Approximately 15% of couples will experience infertility.1 By definition, this is the failure to achieve pregnancy within 12 months of regular unprotected intercourse in a woman aged <35 years or within six months in a woman aged >35 years.2
It is appropriate to perform an assessment of both male and female fertility factors at these junctures. Additionally, it would be prudent to undertake assessment in advance of these defined time points when there are factors on clinical assessment that could increase the risk of subfertility. These include oligomenorrhea; amenorrhoea; known or suspected uterine, tubal or peritoneal disease; severe endometriosis; multiple surgeries to the ovary or loss of one ovary; and previous chemotherapy or radiotherapy treatment.3,4 Known or suspected male subfertility should also prompt evaluation.4
The initial evaluation should comprise history-taking and examination focused on reproductive history factors and assessment of antenatal risk. A structured approach to initial reproductive history-taking is outlined in Box 1. The examination should include an assessment of body mass index and blood pressure, a focused examination of the thyroid and breasts, and auscultation of the heart sounds. An abdominal and/or pelvic examination may be indicated on the basis of the presenting history and to complete cervical or infectious screening.
| Box 1. Systematic approach to female reproductive history |
Duration of infertility
- Frequency and timing of intercourse
- Sexual dysfunction
Gynaecological and obstetric past history
- Cervical screening results, previous treatments
- Previous pregnancies: time to conceive, management of early pregnancy loss and termination, mode and timing of delivery and antenatal, intrapartum or post-partum complications
- Pelvic infection
- Menstrual history: cycle interval, duration of bleeding and associated abnormal uterine bleeding and dysmenorrhoea
- Dyspareunia
Previous medical history
- Medical comorbidities: management and stability
- Previous surgery
Medications, including any allergies
- Past and present medication use
- Previous contraceptive use
- Vaccination history: rubella, varicella, hepatitis B, influenza
- Folic acid and iodine supplementation
Family history
- Heritable conditions
- Premature ovarian insufficiency
Social history
- Smoking, alcohol and recreational drug use
|
Ovulation
Ovulatory cycles are indicated by a history of regular cycle intervals of between 21 and 35 days with consistent characteristics and moliminal symptoms. Serum progesterone is not required to confirm ovulation when cycles are regular in frequency and character. If there is uncertainty, serum progesterone is confirmatory, provided that it is performed in the mid-luteal phase (ie seven days before the next expected menses). This may require serial progesterone levels to be performed for patients with minor inter-cycle variation.1
A clinical history consistent with anovulation requires further evaluation. A history of weight changes, stressors, hot flushes, visual disturbance, galactorrhoea or clinical hyperandrogenism may assist in delineating the cause of anovulation. Anovulation may be classified using the World Health Organization classification system (Table 1).5–7 Accordingly, investigation of oligomenorrhoea or amenorrhoea should include follicle-stimulating hormone (FSH), luteinising hormone and oestradiol (E2) in addition to thyroid stimulating hormone and prolactin concentrations. The recent international consensus guidelines for the assessment and management of polycystic ovarian syndrome (PCOS) endorse the Rotterdam criteria for diagnosis.8 Biochemical hyperandrogenism should be assessed using calculated free testosterone, free androgen index or calculated bioavailable testosterone using a liquid chromatography mass spectroscopy assay. Androstenedione and dehydroepiandrosterone may be considered for patients with normal testosterone. Given that PCOS is a diagnosis of exclusion, it is important to exclude non-classical congenital adrenal hyperplasia with a 17-hydroxyprogesterone concentration, which tests for the most common enzymatic deficiency in 21-hydroxylase. Exclusion of Cushing’s disease also requires consideration, particularly when there are severe features of hyperandrogenism.8
| Table 1. World Health Organization classification of anovulation5–7 |
| Group |
Classification |
Causes |
Group 1
|
Hypogonadotropic anovulation
|
Hypothalamic amenorrhoea: stress, weight loss, excessive exercise
Hyperprolactinaemia
Primary pituitary disease: infiltrative disease, central nervous system tumour
Congenital gonadotropin-releasing hormone deficiency |
Group 2
|
Normogonadotropic anovulation |
Polycystic ovary syndrome
Congenital adrenal hyperplasia |
| Group 3 |
Hypergonadotropic anovulation |
Premature ovarian insufficiency |
Ovarian reserve testing
Both oocyte quantity and quality are important factors for successful conception.
Oocyte number peaks at 20 weeks’ gestation; this is followed by a progressive decline that continues throughout reproductive life until a critical threshold is reached, resulting in menopause.9,10 Evaluating markers of ovarian reserve attempts to quantify the size of the remaining follicular pool as a surrogate for fertility. Routinely performed markers of ovarian reserve include day 2–4 FSH and E2, anti-Müllerian hormone (AMH) and assessment of antral follicle count (AFC) on transvaginal ultrasounds.10 No marker is directly able to measure the size of the primordial follicle pool. Ovarian reserve testing is an important component of an infertility assessment, and it provides information regarding the predicted ovarian response to assisted reproductive treatment (ART). However, caution should be exercised when performing the investigation outside this setting as it is not predictive of spontaneous conception and therefore interpretation is problematic.
