Imaging has always had a critical role in facilitating early diagnosis, mapping the extent of injury and planning a return to activity for elite sportspeople. In addition, ‘the athlete’ now represents a large number of the active population; hence, a need for rapid return to activity after an athletic injury is frequently expected in clinical practice. Whenever imaging is considered for a musculoskeletal injury or condition, the indication for the imaging should be derived from a comprehensive patient examination. Sports physicians, general practitioners and physiotherapists – who are often the first respondents in the post-injury scenario – require familiarity with imaging tools and their effective use to expedite management. Presented in this article are common sports injury scenarios with appropriate use of diagnostic imaging for effective management and quick return to activity.
The evolving role of musculoskeletal imaging
At elite events, the past decade has seen sports imaging move from radiology practice to the pitchside. X-ray, ultrasonography and even magnetic resonance imaging (MRI) are now available. This enables quick decision making in a high-stakes scenario regarding whether an injured athlete may continue to compete in a game.1 Ultrasound-guided local anaesthetic injection is used commonly on match days. Management can begin much earlier than if the injured athlete needed to travel to a hospital or imaging clinic.
Many sports medicine physicians are proficient in the interpretation and use of imaging. Musculoskeletal ultrasonography can be described as ‘the stethoscope’ of the sports medicine profession. In this scenario, radiologists can provide further interpretation, a second opinion and an understanding of how a particular imaging modality might add to the diagnostic pathway.2 Radiologists also provide the services of ultrasound-guided and computed tomography (CT)–guided injections, perform arthrogram procedures and interpret imaging modalities including MRI, CT and scintigraphy. Radiologists are involved in research studies featuring athletes as subjects.
Head and spinal injuries are relatively less common but require urgent imaging. This is outside the scope of this article. Imaging in sports injuries is indicated:
- for an uncertain clinical diagnosis
- when clinical ‘red flags’ are present
- when a sinister or systemic abnormality must be excluded
- to evaluate the extent of injury or presence of complications
- to determine the reason for failed treatment
- when objective evidence is required to document the existence, progression or resolution of disease (eg medico-legal situations)
- for preoperative localisation or planning
- for image-guided procedures such as steroid injections and biopsies.
X-rays
Despite the advent of technologies such as CT and MRI, X-ray continues to play a significant part in the diagnosis and management of sports injuries, primarily because of its wider availability, low radiation dose and quick turnaround. When a fracture or dislocation is clinically suspected after a sporting injury, X-ray is an important and quick step to rule out a significant bony injury with displacement. The use of X-rays to rule out subtle bone injury and soft tissue injury is quite limited.
Ultrasonography
Technological advances now allow visualisation of muscular architecture at in-plane resolution under 0.1 mm, which is better than MRI. Ultrasonography offers dynamic muscle assessment as it is fast and relatively inexpensive and allows serial evaluation to follow healing.3 It can be used to perform guided interventions. It is also useful in diagnosing subtle fractures that are not visible on X-ray imaging by revealing cortical discontinuity. Dynamic ultrasonography assessment before and after muscle contraction can depict persistence of fibre disruption after clinical management and rehabilitation. Ultrasonography can also provide a ‘deep palpation’ together with visualisation of the region of clinical interest. Deep palpation adds a visual component to standard clinical tactile palpation, adding depth to the examination.
As ultrasonography is an operator-dependent modality, it is reliant on the skill of the operator. High-resolution ultrasonography is also affected by signal attenuation in deep tissues of patients with a high body mass index.
Ultrasonography has an exciting future as technological advances open new frontiers for diagnosis. Elastography may prove to be a useful tool for detecting subtle changes in muscle, tendon or nerve mechanical properties that occur early in the course of an injury or disorder. Muscle, tendon or nerve stiffness quantification also provides insight into the mechanisms that may underpin treatments and rehabilitation programs and could ultimately assess their efficacy. Other technologies that offer promise for the future include image fusion with CT and MRI, volume scanning that allows panoramic multiplanar imaging similar to CT and MRI, and real-time three-dimensional imaging for dynamic assessment of moving and physiologically-loaded joints.
