This article is the first in a commissioned series on paediatric orthopaedics.
Scoliosis is a common paediatric condition with a prevalence of 0.47–5.2%.1 It is a three-dimensional deformity with a coronal plane Cobb angle >10° and rotation evident at the apex of the curve.2 Males and females are equally affected for small curves. However, females are seven times more likely to have a curve >40°.1 Scoliosis can be divided on the basis of age of onset: early onset (≤10 years of age; further divided into infantile [0–3 years of age] and juvenile [4–10 years age]) and adolescent (>10 years of age).3 Concerning curves include early onset scoliosis, premenarchal scoliosis with a curve >25° and mature patients with curves >50°. The role of the primary care provider is to identify significant curves and decide which patients require imaging and when to refer.
Aetiology
Scoliosis can be classified as structural or non-structural (Table 1). Non-structural lateral curvature can masquerade as scoliosis. Common causes include leg length discrepancy, pain, poor posture and spondylolisthesis. A leg length discrepancy can cause the spine to develop a compensatory curve to improve coronal balance. Pain from infection, tumour, trauma or nerve irritation can result in a curve from muscle spasm or relieving pressure on nerve compression. Advanced investigation with magnetic resonance imaging (MRI) is mandatory for patients with painful curves.4
| Table 1. Non-exhaustive list of causes of spinal curves |
Non-structural
(nil rotation) |
Structural (rotation) |
| Idiopathic (75%) |
Neuromuscular (10%) |
Congenital (10%) |
Other (5%) |
- Poor posture
- Leg length discrepancy
- Trauma
- Tumour
- Infection
- Nerve irritation
|
- Early onset ≤10 years
- Adolescent >10 years
|
Neuropathic
- Cerebral palsy
- Friedreich’s ataxia
- Polio
- Spinomuscular atrophy
- Spina bifida
Myopathic
Muscular dystrophy |
- Failure of formation
- Failure of segmentation
- Mixed
|
- Neurofibromatosis
- Skeletal dysplasia
- Metabolic disorders
- Collagen disorders
- Irradiation
|
The hallmark of a structural curve is axial rotation, which clinically manifests as a rib prominence (Figures 1 and 2). Structural causes of scoliosis include idiopathic (75%), neuromuscular (10%), congenital (10%) or other (5%).5 Neurological (upper and lower motor neuron) or myopathic conditions can give rise to scoliosis.6 Patients commonly will have a long, C-shaped curve with pelvic obliquity and truncal imbalance.

Figure 1. Clinical photographs of right-sided thoracic scoliosis
A. Patient standing; B. & C. Adam’s forward bending test measuring thoracic rotation and rib prominence using inclinometer application on the smartphone

Figure 2. Erect plain posteroanterior radiographs of the spine
A. Non-structural scoliosis secondary to spondylolisthesis; note symmetrical pedicles over the apex of the curve; B. Structural thoracic scoliosis with rotation at the apex of the curve; note asymmetrical pedicles and lateral deviation of the spinous process over the apex of the curve
Congenital scoliosis arises from an error in vertebral development resulting in failure of formation and/or segmentation.7 Failure of formation causes wedge/butterfly vertebrae or hemivertebrae. Failure of segmentation results in the fusion of spinal elements causing block vertebrae or vertebral bar. Prognosis is highly dependent on the vertebral malformation. The highest progression rate occurs with hemivertebrae and a contralateral bar.7 Non-vertebral skeletal, intra-spinal, cardiac and genitourinary abnormalities are common and require appropriate investigation.
Other causes of scoliosis include neurofibromatosis, skeletal dysplasia, connective tissue disorders and inflammatory conditions. Neurofibromatosis curves can be dystrophic or non-dystrophic.8 Dystrophic curves are short, sharp curves characterised by rib pencilling, wedge vertebrae and dural ectasia. Non-dystrophic curves behave similarly to idiopathic curves. Skeletal dysplasia and osteogenesis imperfecta are characterised by a rapidly progressing curve and osteopenia. Marfan syndrome is characterised by ligamentous laxity, aortic enlargement, tall stature, lens dislocation, high arched palate and arachnodactyly.
