Coronary artery disease (CAD) is the single leading cause of disease morbidity and mortality in Australia and is responsible for approximately in one in 10 deaths.1 While chronic angina is a common presentation of CAD, up to half of individuals will initially present with myocardial infarction or sudden cardiac death.2 For the purposes of prevention, it is necessary to identify asymptomatic at-risk individuals likely to benefit from the early detection and treatment of CAD.
In Australia, risk assessment is recommended to be performed using the National Vascular Disease Prevention Alliance tool, which is in turn based on the Framingham Risk Equation.3 These office-based calculators integrate several risk factors in order to estimate absolute cardiovascular risk.3,4 While these tools offer a quick and cost-effective method of risk assessment, it is recognised that many patients are not identified as high risk prior to their first coronary event.5,6
Coronary artery calcium (CAC) is a highly specific marker of atherosclerosis that has prognostic value in predicting cardiovascular risk.3,7 The quantification of coronary calcium by non-contrast computed tomography (CT) has emerged as an attractive tool to improve risk stratification and risk reclassification in asymptomatic individuals.
What is coronary artery calcium?
CAC refers to calcium deposits in the coronary arteries that occur during atherosclerotic plaque formation.8 Previously thought to be a result of ageing, coronary calcium is an abnormal finding that can be identified as early as the second decade of life following fatty streak formation.9
The link between coronary calcium and atherosclerosis has been known since the 1970s, when fluoroscopically detected calcium was associated with adverse cardiovascular events.10 With the development of CT imaging, coronary calcium was found to correlate with atherosclerotic plaque volumes both in pathological specimens and in vivo using intravascular ultrasonography.11,12 As a surrogate measure of atherosclerotic burden, calcium score can be considered a reflection of an individual’s cumulative risk factor exposure across their lifetime.
How is calcium scoring performed?
Calcium scoring involves a CT scan of the heart using a slice thickness of 3 mm.3 The study is complete within 10 minutes, and the radiation dose is low at approximately 1 mSv.13 The scan is performed without contrast administration and therefore does not provide luminal stenosis assessment. This is unlike coronary CT angiography, which is typically performed for symptomatic patients with suspected obstructive CAD.7
CAC appears on CT as >1 mm2 areas of hyperattenuation (>130 Hounsfield units) and is most commonly quantified using the Agatston method.13,14 In this method, the angiographer reviews each 3 mm thick CT slice of the heart (usually 12–16 cm in length) to identify coronary calcium.13 The amalgamated volume and density of coronary calcium is then calculated using dedicated computer software (Figure 1).3
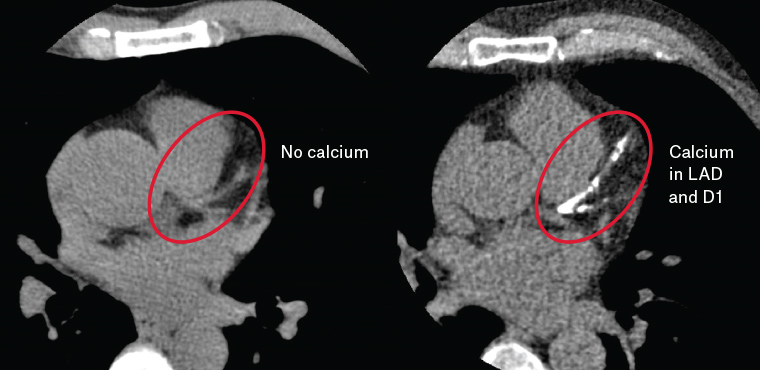
Figure 1. Coronary artery calcium in the left anterior descending (LAD) and first diagonal (D1) arteries
How are calcium scores interpreted?