Magnetic resonance imaging
MRI has become well established as a gold-standard modality for assessment of musculoskeletal abnormalities because of its excellent soft-tissue contrast and multiplanar capabilities (Figure 1). Being extremely sensitive for the presence of bone marrow and soft tissue oedema, MRI can identify the ‘active cause’ of pain.4 This is especially helpful for patients with several findings on a scan. Technological advances have enabled three-dimensional isotropic acquisitions, resulting in high spatial resolution and generation of high-quality multiplanar reformats. At the same time, the negative predictive value of a sensitive imaging modality such as MRI would allow the physician to proceed with manual therapy or another conservative intervention with greater confidence. Administration of intravenous contrast is essential in investigation of suspected inflammatory conditions, infection and musculoskeletal tumours.
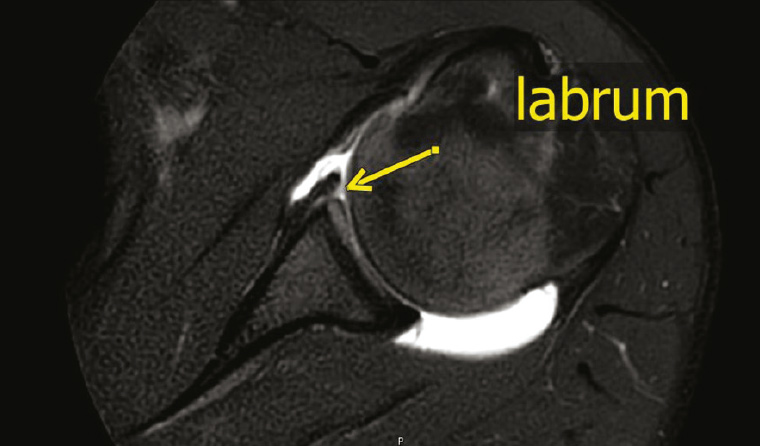
Figure 1. Glenoid labrum can be seen on a magnetic resonance arthrogram of the shoulder
Limited access and complexity of imaging techniques are two factors that contribute to MRI being used after initial evaluation with ultrasonography or an X-ray. Post-injury return to activity and management options are best determined using MRI. In addition, MRI is particularly useful:
- for diagnosis, grading and severity of a muscle/tendon/ligament and bone injury
- to determine the extent and severity of injury for guiding management
- when there is an unclear diagnosis after ultrasonography, an X-ray or CT examination.
Advances in magnetic resonance imaging techniques
Advances in MRI techniques in the research setting have great potential to be applied in a sports medicine setting to provide information on composition, microstructure and function of muscle. Some of these techniques have the potential to assess:
- magnetic resonance spectroscopy to evaluate muscle composition, including assessment of early fatty change, muscle metabolism and force production
- T2 signal mapping to evaluate muscle function, including assessment of recruitment of muscles and their metabolism
- muscle microstructure by evaluating the direction of muscle fibres by using diffusion tensor imaging
- muscle elasticity with magnetic resonance elastography.
Computed tomography scanning
The CT scan is an X-ray–based imaging modality with soft tissue contrast inferior to MRI. However, as a result of relatively easier access and shorter examination time, it can be used for sporting injuries involving bones. The radiation dose has decreased in modern CT scanners. Metal artefact reduction software makes CT scanning the favoured modality in the post-operative scenario. CT is best used for:
- suspected bony injury, where X-ray findings are equivocal
- bone or large soft-tissue injuries, where MRI is not available or contraindicated
- operative planning – in complex fractures, three-dimensional images can also allow for manufacture of dedicated personalised implants.
Image-guided interventions
Musculoskeletal injections were previously delivered ‘blind’ using clinical skills and anatomical landmarks; however, in recent years, ultrasound-guided and CT-guided interventional procedures have become preferred methods because of improved accuracy (Figure 2). The most common procedure is the injection of a mixture of steroid and local anaesthetic for symptomatic relief. This injection also works as a diagnostic procedure to determine whether an abnormality is the cause of a symptom.5
Other procedures that can be performed are aspirations of collections, haematoma and joint fluid. Recently, injections of autologous blood and platelet-rich plasma are becoming popular for the treatment of chronic tendinopathy and osteoarthritis. Prolotherapy involves the injection of an irritant solution into a tendon or ligament, inciting a local inflammatory response that results in fibroblast proliferation and collagen synthesis, to encourage healing and restoration of tensile strength. For osteoarthritis symptom alleviation, intra-articular injection of hyaluronic agent derivatives can be performed. For chronic injuries, trigger point injections can be useful for myofascial pain relief.
