money or resources to change to a healthier behaviour.