The diagnosis of idiopathic scoliosis is dependent on excluding the aforementioned underlying causes.9 A typical adolescent idiopathic scoliosis patient is a female with a convex right thoracic curve or convex left lumbar curve, right shoulder elevated, right rib prominence, left lumbar loin bolster, no abnormal neurology and no significant pain. Deviation from typical features should prompt a search for underlying causes.
Natural history
Patients with untreated idiopathic scoliosis have increased dissatisfaction with their appearance. One-third of patients feel their lives are limited as a result of scoliosis causing decreased physical activity and self-consciousness.10 Psychological therapy may be beneficial.
While scoliosis has cosmetic implications, its clinical significance is related to growth potential and respiratory function. Thoracic idiopathic curves may be associated with decreased respiratory function when >50° and increased shortness of breath when >80°.11 Scoliosis in children under 10 years of age may result in pulmonary hypoplasia and long-term respiratory failure.12
Pain is not a significant feature of scoliosis.4 Patients with untreated idiopathic scoliosis have increased prevalence of pain, but do not appear to experience pain of longer duration or stronger intensity than their peers and generally do not require analgesia.11 Long-term studies have shown that function in patients with curves of >40° was only marginally worse than in age-matched controls with no scoliosis.11 Scoliosis almost never causes paralysis, irrespective of curve size.
Clinical assessment
The goal of the clinical assessment is to identify any underlying cause, assess the severity and determine if the curve is typical or atypical (Box 1). Critical elements to determine during history-taking include family history, pre-existing conditions, pain and neurological symptoms.
| Box 1. Red flags for atypical curve |
- Structural scoliosis in a male patient
- Significant pain, particularly night pain
- Left-sided thoracic curves
- Abnormal neurological signs/symptoms
- Rapidly progressive curves
- Onset in childhood rather than adolescence
|
General inspection should look for findings associated with the aforementioned clinical syndromes. It is important to document curve location as well as shoulder and pelvis symmetry. Leg length discrepancy can be assessed by palpating both iliac crests while the patient is standing. Rib prominence, resulting from rotational deformity, is measured by the Adam’s forward bend test.13 In this test, the standing patient bends forward from the waist, and the examiner uses a scoliometer to measure symmetry between sides. A smartphone can be used as a substitute for a scoliometer for measuring scoliosis parameters (Figure 1).14,15 A patient with a measurement ≥7° requires imaging and referral to a specialist paediatric spine surgeon.16 A detailed neurological examination is required to assess tone, power, reflexes and sensation of upper and lower limbs.
Radiological assessment
A standing whole-spine plain posteroanterior and lateral radiograph should be obtained for patients with structural scoliosis. The Cobb angle measures the most significant magnitude of the curve from the superior endplate of the upper vertebral body to the inferior endplate of the lower vertebral body involved in the curve. Measurements are subject to high intra- and inter-observer error.14 The lateral radiograph can be used to identify sagittal plane deformities such as hypokyphosis and spondylolisthesis. Where available, EOS imaging is increasingly being used for the assessment of scoliosis deformities. MRI of the neuroaxis (brain and whole spine) should be obtained for patients with atypical curves or those undergoing surgery. Computed tomography is rarely required for initial scoliosis assessment. Given radiation risks, these authors recommend that it be ordered by the paediatric spinal surgeon as pre-operative work-up for severe congenital deformities.
Scoliosis progression
Curve progression is primarily related to curve magnitude and growth potential.17 Presentation Cobb angle is the most predictive factor of scoliosis progression.18 Cobb angle <25° is unlikely to progress, 25–50° will likely progress during skeletal immaturity and >50° will likely progress even after skeletal maturity.19 Assessment of growth potential is important in clinical decision making. Pubertal status correlates with peak growth velocity. Menses generally coincides with a slowing of growth, with most girls reaching skeletal maturity within 18 months. Peak growth velocity (growth of 5–6 cm in six months) usually occurs 6–12 months before menses. This growth spurt represents the period of highest risk of curve progression.17 Bone age is assessed by Risser grade on the iliac apophysis. This is graded from 0–5 on the basis of increasing ossification (Figure 3). A Risser grade of 0–2 represents skeletal immaturity, high growth potential and increased scoliosis growth rates.