A basal (day 2–4) FSH concentration is an indirect marker of ovarian reserve based on feedback inhibition of pituitary FSH secretion. In the case of diminished ovarian reserve, ovarian steroidogenesis will be insufficient to suppress early follicular FSH. A simultaneous measurement of serum E2 concentration should be performed, as this increases the sensitivity of FSH testing to assess ovarian reserve. Elevation in basal E2 concentration occurs in diminished ovarian reserve secondary to increased early follicular FSH but results in suppression of pituitary FSH secretion and an FSH concentration that falls within the normal range. An FSH concentration of >10 IU/L has high specificity for poor ovarian response to controlled ovarian hyperstimulation in women undergoing ART (≤4 oocytes retrieved at egg collection) but is poorly sensitive. Sensitivity is even poorer for predicting conception, and FSH demonstrates significant intra- and inter-cycle variation. Interpretation also requires intact function of the hypothalamic–pituitary–ovarian axis, which limits clinical application.10–12
AMH is produced by the granulosa cells of the pre-antral and antral follicles, thereby reflecting the size of the primordial follicle pool.13 Serum AMH concentration is inversely related to female age and shows minimal variation both within and between cycles. Therefore, testing on any day of the menstrual cycle is appropriate.10 Results will often be reported as the absolute number as well as the centile in relation to female age, which assists interpretation. Elevated AMH is predictive of an excessive response to controlled ovarian hyperstimulation during ART, while low AMH is predictive of an increased risk of poor ovarian response.14,15 For women attempting spontaneous conception, AMH correlates poorly with fecundity.16
AFC is the total number of follicles in both ovaries with a mean width measurement of 2–10 mm on ultrasound assessment. Although it is possible to count throughout the menstrual cycle, assessment in the early follicular phase avoids underestimation of follicle number due to the presence of a corpus luteum or large dominant follicle. Ultrasonography is an operator-dependent technique; therefore, AFC may vary between operators and be influenced by other imaging factors such as machine resolution and patient body habitus. Antral follicle number >15 or <3–7 predicts hyper response and poor ovarian response, respectively, but correlates poorly with pregnancy.15,17
Pelvic anatomy and tubal patency
Transvaginal pelvic ultrasonography is an important component of female fertility assessment. In addition to assessing the AFC, it allows for assessment of the uterine anatomy and structure and mobility of the pelvic organs.
Uterine polyps, fibroids and abnormalities of the Müllerian tract may be detected on transvaginal ultrasounds with or without saline infusion. Venetian blind shadowing, globular uterine appearance, loss of junctional zone definition and ‘question mark sign’ are all sonographic features associated with adenomyosis (Figure 1).18 Endometriosis may be diagnosed using ultrasonography in the hands of an experienced operator. Limitation in mobility of the adnexal structures and/or specific probe tenderness may indicate superficial endometriosis or other pelvic pathology associated with adhesion formation. Direct visualisation of nodules and endometriomas (Figure 2) and absent sliding of the rectum against the uterus are features of deep infiltrating disease. In addition to guiding a presumptive diagnosis, ultrasonography assists in surgical planning for women with deep infiltrating disease, particularly with regard to bowel involvement.19 Any of these findings may affect oocyte capture to the fallopian tube; fallopian tube structure, patency and transport; successful implantation and ongoing pregnancy.
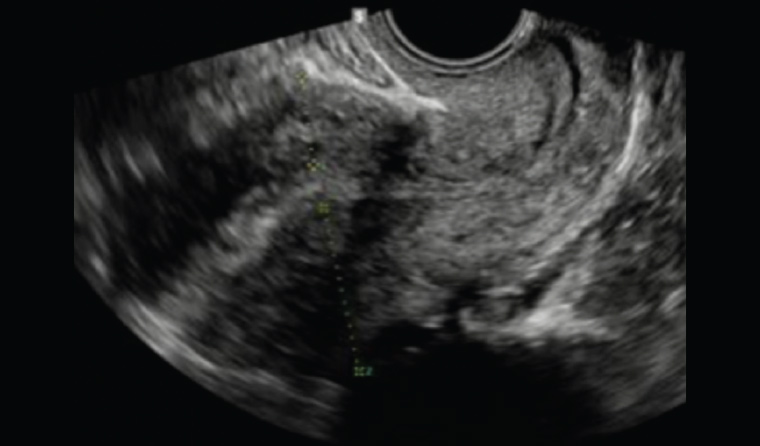
Figure 1. Pelvic ultrasound with features suggestive of adenomyosis: heterogeneous myometrium and ‘venetian blind’ artefact
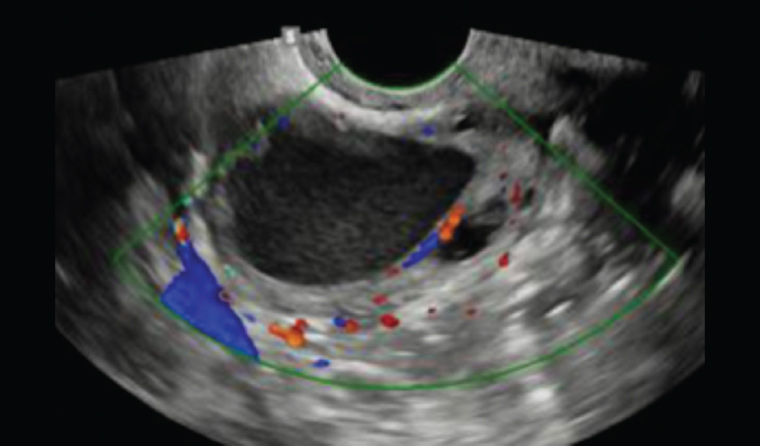
Figure 2. Pelvic ultrasound showing typical ‘ground glass’ appearance of an endometrioma
Tubal patency may be assessed using hysterosalpingography, hysterosalpingo-contrast sonography or hydrotubation at laparoscopy. Tubal patency testing may also be combined with a therapeutic intervention such as flushing with oil-based contrast, which may increase conception in the following six months when compared with flushing with water-based contrast.20,21 An assessment of tubal patency is generally considered following preliminary fertility investigations (Box 2) including semen analysis, and the modality is decided on the basis of the suspected cause of infertility, concurrent symptoms, anticipated treatment and predicted risk of tubal disease.
