Recreational sports participation provides many potential benefits to individuals including improved physiological functioning, social interaction and the promotion of mental health. For the majority of recreational athletes (eg those exercising 45–90 minutes, 2–3 times per week), a dietary intake prioritising whole foods in accordance with the Australian Guide to Healthy Eating1 will be sufficient to meet an individual’s training and competition needs.2 However, when exercise demands increase and/or when dietary intake is restricted, specific nutrition strategies should be implemented to promote favourable training adaptations and optimise competition performance while also supporting health and wellbeing.3
Fuelling for the demands of training
A reciprocal relationship exists between nutrition and intense sports participation: frequent participation in sport can create unique nutritional requirements,3 while attention to the unique nutritional goals of sportspeople can enhance training and promote optimal competition performances. An athlete’s nutritional needs are principally determined by training load (ie intensity, frequency and duration of daily workouts), type of exercise and body mass. However, when immersed in a sport, individuals are often exposed to the dietary ‘norms’ (eg cycling and coffee), sports nutrition products (eg drinks, gels and supplements) and body composition expectations that can ultimately influence dietary intake. When training load changes, current sports nutrition recommendations encourage athletes to manipulate dietary intake to support daily performance and optimise adaptations to daily training.4 Consumer resources to support a ‘food first’ approach to matching energy intakes with increased training loads have been developed (Figure 1).5 These freely available resources encourage manipulation of ‘plate real estate’ to better align daily carbohydrate and energy intake with expenditure, a concept known more recently as ‘fuel for the work required’.6

Figure 1. The Athlete’s Plate nutrition education tool
Developed by Meyer NL with University of Colorado Colorado Springs’ (UCCS) Sport Nutrition Graduate Program in collaboration with the US Olympic Committee’s (USOC) Food and Nutrition Services. Reproduced with permission.
Such resources may be particularly valuable for education of several groups of recreational athletes (eg endurance athletes, athletes in aesthetic sports, athletes in weight-making sports, adolescent athletes) at risk of consuming an inadequate dietary intake to meet the demands of daily training, health and wellbeing.7 Further, some athletes may prioritise nutritional strategies that support leanness over strategies complementing daily fluctuations in training, leaving an individual vulnerable to illness and injury.
Eating insufficiently and sports participation
The concept of ‘energy availability’ is useful for understanding the implications to an athlete of an inadequate dietary energy intake. In simple terms, energy availability (EA) = energy intake – exercise energy expenditure. That is, EA = calories remaining for biological processes once the energy cost of the sporting activity has been subtracted. Sustained periods of low EA (typically considered <30 kcal/kg fat-free mass) or repeated acute (within day) bouts of low EA in very lean individuals can cause impaired physiological functioning, a condition defined as relative energy deficiency in sport (RED-S).8,9 RED-S includes impairments of metabolic rate, menstrual function, bone health, immunity, protein synthesis and cardiovascular health (Figure 2).
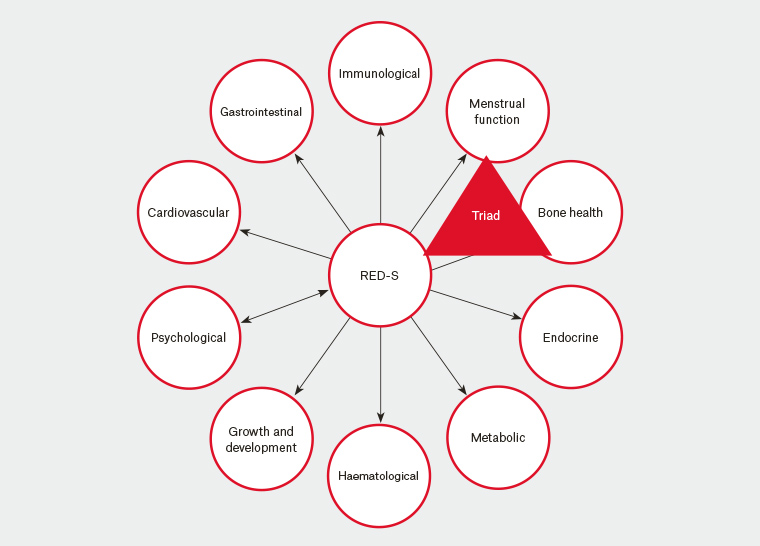
Figure 2. Health consequences of relative energy deficiency in sport (RED-S). ‘Triad’ refers to the female athlete triad.17
RED-S, relative energy deficiency in sport
The impact of RED-S can be significant, and its effects may result in medical presentations with differing signs and/or symptoms. The direct evaluation of RED-S is complicated by the methodological challenges associated with reliably quantifying energy intake, energy expenditure and fat-free mass. For female athletes, irregular or absent menstrual cycles are an obvious clinical indicator of insufficient energy availability. In addition, decreased testosterone/oestrogen and/or thyroid hormone triiodothyronine (T3 ), or an increase in cortisol, offer potential hormonal assessment parameters of RED-S. However, there is no absolute threshold of low EA that results in amenorrhoea in females or low testosterone in males. Therefore, an individual clinical evaluation including discussion of nutrition attitudes and practices, combined with menstrual history for females and endocrine markers for male and female athletes, is suggested.8 In an attempt to simplify the complex clinical assessment and return-to-play decision-making process, the RED-S Clinical Assessment Tool (RED-S CAT)8 has been developed (Table 1). The tool provides a simple evaluation of RED-S risk that is easy to implement, based on three categories: ‘red light’ = cease participation, ‘yellow light’ = compete medical clearance/train under supervision, ‘green light’ = full participation.