Figure 3. Pelvic radiograph showing Risser grade. A Risser grade of 5 is a fully fused iliac apophysis; 0–2 indicates high growth potential; 3–5 indicates low growth potential.
Treatment
Treatment of paediatric scoliosis is dependent on the aetiology, magnitude of curve and growth potential. The goal of management is to enter skeletal maturity with a balanced spine that will notprogress. If the curve is >40–50° degrees at skeletal maturity, progression will likely occur. The treatment chosen should be the most minimally invasive option available that can achieve these goals for a specific patient. Referral to a paediatric spinal specialist is appropriate for immature patients with curves >20°, significant rotation (>7° on scoliometer) or red flags.
Non-operative
Non-operative treatments consist of observation, bracing and symptomatic management. Observation is appropriate for curves <20° in patients with high growth potential (Risser 0–2) and curves <40° in patients with minimal growth potential (Risser 3–5).20 If the curve is <20° without rotation, it is appropriate for the general practitioner to repeat plain radiograph imaging in six months’ time to assess progression. At each consultation, the patient should perform an Adam’s forward bend test. Bracing is appropriate for patients with a curve of 20–40° with high growth potential.21 A brace works by holding the deformity during growth. When brace treatment ceases at the end of growth, the curve will often return to its initial Cobb angle. Bracing reduces curve progression to <50° in 72% of patients, compared with 48% of patients whose treatment involved observation alone.21 Brace compliance correlates with treatment success.22 In adolescent patients with idiopathic scoliosis, 51% of untreated patients had progression, compared with 7% of patients wearing a brace 23 hours per day.23 As a result, bracing is often prescribed 23 hours per day. Symptomatic treatment includes an exercise regimen for core strengthening and posture control. Physiotherapy can help obtain and maintain muscle condition. In addition, physiotherapy scoliosis-specific exercises may be beneficial when used in conjunction with bracing. However, physiotherapy and manipulative treatments do not reverse structural scoliosis.24
Operative
Indications for the surgical management of scoliosis vary considerably depending on patient and curve factors; however, surgery can be indicated when the curve is >40–50°.20 Surgery can be divided into three groups: growth modulation, instrumentation without fusion and instrumentation with fusion.
Growth modulation
Thoracic growth is essential for lung development. Delaying spinal fusion is desirable until the patient is aged 10–12 years to allow chest and lung development.12 This can be achieved by using growing rods or vertebral body tethering.
Growing rods are expandable rods attached to the spine proximally and distally, allowing the spine to grow (Figure 4). They are inserted using a minimally invasively procedure with no fusion in the primary curve. At regular time intervals (often six monthly), the rods are expanded, surgically or magnetically, to straighten the spine and allow thoracic development. When chest growth is sufficient, the construct can be replaced with a posterior spinal instrumented fusion. Comparing spinal parameters pre–growing rods to post–definitive fusion, the mean Cobb angle decreases by 40° and total spine length increases by 11.3 cm.25
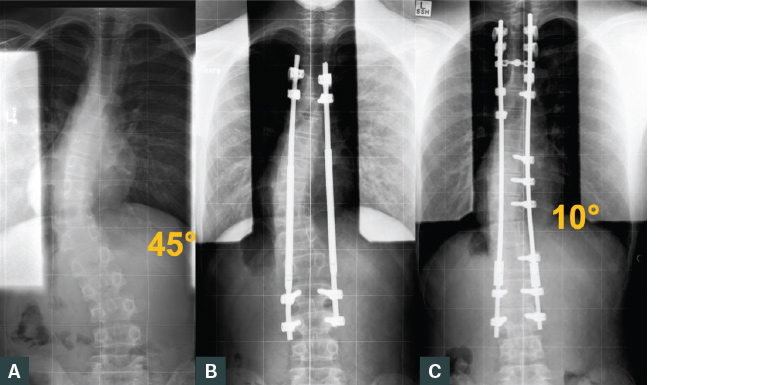
Figure 4. Erect plain posteroanterior radiographs of the spine of a patient with Arnold Chiari malformation type 1 and syrinx and atypical scoliosis treated with growing rods. Five lengthenings were performed, allowing a 13.2 cm increase in trunk length prior to definitive fusion.
