Case
A Caucasian man aged 63 years with a history of heavy smoking and occasional alcohol drinking (<1–2 standard drinks per week) presented with concerns regarding a hard lump in the middle of his hard palate, which had been disturbing him for a few months.
His main concern was whether the lump could be ‘cancer’. He did not have any pain or tenderness, bleeding, oozing or discharge from the lump, and he reported that the lump was not growing. Systemic enquiry was unremarkable.
On physical examination, there appeared to be a smooth, approximately 1.0 cm × 1.5 cm, multilobulated, hard, non-tender, non-mobile, non-fluctuating lump, with the consistency of bone and natural colour of the oral mucosa in the midline, on the hard palate (Figure 1). There were no signs of discolouration or ulceration. There was no lymphadenopathy and no further concerning lesions.
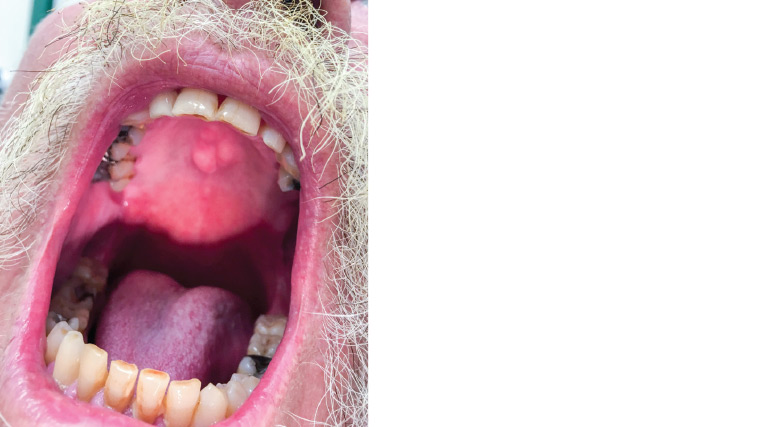
Figure 1. Clinical appearance of the lump on the hard palate (midline)
Question 1
What are the potential differential diagnoses?
Question 2
What is the initial investigation?
Answer 1
The most likely diagnosis based on the clinical presentation is bony exostosis.
Other diagnoses that can be considered include other primary osseous tumours such as osteoma, osteochondroma, osteoblastoma, chondrosarcoma or giant cell tumour.1,2 Non-bony differential diagnoses that may present with a firm mass or nodules include ossifying fibroma and inflammatory papillary hyperplasia.2
While there is a history of heavy tobacco use, oral tissue malignancies such as squamous cell carcinoma (SCC) are very unlikely to present in this manner, as they occur most commonly on the tongue, floor of the mouth and vermilion border of the lower lip.3
Answer 2
The diagnosis is primarily clinical; however, referral for imaging studies may be warranted if there is uncertainty about the diagnosis or if the mass is rapidly growing, is not located in the midline or has an atypical appearance, especially in the context of heavy tobacco use and/or alcohol intake. Therefore, if referral is warranted, a computed tomography (CT) scan of the facial bones (mainly maxilla) is the preferred method. The investigation is also in accordance with the current dental practice guidelines.4
Case continued
As the patient was a heavy smoker, he was deemed an appropriate candidate to be referred for a CT scan. A non–contrast enhanced CT scan of the facial bones, with focus on the hard palate, was performed (Figure 2). The CT scan confirmed the presence of a lobulated bone protrusion along the middle of the hard palate. There was no aggressive periosteal reaction. No associated soft tissue mass was seen. Bony excrescence seen along the inferior cortex of the hard palate with smooth contours (arrows) was classical for ‘torus palatinus’. Incidentally, mucosal thickening was seen involving ethmoid and maxillary sinuses with mucous retention cyst formation in the maxillary antra bilaterally. No aggressive bone abnormality was identified.
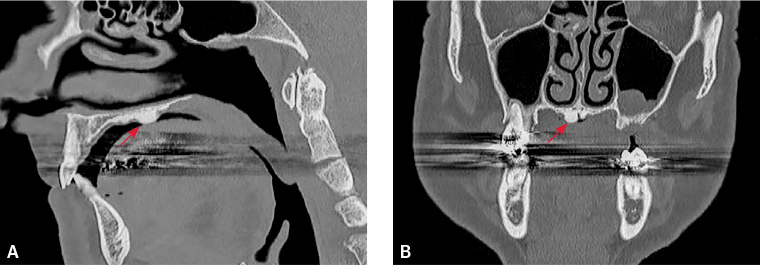
Figure 2. High-resolution computed tomography scan obtained through facial bones and paranasal sinuses; bony excrescence was seen along the inferior cortex of the hard palate with smooth contours (arrows).
A. Sagittal reformat; B. Coronal reformat
Question 3
What are the management options?
Answer 3
Torus palatinus has a benign and localised nature.5 However, since a thin layer of mucosa covers the bony overgrowth, the lump is prone to lacerations and may trap food, thus increasing the aspiration risk if it gets larger.6
Indications for surgical management are limited to issues with speech or prosthodontic management. Referral should be made to a maxillofacial surgeon for the removal procedure. If a maxillofacial surgeon is not available, referral to an otolaryngologist can also be considered.
If the patient is asymptomatic, they can be managed expectantly with monitoring of any changes.
Case continued
The patient preferred watchful waiting. He was advised to present if he noticed any changes or had further concerns, at which time specialist referral could be made.
Question 4
What is the outlook for living with this condition?
Question 5
If removal surgery is required, what are the potential complications?
Answer 4
Tori are genuinely benign. Globally, prevalence of torus palatinus varies from 8% to 51% in various populations.7 On the palate, the exostoses occur posterior to the midline and tend to be noticeable only by the third decade. Tori are seen more frequently in middle-aged adults, with torus palatinus being more common in females than males. In the case of the torus mandibularis, the tumour presents in the lingual aspect of the mandible, opposite the mental foramen.8 It has been observed that certain ethnic groups might be more prone to having tori.9
Prognosis depends on the background aetiology. The aetiologies behind tori are mostly unknown, although a role for genetic factors has appeared in the literature. Despite having a hereditary component, this does not account for all cases of tori. A few rare pathologies, such as superficial injuries or palate stress from mastication, have also been cited in the literature.5,6 Regular clinical photography of the lesion by the patient and/or general practitioner would help in monitoring the changes.
Answer 5
Excision is rarely necessary. Intra-oral complications include perforation of the nasal cavities, palatine nerve or arterial damage, or fracture of the palatine bone. Post-operative complications are similar to any other surgery and may include haematoma, surgical-site infection, poor scarring or dehiscence.9
Key points
- It is necessary to reach a diagnosis in every patient with a lump, mass or lesion in the oropharyngeal mucosa or cavity, keeping in mind tobacco use and alcohol consumption as further risk factors for oropharyngeal malignancies.
- The prevalence of torus palatinus varies largely in different populations.
- Tori are benign lesions, and they do not necessarily require any intervention. Annual review of the lesion, or earlier if the patient suspects change, is recommended