The carpometacarpal joint (CMCJ) of the thumb is one of the joints most commonly affected by arthritis.1 It plays an important part in the positioning of the thumb in space to allow important activities of daily living. It is integral to fine motor activities such as pinch, key and chuck grips as well as having an important role in power grips.2,3 CMCJ osteoarthritis is more common in post-menopausal women, who make up approximately 80% of the patient population. The dominant hand is involved in 60–65% of cases.2,4
Anatomy/pathophysiology
The thumb CMCJ is a biconcave–convex saddle joint that allows flexion/extension, adduction/abduction and limited rotation through the joint. There are 16 ligaments that have been described that help stabilise the joint. The most important of these ligaments appears to be the deep anterior oblique ligament. Attrition ruptures of this ligament have been postulated to initiate changes in the biomechanics that eventually lead to arthritis of the joint.5 Furthermore, CMCJ morphology itself may have a part to play in the development of arthritis within this joint. Studies by Eaton and Littler as well as Aune have reported shallower trapezial articular surface morphology in women when compared with men, which may explain the higher incidence of CMCJ osteoarthritis in women.6
Classification
Eaton and Glickel proposed a staging system for CMCJ osteoarthritis and provided a treatment rationale on the basis of this classification. This classification is commonly used and separates the condition into four stages. The early stages (I/II) are more amenable to non-operative treatment modalities, whereas the latter stages (III/IV) are associated with significant progression of arthrosis and are more responsive to surgery (Table 1; Figure 1).7,8
| Table 1. Eaton classification of basilar thumb arthritis7 |
| Stage |
Features on plain radiographs |
| Stage I |
Articular contours normal. Slight widening of joint space on X-ray. |
| Stage II |
Slight narrowing of joint space. Osteophytes ≤2 mm. Scaphotrapezial joint normal on X-ray. |
| Stage III |
Marked narrowing of joint space with cysts and sclerosis. Osteophytes >2 mm. Scaphotrapezial joint normal on X-ray. |
| Stage IV |
Stage III changes with associated scaphotrapezial joint involvement. |
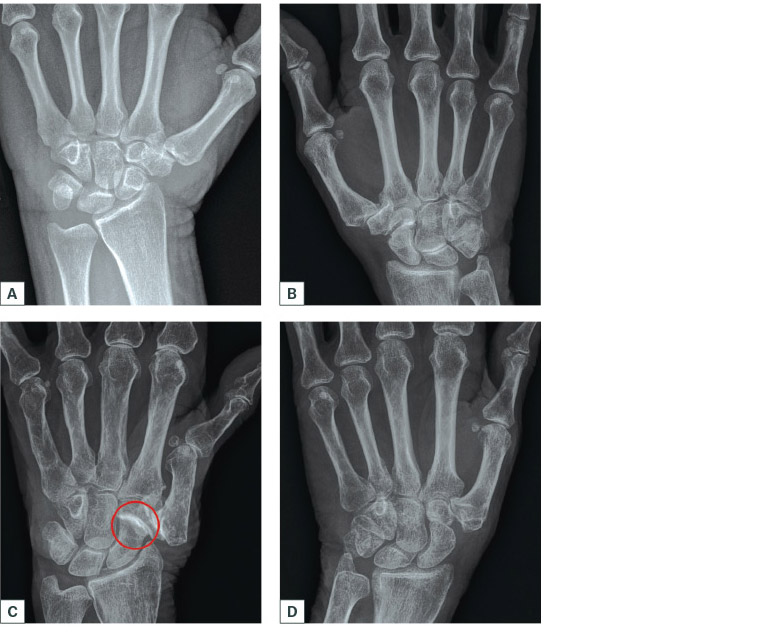
Figure 1. Different radiographic stages of basal thumb arthritis
A. Stage II with small osteophytes (≤2 mm) and preservation of joint space; B. Stage III medial osteophytes >2 mm, complete loss of joint space and joint subluxation; C. Stage IV arthritic involvement of the scaphotrapeziotrapezoidal joint (circle); D. Radiograph post-trapeziectomy with ligament reconstruction and tendon interposition
Non-operative management
The aim of non-operative management of basal thumb arthritis is to restore thumb functionality by treating pain and improving stability, mobility and strength. Engagement with non-operative strategies should be undertaken for a minimum of six months. Failure to achieve pain relief, improve occupational performance and enhance quality of life with conservative strategies necessitates consideration of surgical intervention.