A. Prior to treatment; B. Post–growing rod insertion C. Post–definitive posterior spinal instrumented fusion
Vertebral body tethering has been developed recently to treat young patients with scoliosis (Figure 5).26 This surgery can be considered if the patient has a single major thoracic curve of 30–65° and a Risser grade of 0–2.27 This fusionless procedure uses thoracoscopically placed vertebral body screws with a tape tensioned between connecting screws on the convexity of the curve. Only partial correction of the curve occurs intra-operatively. Spinal growth occurs asymmetrically, according to the Hueter-Volkmann principle, leading to further curve correction. Long-term data are still pending.
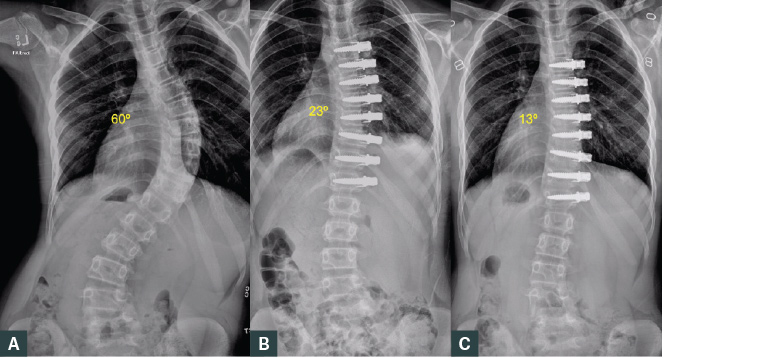
Figure 5. Erect plain posteroanterior radiographs of the spine of a female aged 13 years. The patient had a Risser grade of 0 with idiopathic scoliosis treated with vertebral body tethering.
A. Prior to treatment; B. Post-operative partial curve correction; C. Further improvement at six months post-operatively
Instrumentation without fusion
Bipolar instrumentation is a fusionless technique used for severe neuromuscular scoliosis (Figure 6).28 This recently developed technique uses proximal hooks, distal iliosacral screws and submuscular rods to distract and straighten scoliosis. Long-term data are still pending.
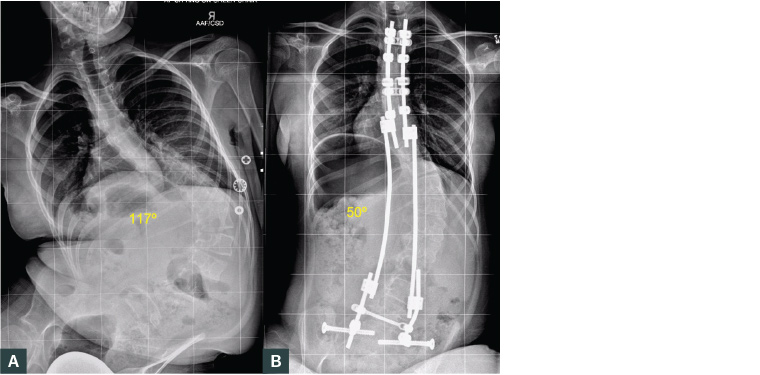
Figure 6. Sitting plain posteroanterior radiographs of the spine of a female aged 10 years with neuromuscular scoliosis (pelvic obliquity 27°) treated with bipolar posterior instrumentation.