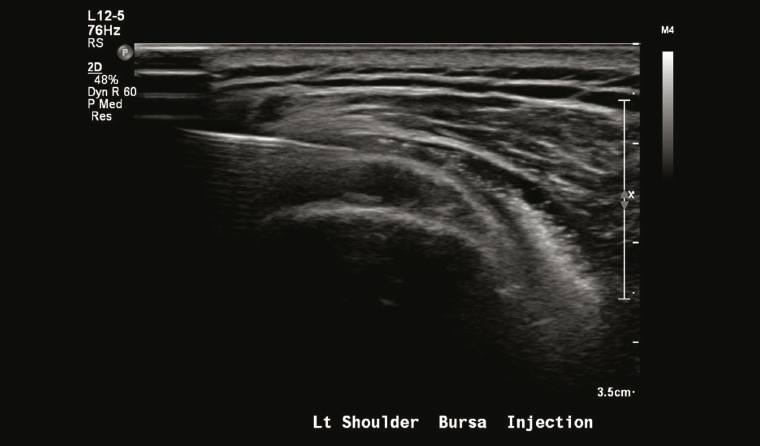
Figure 2. Ultrasound-guided injection into thickened subacromial bursa
Imaging and return to play
Time is precious in professional sport, and a desire for a quick return from injury to avoid missing competition must be balanced with the risk of re-injury. The athlete’s long-term health must be kept in mind.
MRI is considered by some as the main imaging modality in this scenario. Current literature on return-to-play determination is mainly limited to hamstring-related research with a significant interest in the creation of a scoring system that reliably predicts return to play.6 However, to date, no reliable scoring system has been adopted to calculate the exact time of return to play or risk of re-injury. While clinical evaluation must guide the final decision, imaging offers the opportunity to incorporate objective evidence findings into decision making.
Special applications
Cartilage imaging
As a result of its inherently high soft-tissue contrast, MRI is highly sensitive for evaluating chondromalacia (Figure 3) and provides objective measurements of cartilage ultrastructure. In the setting of femoro-acetabular impingement in the hip, MRI can detect surface and basilar delamination.7 MRI aids in preoperative planning for cartilage repair and it is a non-invasive, objective means of long-term post-operative monitoring after cartilage repair. Quantitative MRI techniques that can be used are T2 mapping to assess collagen orientation, delayed gadolinium-enhanced MRI of cartilage and T1rho mapping to assess proteoglycan content.
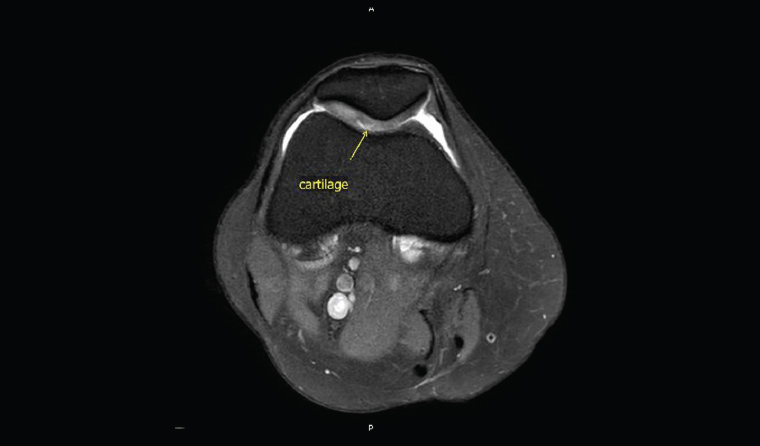
Figure 3. A small focus of chondromalacia can be seen clearly on a magnetic resonance imaging scan.