Hand therapy
The mainstays of therapist-led conservative management for thumb CMCJ osteoarthritis are education, orthotics and exercise.9 Specialised occupational therapists or physiotherapists work in collaboration with medical practitioners and the patient to achieve these goals.
Education
Education regarding assistive equipment, pain management, activity pacing, joint protection and support services (eg Arthritis Australia and Independent Living Centres) is also important.9 The efficacy of education has been established by Dziedzic et al, who compared the pain and disability states of patients who either received or did not receive a program incorporating joint protection, pain management and energy conservation education.10 The rationale for providing this education is to optimise joint congruency during functional use, decrease inflammation, decrease pain and increase independence, which also optimises the patient’s psychological response to their condition.11
Orthoses
International guidelines recommend the provision of orthoses for patients with osteoarthritis of the first CMCJ.12 An orthosis that supports the first CMCJ in palmar abduction is recommended as it facilitates the inherent stability provided by the joint surfaces while maximising the thumb web space (Figure 2).13 Effective pain management can be achieved if the splint is worn for longer than three months. Even if only worn at night, the splint can provide daytime pain relief.14

Figure 2. Examples of opponens splints that help support and position the thumb in a position of function within the hand
A. & B. Long splints; C & D. Short splints
Exercises
Exercise programs that focus on stabilising the first CMCJ, increasing pain-free thumb joint range of movement, and general body conditioning have been recommended by recent international guidelines.12 The rationale for stabilisation exercises (ie those that strengthen the muscles that abduct and oppose the thumb and the first dorsal interossei) is to counteract the destabilising force of the thumb adductor at the first CMCJ.13 Exercises must be tailored to the individual to ensure they do not increase joint stress or exacerbate deforming forces.
Other modalities
As a result of weak evidence, the use of warmth/cold was not included as a recommendation in the current international guidelines.12 However, it was noted that using warmth may assist in decreasing pain and improving joint motion. Conversely, during osteoarthritic flares, cold packs may be used to achieve the same effect.9,15 There is limited literature exploring the efficacy of compression gloves in the management of osteoarthritic pain, oedema and stiffness. Recommendations are based on expert opinion, but gloves may be used in an attempt to control symptoms.16
Intra-articular injections
A systematic review of the literature looking at the benefits of intra-articular injections of either corticosteroids or hyaluronate showed mixed results. Although most of the randomised controlled trials (RCTs) showed some benefit of intra-articular injections, the duration and efficacy of symptom improvement when compared with placebo was variable. The mechanism of action of each differs, with corticosteroids modulating the inflammatory process while hyaluronate restores the reduced viscoelasticity of the synovial fluid. Overall, there is evidence that intra-articular injections improve the pain profile, with hyaluronate being more effective and longer lasting than corticosteroids.17
Operative management
With more advanced disease or failure of non-operative management, surgical strategies can be considered. The goal of surgical intervention is to eliminate pain and restore hand function while maintaining stability and mobility.2 There is strong consensus that the removal of the arthritic articular surfaces of the thumb CMCJ is associated with good clinical outcomes.4 A range of surgical options are available to achieve this goal. These can be broadly divided into two categories: non-implant and implant-related procedures. Non-implant procedures include trapeziectomy with or without tendon interposition, suture suspension, arthroscopic procedures, metacarpal osteotomies and joint fusion. Implant-related procedures include all surgical options where implants (cobalt chrome, titanium, pyrocarbon, silicon) are used to replace or recreate the joint articulation similar to knee or hip joint replacements.2,8
Trapeziectomy with or without ligament reconstruction and tendon interposition