Calcium scores are represented by an absolute numerical value and a percentile based on sex, age and ethnicity.7 The Cardiac Society of Australia and New Zealand (CSANZ) divides calcium scores into the following groups on the basis of absolute values: CAC = 0, CAC = 1–100, CAC = 101–400, and CAC >400, with each group corresponding to a particular level of cardiovascular risk (Table 1).3
| Table 1. Interpretation of coronary calcium score3 |
| Calcium score |
Interpretation |
Risk of myocardial infarction/stroke at 10 years |
| 0 |
Very low risk |
<1% |
| 1–100 |
Low risk |
<10% |
| 101–400 |
Moderate risk |
10–20% |
| 101–400 and >75th percentile |
Moderately high risk |
15–20% |
| >400 |
High risk |
>20% |
What are the benefits of calcium scoring?
Independent prediction of cardiovascular risk
Large prospective studies of asymptomatic individuals have shown that calcium score predicts important cardiovascular outcomes, including coronary events, myocardial infarction and all-cause mortality.15–17 Initial evidence supporting the prognostic value of coronary calcium was provided by the landmark Multiethnic Study of Atherosclerosis (MESA), a prospective cohort of 6814 individuals from four major ethnic groups.15 This study found an independent and graded association between calcium score and adverse coronary events over 3.8 years of follow-up.15 Subsequent studies have validated calcium scoring in a wide range of ages, sexes and clinical risk factor burdens,18–20 and have confirmed its long-term prognostic value over >10 years of prospective follow-up.16,17
Utility as a negative risk marker
A key advantage of calcium scoring is that while high scores are associated with elevated cardiovascular risk, the absence of coronary calcium is a negative risk marker that confers a favourable prognosis.3 In a meta-analysis of 71,595 asymptomatic individuals, the cardiovascular event rate in those with CAC = 0 was 0.47% over 50 months of follow-up, compared with 4.14% in those with a positive calcium score.21 Studies assessing all-cause mortality have reported similarly low event rates of <0.1% annually.22,23
The negative predictive value of zero coronary calcium appears to be greatest in individuals at intermediate risk by traditional risk calculators; 45% of these patients will have CAC = 0, placing them at a low cardiovascular risk and removing the need for preventive therapy such as statins.24 Conversely, the power of zero coronary calcium is limited in high-risk individuals, who remain at greater than low cardiovascular risk despite CAC = 0.24
Improvement on traditional risk calculators
Studies have shown that the addition of calcium scoring to traditional risk calculators improves the accuracy of risk prediction.15,25,26 In particular, the use of calcium scoring results in a significant net reclassification improvement (NRI), defined as the proportion of a population correctly reassigned to a higher or lower risk class following calcium scoring. Data from MESA determined that calcium scoring produced an NRI of 25% when added to the Framingham Risk Equation, and that this improvement was greatest in the intermediate-risk population, for whom the NRI was 55%.25 These findings have been corroborated by subsequent studies.3,26,27
What are the limitations of calcium scoring?
High-risk and low-risk asymptomatic patients
While intermediate-risk patients benefit the most from calcium scoring, studies have generally reported smaller reclassification benefits among low- and high-risk individuals.25–27 In a study of 2028 patients, the NRI of calcium scoring when added to the Framingham Risk Equation was 12% in the low-risk group and 34% in the high-risk group, compared with 52% in the intermediate risk group.27
The smaller reclassification benefit in low-risk populations can be attributed to a high prevalence of zero coronary calcium, which results in many patients remaining at low risk following calcium scoring.28 Conversely, the low prevalence and reduced negative predictive value of CAC = 0 in high-risk individuals limits the ability of calcium scoring to reclassify cardiovascular risk in this population.24
Symptomatic patients
Calcium scoring is not currently recommended for symptomatic patients by the CSANZ.3 Instead, guidelines recommend the upfront use of stress testing or cardiac CT angiography, which provide assessment of ischaemia and luminal stenosis, respectively.3 While calcium scoring is a reliable measure of atherosclerotic burden, it does not distinguish between obstructive and non-obstructive CAD.29
Non-calcified plaque
Calcium scoring does not provide information on the presence or burden of non-calcified plaque, which has low radiological attenuation and requires contrast administration to be assessed.30 This is typically performed using coronary CT angiography.30 Non-calcified plaque burden has been identified as an important predictor of future adverse cardiac events, particularly among symptomatic patients.31 However, in asymptomatic patients, the use of coronary CT angiography to assess non-calcified plaque has not been shown to improve cardiovascular risk assessment when added to calcium scoring.32,33
Cost effectiveness
There are no available Australian data assessing the cost effectiveness of calcium scoring.3 Hence, the impact of calcium scoring on downstream investigations, procedures and resource use is not known. As no Medicare Benefits Schedule items exist for calcium scoring at this time, the cost of the test is funded by patients, approximately $150–200 per scan.
