The complexity of tests, treatments and procedures in modern medicine is at an unprecedented level. Unnecessary practices and frequent and invasive investigations are potentially costly to the healthcare system, may divert away from effective care and can potentially expose the patient to undue risk of harm, emotional stress or personal financial costs.1
Paediatric and adolescent gynaecology is a unique sub-speciality that falls under the domain of general practitioners (GPs), gynaecologists, paediatricians and emergency physicians. During medical training, this sub-speciality is frequently not covered in depth, and exposure to this area can be limited post-fellowship. It has been shown that history taking and diagnostic ordering for adolescent females presenting with heavy menstrual bleeding (HMB) is inconsistent and inadequate.2
This has been suggested to contribute to clinicians ordering investigations overcautiously. The resultant increase in patient (and parental) anxiety, which is not uncommon in this patient demographic, is considerable.
Abnormal uterine bleeding (AUB) refers to any variation from a normal menstrual cycle. It includes HMB and irregular bleeding, which together account for up to half of adolescent gynaecology visits.3 HMB in this age group is almost invariably due to an immature hypothalamic–pituitary–ovarian axis, which is reflective of the pubertal transition. The physiological maturation of this axis can persist for up to 5–8 years post-menarche.4,5 This differs from the causes and management of HMB in older women of reproductive age, which are more likely to be related to structural causes. A retrospective review of 230 adolescents at a paediatric hospital in Canada showed that 67.8% of all patients referred with AUB had pelvic ultrasonography performed as part of their initial workup, and ‘no patient had a change in her AUB management due to ultrasound findings’.6 Unfortunately, unnecessary ordering of pelvic ultrasonography for AUB in adolescent females is common.
In Australia, 14.9% of GP encounters with female patients aged <25 years are for women’s health problems, compared with 12% for women of any age.7 The majority of these patients are managed solely by GPs, with referral to a gynaecologist occurring at a rate of 0.8 per 100 GP–female patient encounters.8 In Victoria, Tasmania and southern New South Wales, a significant proportion of adolescent females referred to a gynaecologist are seen at the Royal Children’s Hospital (RCH).
This study was designed to review all new referrals to gynaecology for female adolescents with HMB from 1 January 2017 to 31 December 2017, to identify whether or not pelvic ultrasonography had been arranged prior to a referral. It was hypothesised that pelvic ultrasonography was frequently being ordered in the initial work-up of female adolescents with HMB. It was also predicted that these ultrasounds would predominantly not alter management and therefore could potentially be avoided, thereby reducing patient anxiety and healthcare costs on unnecessary investigations. The purpose of this review was to enable targeted education to relevant medical professionals, thereby attempting to prevent unnecessary investigations in this context.
Method
This audit of adolescent females presenting with HMB was a pragmatic retrospective observational study. All female patients ≤18 years of age who had been referred to RCH for the management of HMB during the study period were identified through the gynaecology outpatient database. Medical records of all patients fulfilling inclusion criteria were reviewed.
Medical records were reviewed to determine if pelvic ultrasonography was ordered during the diagnostic process. If ordered, the reviewed information included: the indication, ordering health professional and whether the ultrasound result altered clinical management. Data were extracted from RCH records, collated and de-identified. The RCH imaging database was also reviewed to cross-correlate findings and to ensure accuracy and completeness.
Human research and ethics committee (HREC) permission to undertake this audit was obtained (HREC Reference Number: LNR/18/RCHM/218; SSA Reference Number: LNRSSA/18/RCHM/219; RCH HREC Reference Number: 37332A).
Results
During the study period, 541 new referrals were received by the RCH gynaecology department. Eighty-two of these were for female adolescents with HMB (15.1%). Approximately half of these referrals came from GPs (n = 43), with the remainder being referred from paediatricians either at RCH (n = 27) or within the community (n = 6), emergency physicians at RCH (n = 5) or adult physicians in the community (n = 1). Figure 1 illustrates this.