| Table 1. The relative energy deficiency in sport decision-based return-to-play model8 |
| High risk: No start red light |
Moderate risk: Caution yellow light |
Low risk: Green light |
- Anorexia nervosa and other serious eating disorders
- Other serious medical (psychological and physiological) conditions related to low EA
- Extreme weight loss techniques leading to dehydration-induced haemodynamic instability and other life-threatening conditions
|
- Prolonged abnormally low percentage body fat measured by DXA or anthropometry using ISAK15 or non-ISAK approaches16
- Substantial weight loss (5–10% body mass in one month)
- Attenuation of expected growth and development in adolescent athlete
- Abnormal menstrual cycle: FHA amenorrhoea >6 months
- Menarche >16 years
- Abnormal hormonal profile in men
- Reduced BMD (either from last measurement or Z-score < −1 standard deviation)
- History of ≥1 stress fractures associated with hormonal/menstrual dysfunction and/or low EA
- Athletes with physical/psychological complications related to low EA/disordered eating, electrocardiogram abnormalities or laboratory abnormalities
- Prolonged relative energy deficiency
- Disordered eating behaviour negatively affecting other
team members
- Lack of progress in treatment and/or non‑compliance
|
- Healthy eating habits with appropriate EA
- Normal hormonal and metabolic function
- Healthy BMD as expected for sport, age and ethnicity
- Healthy musculoskeletal system
|
BMD, bone mineral density; DXA, dual-energy X-ray absorptiometry; EA, energy availability; FHA, functional hypothalamic amenorrhoea; ISAK, International Society for the Advancement of Kinanthropometry
Reproduced with permission of BMJ Publishing Group Ltd from Mountjoy M, Sundgot-Borgen J, Burke L, et al, The IOC consensus statement: Beyond the female athlete triad – relative energy deficiency in sport (RED-S), Br J Sports Med 2014;48(7):491–97. |
Low energy availability in the general practice context
Two of the most likely scenarios associated with low EA in recreational athletes relate to the presentation of individuals with bone stress injuries and/or compromised iron status.
The impact of low EA on bone is pronounced and occurs quickly, particularly in women. Oestrogen-dependent and oestrogen-independent mechanisms that affect bone and are affected by low EA have been clearly identified.10 In early work undertaken by Loucks and colleagues, a short period of low EA (five days) had a negative impact on bone protein synthesis and mineralisation,11 suggesting dietary solutions should be advocated promptly. Given the underlying pathology evolves from the creation of a sustained low EA, an increase in EA should be prioritised.
Regarding iron, the various stages of deficiency for athletic populations are well established (Table 2).12 Prevalence studies indicate that approximately 15–35% of female athletes and 3–11% of male athletes are Stage 1 – Depleted iron stores.