Other considerations
Calcium scoring involves approximately 1 mSV of radiation exposure, which is comparable to two screening mammographies.13 The benefit of improved cardiovascular risk assessment must be considered against the risks of radiation exposure (eg malignancy).
Calcium scoring is performed with a CT scan of the chest and may result in incidental findings. In a study of 966 individuals who underwent calcium scoring, 8.2% of patients had incidental findings requiring further investigation or treatment.34 Incidental findings may result in increased healthcare resource expenditure and psychological harm.34
Who should undergo calcium scoring?
The CSANZ recommends the use of the Framingham Risk Score to select patients for calcium scoring, as studies assessing its predictive value have typically used the Framingham Risk Equation as a comparator.3
The CSANZ suggests that calcium scoring is appropriate for asymptomatic patients at intermediate Framingham risk, for whom there is strong evidence supporting its ability to improve cardiovascular risk assessment.3 Calcium scoring may also be appropriate for lower-risk patients (6–10% 10-year risk) with concerning features not considered by the Framingham Risk Equation. The CSANZ suggests that in this group, Aboriginal and Torres Strait Islander patients and patients with a strong family history of premature coronary heart disease or diabetes may derive benefit from the increased accuracy of calcium scoring.3
Who should not undergo calcium scoring?
The CSANZ recommends against calcium scoring for high-risk and very low–risk patients (<6% 10-year risk), for whom calcium scoring has a limited ability to reclassify cardiovascular risk.3 The use of calcium scoring for symptomatic patients is also not recommended because of insufficient evidence supporting its use over functional testing, CT angiography and invasive coronary angiography (Figure 2).3
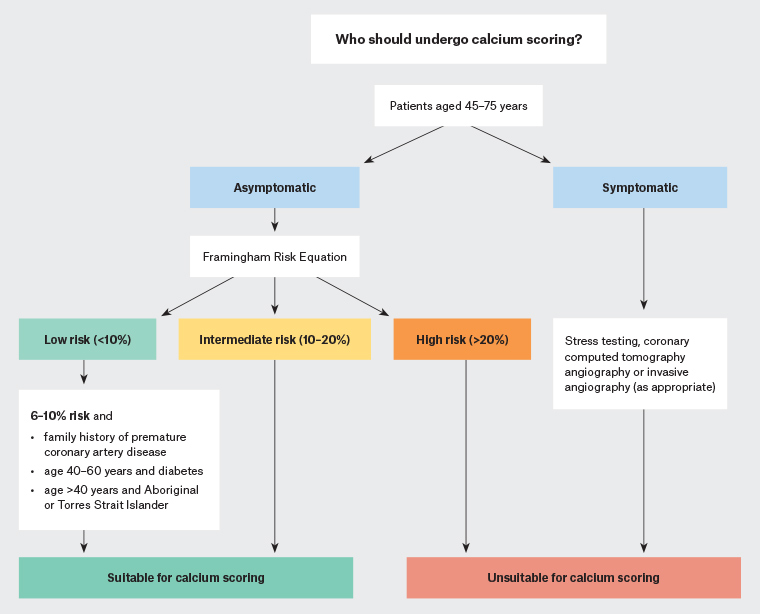
Figure 2. The Cardiac Society of Australia and New Zealand’s recommended indications for coronary artery calcium scoring3
How does calcium score guide management?
As calcium scoring improves cardiovascular risk assessment, it has the capacity to inform the risk-based selection of patients for preventive pharmacotherapy. A number of large observational studies show that calcium score identifies patients who may benefit from aspirin and statin therapy.35–37
Aspirin
Aspirin is not generally recommended for primary prevention as its cardiovascular benefits are outweighed by an increased risk of bleeding.3 However, calcium scoring has been shown to identify a subgroup of patients for whom prophylactic aspirin may be beneficial.