Trapeziectomy alone was the standard operative treatment for many years. However, concerns about longitudinal collapse of the thumb ray affecting grip and pinch strength resulted in the development of alternative surgical techniques.1 Trapeziectomy with ligament reconstruction and tendon interposition (T-LRTI), first popularised by Burton and Pelligrini, has become the most commonly performed procedure (Figure 3).1,4,8 Case series looking at medium- to long-term results show 95% satisfaction rates, with good pain relief and improved range of motion and grip strength. T-LRTI has become the standard by which other treatment modalities are measured.4 However, there is a small incidence of complications associated with the procedure; graft harvest morbidity, wound irritation, flexor carpi radialis tendonitis and complex regional pain syndrome have been reported.1 Randomised studies comparing these two techniques have failed to find any statistically significant advantage of T-LRTI over trapeziectomy alone.4
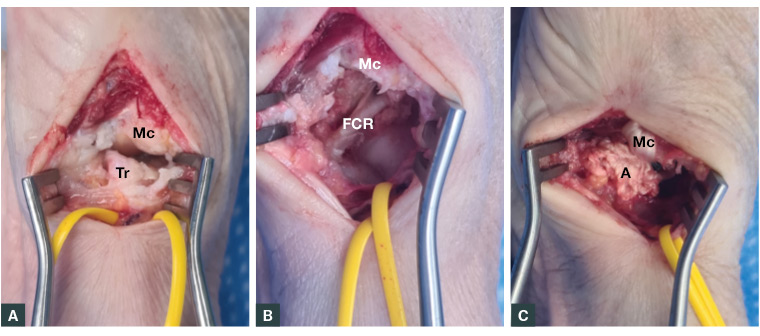
Figure 3. A. Arthritic thumb carpometacarpal joint (Mc – metacarpal; Tr – trapezium), vessel loop around radial artery; B. Post-trapeziectomy flexor carpi radialis in floor (Mc – metacarpal; FCR – flexor carpi radialis); C. Post–ligament reconstruction and tendon interposition (Mc – metacarpal with flexor carpi radialis sling; A – anchovy made from flexor carpi radialis tendon)
Tightrope suture suspension
To minimise graft harvest morbidity, other surgical techniques such as suture suspension and tightrope stabilisation have been described. The suspension of the thumb metacarpal base to the index metacarpal base is achieved by using a synthetic ligament secured and tightened over buttons. There is an overall improvement in pain and functional scores with this technique. Complications such as superficial wound infections, pain with over tightening, fracture and complex regional pain syndrome have been documented.18
Arthroscopic procedures
With recent advances in arthroscopic techniques, minimally invasive options for the management of CMCJ osteoarthritis have been described. Arthroscopic partial or total resection of the trapezium, with soft-tissue interposition with varying biomaterials, has been shown to be effective in improving pain, strength, range of motion and functional scores in the short to medium term.19,20 However, failure rates of 20–25% with these techniques have been documented, often requiring revision to T-LRTI.4,19 Further prospective RCTs are warranted to explore the risks and benefits of this technique over others.19
Thumb CMCJ fusion (arthrodesis)
Fusion is an excellent option for the management of thumb trapeziometacarpal arthritis. It is usually reserved for younger patients (aged ≤50 years) with heavy manual labour occupations because, in addition to effective pain relief and strengthened pinch grip, it provides improved stability while maintaining the length of the first ray. Painful non-union can be an issue when undertaking this procedure. The rate of non-union has been reported between 0% and 48%, with a mean of 13%.21 Literature comparing arthrodesis procedures to trapeziectomy with or without interposition arthroplasty shows similar results with tip pinch, key pinch and grip strength; however, pain relief, cold intolerance and complication rates are better in the trapeziectomy group.4
Implant-associated procedures
A variety of implantable devices have been described with varying results in the literature.3,4,8,22 They can be divided into five groups on the basis of the classification described by Vitale. These include: 1) total joint replacement, 2) hemiarthroplasty, 3) interposition of implant with partial trapezial resection, 4) interposition of implant with complete trapezial resection and 5) interposition of implant with no trapezial resection. Interposition materials include biologics, silicone, pyrolytic carbon, titanium and cobalt chrome. Systematic reviews have found a consistently higher failure rate for all implant arthroplasty groups when compared with non-implant arthroplasty.8 These failure rates approach 40% in some studies. However, the data are derived from level III and IV studies of small case series; therefore, caution needs to be exercised in extrapolating from these data. The overall rate of implantable device failure is likely to be underestimated because of the small sample sizes and the short- to medium-term follow-up period in these study groups.8
Conclusion
The thumb CMCJ is one of the joints most frequently affected by osteoarthritis. Dysfunction of the joint can lead to significant impairment of hand function. Both non-operative and operative strategies are effective in managing pain and dysfunction associated with this joint, and treatment should be individually tailored to the patient’s needs. Eaton’s staging of the disease provides a framework on which treatment rationales can be based. The evolution of implant arthroplasties provides novel solutions that negate the need for graft harvesting; however, failure rates appear to be higher than with non-implant arthroplasties. Though most surgical options have similar outcomes with regard to pain and grip strength, owing to the reduced complication profile, simple trapeziectomy or T-LRTI remain the standard by which other procedures are measured.