A. Prior to treatment; B. Post-operative radiograph shows well‑balanced spine and minimal pelvic obliquity
Instrumentation with fusion
Spinal correction and fusion is generally reserved until patients are aged >10–12 years. Fusion can be anterior or posterior depending on curve and patient characteristics. The posterior approach is the most commonly used method for scoliosis correction (Figure 7). The thoracoabdominal approach is indicated in primary lumbar curves. The thoracoscopic approach is indicated for a single main thoracic curve (Figure 8).29
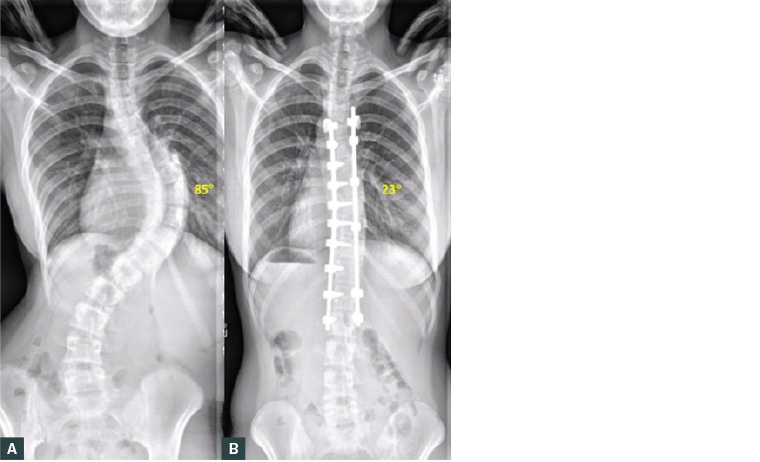
Figure 7. Erect plain posteroanterior radiographs of the spine of an adolescent with idiopathic scoliosis treated with open posterior spinal instrumented fusion.
A. Prior to treatment; B. Post-operative radiograph
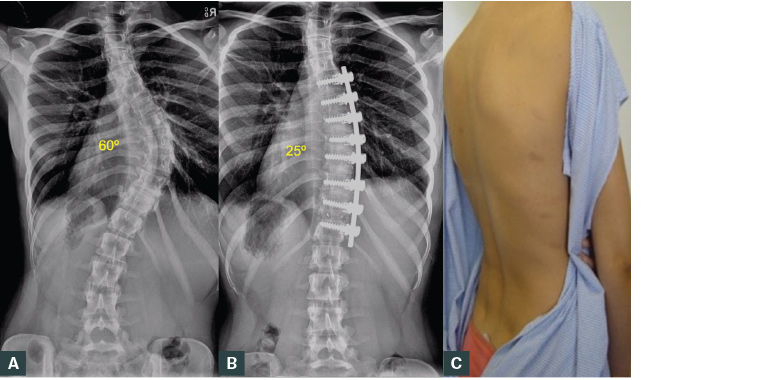
Figure 8. Female aged 16 years with idiopathic scoliosis treated with thoracoscopic instrumented correction and fusion.
A. Radiograph prior to treatment; B. Six month post-operative radiograph; C. Clinical photograph shows improved curve with minimal scars and rib prominence
Conclusion
Scoliosis assessment should identify structural curves, underlying causes, severity and growth potential. Red flags for atypical curves must be excluded. Observation is appropriate for curves <20° in patients with high growth potential (Risser 0–2) and curves <40° in patients with minimal growth potential (Risser 3–5). Bracing is appropriate for patients with curves of 20–40° with high growth potential. Indications for surgery vary depending on patient and curve factors. Surgery can be indicated when the curve is >40°. Early discussion with the local paediatric spine service can be considered.
Key points
- It is necessary to determine if the curve is structural; this can be done by measuring rotation on the forward bend test.
- Underlying causes for scoliosis (Table 1) must be excluded.
- Atypical curves and red flags need to be investigated (Box 1).
- Practitioners can assess the curve severity by examining radiographs, rib prominence and alignment.
- Growth potential can be determined using pubertal status and Risser grade.
- Early referral to a paediatric spinal specialist is recommended, especially for skeletally immature patients with curves >20°, patients with significant rotation or those with red flags.
- Management is based on growth potential and curve character.