Using data from MESA, Miedema et al showed that aspirin had a net benefit among individuals with CAC >100.35 In this group, the calculated five-year number needed to treat (NNT) of aspirin to prevent one coronary event was significantly less than the number needed to harm (NNH) for major bleeding.35 Conversely, aspirin showed no net benefit for individuals with CAC = 0 and could not be universally recommended for those with CAC = 1–99.35
Statins
Studies have also assessed the ability of calcium scoring to guide lipid-lowering therapy. In a study of 950 individuals, the calculated five-year NNT of statins to prevent one coronary event was 549 for individuals with CAC = 0, compared with 24 for those with CAC >100, suggesting that statins should be prescribed for individuals with CAC >100 but may be withheld for those with CAC = 0.36 These findings were recently corroborated in a large study of 13,644 individuals over 9.4 years of follow-up.37
Recommendations
On the basis of the available evidence, the CSANZ suggests preventive therapy with aspirin and a statin is appropriate for individuals with CAC >100 and recommends no therapy for individuals with CAC = 0.3 For individuals with CAC = 1–99, preventive therapy can be considered if concerning features are present (eg family history of premature heart disease).3 Lifestyle management and risk factor control should be implemented for all patients regardless of calcium score (Figure 3).
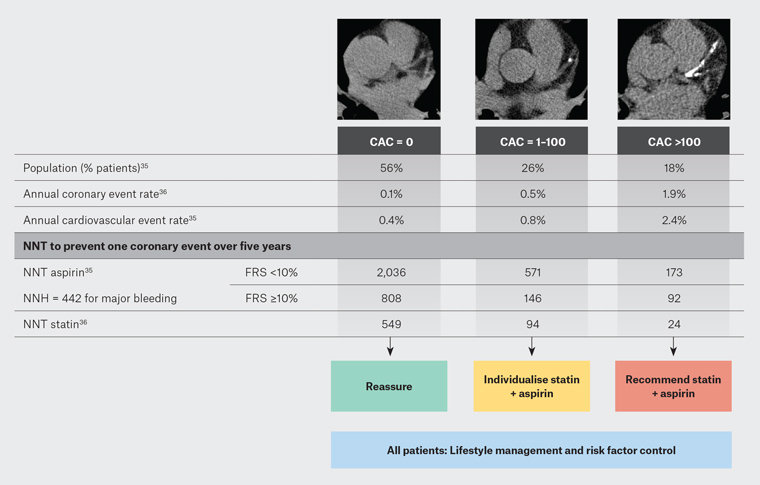
Figure 3. Treatment implications of coronary artery calcium (CAC) score41 Click here to enlarge
FRS, Framingham Risk Score; NNH, number needed to heal; NNT, number needed to treat
Adapted with permission from the British Institute of Radiology
Should calcium scoring be repeated?
CAC either increases or remains stable over time and does not regress.38 Calcium scoring can be repeated in order to reassess cardiovascular risk, provided that this would lead to changes in patient management. For this reason, the role of repeat calcium scoring is likely greatest for individuals with CAC = 0 for whom statins have been withheld. In this group, the CSANZ suggests repeat calcium scoring may be considered after five years, on the basis of data showing a mean time of conversion to a positive score of 4.1 years.3,39
Conversely, patients with CAC >100 should not undergo repeat scoring as they are already candidates for preventive therapy.3 Repeat calcium scoring may be less useful following statin therapy because statins mildly increase coronary calcium as a consequence of plaque stabilisation.40
Summary
Coronary calcium score is a surrogate marker of calcified atherosclerotic burden that independently predicts cardiovascular risk and mortality. It is a widely available test typically performed in intermediate-risk asymptomatic patients. Risk estimates provided by calcium scoring improves the accuracy of traditional risk calculators and can be used for the risk-based selection of patients for preventive pharmacotherapy.