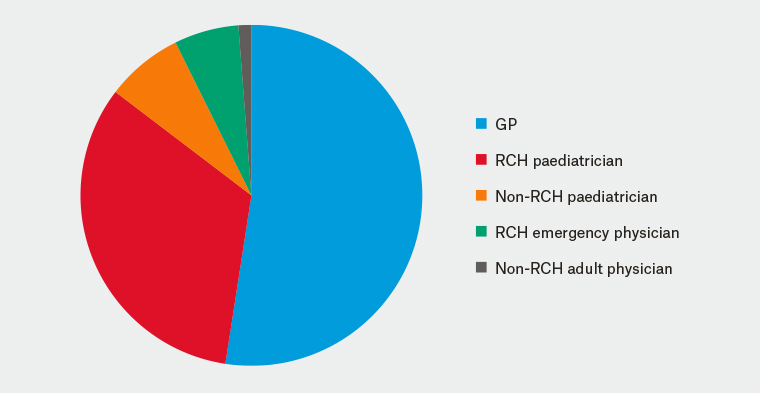
Figure 1. Referral source of adolescents with heavy menstrual bleeding being referred to the Royal Children’s Hospital
GP, general practitioner; RCH, Royal Children’s Hospital
Approximately one-third of these patients had undergone pelvic ultrasonography prior to referral. RCH practitioners were the least likely to have ordered pelvic ultrasonography. Only one patient referred from an RCH paediatrician underwent pelvic ultrasonography prior to referral to gynaecology. No referrals from the RCH emergency department had an ultrasound. Fifty-three per cent of patients being referred from their GP had undergone ultrasonography (n = 23). Community physicians, compared with RCH physicians, were more likely to organise ultrasonography prior to referral (1/1 referral from a community adult physician and 2/6 referrals from non-RCH paediatricians had an ultrasound accompanying the referral). This is illustrated in Figure 2.
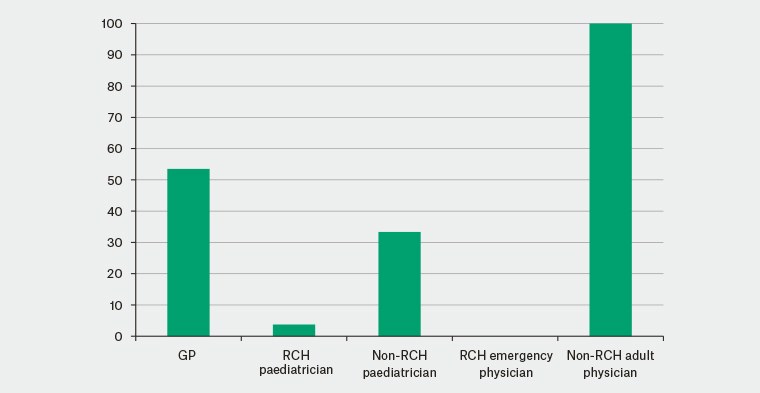
Figure 2. Percentage of new referrals in which the patient has undergone pelvic ultrasonography prior to the Royal Children’s Hospital gynaecology review
GP, general practitioner; RCH, Royal Children’s Hospital
Of the 27 ultrasounds accompanying an initial referral, no ultrasound had an abnormal result that changed management of the patient’s HMB. Two ultrasounds identified pathology. One had a 5 cm incidental physiological cyst that resolved within three months. The second had an endometrial thickness of 23 mm, which resolved with management of the HMB.
Discussion
Over the study period, one in eight referrals to RCH gynaecology was for HMB. The majority of patients were referred from GPs, which likely reflects the preponderance of female adolescents being managed in the community.
The frequency of ordering pelvic ultrasonography for adolescents with HMB is greater for clinicians working external to RCH. This may reflect greater autonomy of clinicians in the community, more frequent discussion and informal referral to adolescent gynaecology within a hospital setting and/or greater exposure to adolescent gynaecology teaching at RCH.
None of the ultrasounds ordered had pathology that changed clinical management. This is reflective of the physiological state of adolescents in the peri-pubertal period, and further evidence that structural causes are extremely rare in this population. This is consistent with the literature3–5 and is the basis for the recent recommendations that routine ultrasonography should not be obtained solely for the work-up of HMB in adolescents.9 If HMB persists post–gynaecological maturation, which can be up to eight years post-menarche, or if initial management of HMB is unsuccessful, ordering pelvic ultrasonography may be required.6,9,10
Strengths of this analysis include that this study analyses contemporary data from a large tertiary paediatric and adolescent hospital, which receives referrals from a large majority of the southern states of Australia. It is consistent with international data.3,4,6,9,10 To the researchers’ knowledge, this is the first study to analyse unnecessary investigation ordering within a community versus hospital setting, which may be the result of inexperience and inadequate knowledge of paediatric and adolescent gynaecology. Finally, medical records were examined by one researcher and all relevant data were able to be collected from the records, thereby eliminating the risk of bias due to incomplete records.
There are several limitations to a retrospective observational study, including the quality of data analysed being limited to what has been documented in the medical records, absence of data from patients presenting at other hospitals – of which the data in this study may not be representative – and the small numbers of patients, which may limit generalisability of the results.
Conclusion
Paediatric and adolescent females referred to RCH are frequently undergoing unnecessary pelvic ultrasonography as a first-line investigation. Education targeted to health professionals managing female paediatric and adolescent patients, especially those within community settings, is recommended to reduce unnecessary ordering and the associated patient and parental anxiety associated with these investigations.