| Table 2. Definition and assessment of stages of iron deficiency12 |
| |
Stage |
| |
1. Depleted
iron stores |
2. Early functional iron deficiency |
3. Iron deficiency
anaemia |
| Description |
Iron stores in the bone marrow, liver and spleen are depleted |
Erythropoiesis diminishes as the iron supply to the erythroid marrow is reduced |
Haemoglobin production falls, resulting in anaemia |
Assessment
|
SF <35 µg/L
Hb >115 g/L
TS >16% |
SF <20 µg/L
Hb >115 g/L
TS <16% |
SF <12 µg/L
Hb <115 g/L
TS <16% |
| Hb, haemoglobin; SF, serum ferritin; TS, transferrin saturation |
Iron studies can be used alongside haemoglobin to assess an athlete’s iron status, as would be done within the sedentary population. However, limitations are associated with the use of ferritin as an indicator of iron status because of its role as an acute phase protein and transient increases during periods of inflammation and following intensive exercise. Furthermore, haemoglobin values are affected by shifts in plasma volume, which, when unaccounted for, may present as pseudo-anaemia. Consequently, a recent review by Sim and colleagues made recommendations for considerations and frequency of iron blood screening for athletes (Figure 3) and identified appropriate strategies to address iron deficiency.13
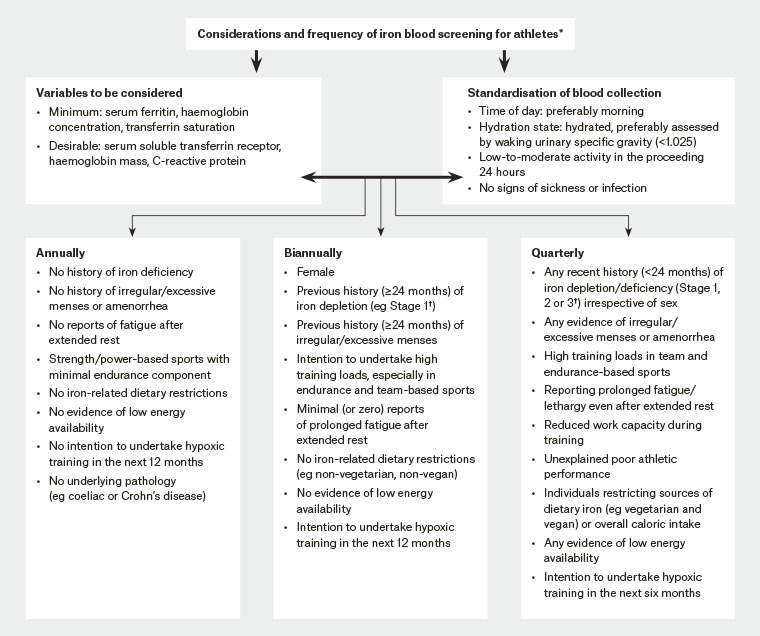
Figure 3. Framework proposing considerations and the frequency of iron blood screening for athletes13
*Use of this framework requires the expertise of trained professionals including a physician, dietitian and sport physiologist.
†Stages of iron deficiency are defined by Peeling et al 2007.12
Reproduced with permission from Sim M, Garvican-Lewis LA, Cox GR, et al, Iron considerations for the athlete: A narrative review, Eur J Appl Physiol 2019;119(7):1463–78, doi: 10.1007/s00421-019-04157-y.
Advice on sports food and supplements
A ‘food first’ policy should be the basis of any athlete’s nutrition plan, as recommendations for dietary supplements typically overemphasise the supplements’ ability to manipulate performance in comparison to other training and dietary strategies. That said, there may be occasions for the prudent use of medical supplements to address nutrient deficiencies, or sports foods that help the athlete to meet nutritional goals when it is impractical to eat food. Supplements and sports foods represent a lucrative industry that takes advantage of strong marketing to athletes and people who exercise while also reflecting the community interest in supplements.
The use of supplements and sports foods by athletes involves a balance between the potential benefits (eg contribution to health and performance) and risks (eg adverse health events, waste of resources, distraction, poor role modelling, supplement contamination). The Australian Institute of Sport has established an independent, evidence-based Sports Supplement Framework (https://ais.gov.au/nutrition/supplements) to support the judicious use of supplements.14
The Framework classifies supplements into four categories (A, B, C and D; Table 3) according to scientific evidence, supporting the use of products that are safe, permitted and effective in improving sports performance.
| Table 3. Overview of the Australian Institute of Sport (AIS) Sports Supplement Framework14 |
| Category |
Description |
Examples |
| A |
Supported for use in specific situations in sport using evidence‑based protocols |
Sports foods/drinks
Medical supplements
Performance supplements |
| B |
Deserving of further research and could be considered for provision to athletes under a research protocol or case-managed monitoring situation |
Collagen support products
β-Hydroxy β-methylbutyrate (HMB)
Quercitin
Ketone supplements |
| C |
Have little meaningful proof of beneficial effects |
Any supplement not listed in A, B or D categories |
| D |
Banned or at high risk of contamination with substances that could lead to a positive drug test |
Stimulants
Prohormones and hormone boosters
Growth hormone releasers and ‘peptides’
Beta-2 agonists
Selective androgen receptor modulators
Metabolic modulators |
Performance-based supplements (Category A) include caffeine, bicarbonate, beta-alanine, nitrate, creatine and glycerol; however, their value is specific to particular event characteristics (eg repeated sprint ability). Supplement considerations may also extend to athletes undertaking travel or competing in challenging environments (eg heat and altitude), and individuals with restricted dietary choice (eg vegetarians). Ideally, each athlete should develop a personalised, periodised, and practical nutrition plan – via collaboration with their coach and accredited sports nutrition expert – to optimise their performance. The Sports Dietitian Australia website is useful to locate the nearest sports dietitian, and in addition provides many free evidence-based sports nutrition resources (www.sportsdietitians.com.au).