| Box 2. Preliminary fertility investigations |
Day 2-4 follicle-stimulating hormone, luteinising hormone, oestradiol
Anti-Müllerian hormone
Thyroid stimulating hormone
Transvaginal ultrasonography of the pelvis: antral follicle count, pelvic anatomy and features of deep infiltrating endometriosis
Blood group and antibody screen
Full blood examination
Rubella, varicella immunoglobulin G
Hepatitis B, hepatitis C, human immunodeficiency virus and syphilis serology
Genetic carrier screening if desired: thalassaemia, triple screen (fragile X syndrome, cystic fibrosis, spinal muscular atrophy), extended carrier screen |
Preconception screening
Women presenting for assessment should have serology performed for rubella and varicella immunoglobulin G (IgG) at a minimum. This allows for vaccination of susceptible women prior to pregnancy, although women should be told to defer conception for at least 28 days post-vaccination.22 Additionally, serology testing for hepatitis B, hepatitis C, human immunodeficiency virus and syphilis may be performed, as these form part of the routine antenatal investigations. Performing these tests prior to conception allows for appropriate pre-pregnancy counselling to take place and any infectious conditions to be optimised to reduce maternal and fetal risk.23
Genetic carrier screening should also be discussed and offered to all women contemplating pregnancy.24 Thalassaemia screening with a full blood examination is a component of routine antenatal screening. Further haemoglobin electrophoresis and DNA studies may be indicated on the basis of results (red cell indices), family history or high-risk ethnic group. Screening panels are now available to simultaneously test for carriership of common genetic conditions. Limited panels test for the three most common conditions: spinal muscular atrophy, cystic fibrosis and fragile X premutation. Extended panels offer testing for hundreds of genetic conditions, including both autosomal and X-linked recessive inheritance, with a single test. Given the high likelihood of carriership detection for one or more conditions in any individual undertaking an extended panel, pre- and post-test counselling is essential, and the advantages and disadvantages of sequential or simultaneous screening of the couple should be discussed.25
Assessment of fertility for women considering oocyte cryopreservation
Age is the most important determinant of female fertility. In Australia, the average age of women at first birth in 2015 was 28.9 years, compared with 28.1 years in 2005; the proportion of births to mothers over the age of 35 years was 22%.26 On a societal level, the shift towards delayed childbearing has led to a decrease in total fertility rate.27
Infertility is most prevalent in women aged >35 years and results in significant burden of disease.28
The advent of vitrification technology means that cryopreserved oocytes have survival rates >84% and comparable in vitro fertilisation outcomes to fresh oocytes.29 Increasingly, women are considering elective oocyte cryopreservation to allow an opportunity to conceive biologically related children at a later age.30
An appropriate preliminary assessment for a woman considering elective oocyte cryopreservation would include systematic history-taking and examination as outlined in Box 1 and investigations as outlined in Box 2. This provides valuable information for the assessment of medical comorbidities and forms the basis for counselling regarding the risks and benefits of elective oocyte cryopreservation and the expected response to controlled ovarian hyperstimulation. The ideal age to freeze oocytes is prior to 35 years of age, as poorer pregnancy outcomes related to deteriorating egg quality are achieved from oocytes vitrified after the age of 35 years.27
Conclusion
A comprehensive assessment of female fertility aims to determine underlying causes of subfertility, provide an opportunity for pre-pregnancy screening and counselling, and offer genetic screening options. Assessment of ovulatory function, ovarian reserve and pelvic anatomy provide a basis for further tailored investigations and infertility management.