Physeal imaging
For adolescent athletes, a T1-weighted sequence can be helpful in the evaluation of physeal injury, quantification of the volume of physeal interruption and operative planning. At the elite level, evaluation of distal radius physeal fusion is used for skeletal age evaluation.
Nerve imaging
While sports imaging is focused on soft tissue structures, peripheral nerves are often involved and can be evaluated with MRI. High-resolution ultrasonography can not only depict even the small peripheral nerves in the extremities, but also help to direct appropriate therapy (Figure 4).
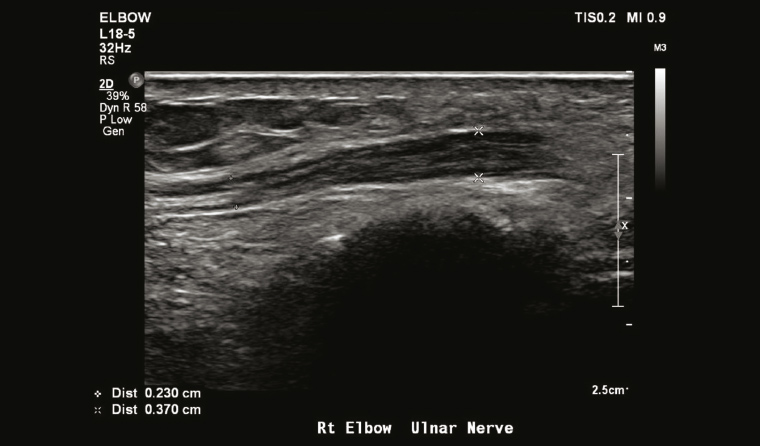
Figure 4. Thickened ulnar nerve in the elbow. Ultrasound-guided injection into the perineural space can be performed for symptomatic relief and to establish a diagnosis of ulnar neuritis.
Differentiating acute versus chronic injury
As a result of its excellent sensitivity to the presence of oedema, MRI can distinguish chronic asymptomatic injuries from acute injuries (eg to determine whether a fracture is chronic or has marrow oedema, which indicates acute injury; Figure 5). Chronic scarring and remodelling with thickening is seen in ligaments with repetitive stress. The presence of oedema in the appropriate clinical setting can help to achieve a diagnosis of acute sprain.
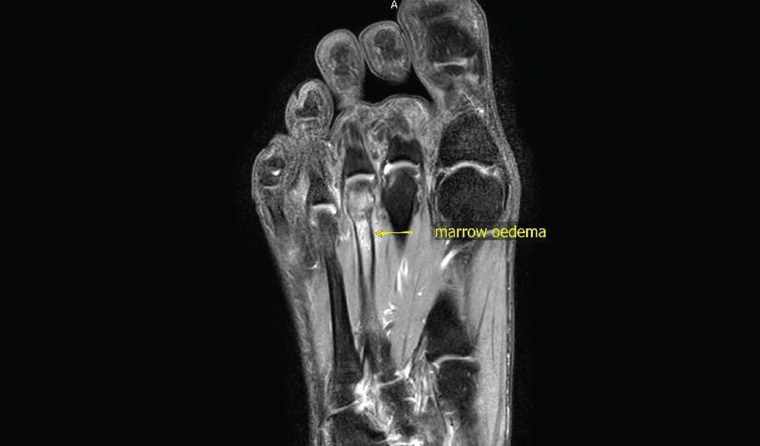
Figure 5. Stress fractures can be better shown on magnetic resonance imaging, especially those inconspicuous on X-ray or computed tomography scans.
Conclusion
While clinical examination remains central to any patient assessment, imaging plays an increasingly important part in the initial evaluation and follow-up of sports injuries. Imaging can assist with appropriate management decisions, return to training and prediction of injury recurrence. Ultrasonography plays an important part in diagnosis as well as guiding interventions. MRI is the current imaging gold standard because of the ability to visualise soft tissues with excellent contrast, high spatial resolution and multiplanar assessment. It is important that sports physicians and musculoskeletal radiologists collaborate for optimal management of injury to an athlete.