The radius and ulna are the long bones fractured most commonly in school-aged children, accounting for 40% of fractures.1,2 Forearm fractures occur at a rate of 1.5 per child, with the ratio of affected boys to girls increasing to 5.5:1 at adolescence. For children over the age of eight years, the distal radius is the site of 25% of all fractures.2
Fracture management is guided by the fracture pattern and remodelling potential. The aim of this article is to provide an overview of management concepts and support general practitioners to confidently manage these fractures and refer to orthopaedic services when required.
Initial assessment
The mechanism of injury may suggest the likelihood of fracture as well as type of fracture sustained. It is important to remember that wrist sprains are uncommon in children.3 Additional injuries should be sought, such as a distal humerus fracture in association with a fracture at the wrist. Past history may provide insight into pathological fractures. The possibility of non-accidental injury should be considered.
Documentation of neurovascular status is essential before and after any intervention, including cast or splint application. A simple screening aid for neurovascular injury in children is to play ‘rock, paper, scissors, okay?’4 ‘Rock’ tests the median nerve supply to the finger flexors, ‘paper’ tests the radial nerve supply to wrist and finger extensors, ‘scissors’ adducts the thumb, abducts the index and middle fingers, and flexes the ring and small fingers to test the ulnar nerve supply to the intrinsic hand muscles, and the ‘okay’ position isolates the anterior interosseous branch of the median nerve with flexion of the thumb and index finger to form a circle. Sensation is examined on the first webspace dorsally (radial nerve), and the pads of the index finger (median nerve) and small finger (ulnar nerve). Demonstrating with the uninjured hand first can build trust.
The pain felt by most patients presenting to general practice with a fracture can be relieved with oral paracetamol and nonsteroidal anti-inflammatory drugs, with a small sip of water if fasting for potential surgery. Nitrous oxide or intranasal or oral opioids may facilitate splinting and transport in more severe cases.
Fracture types
Torus (buckle) fractures
The anatomical term ‘torus’ refers to a rounded protuberance.5 Also called a ‘buckle’ fracture, torus fractures are characterised by buckling of one or more cortices of the bone as a result of a compressive force, typically a fall from standing height onto the outstretched hand. These fractures usually occur in children <10 years, and the distal radius and/or ulna metaphysis is the most common site. The majority of the cortex remains intact, and torus fractures are therefore inherently stable. They can be managed appropriately with a range of immobilisation methods from casts to removable splints,6,7 balancing adequate immobilisation for pain relief against compliance, convenience and costs related to follow-up. A removable splint provides adequate protection while being easily removed by parents at home after a 3–4-week treatment period without further clinical or radiographic follow-up.6,7 Sports, high impact and loading should be avoided for a further four weeks.
Greenstick fractures and plastic deformity
Greenstick fractures are incomplete fractures involving disruption of 1–3 sides of the bone with bending of the others, akin to bending and splintering a tongue depressor without snapping it clean in two. Both the radius and ulna are commonly affected, and these fractures commonly occur with falls from a height or during recreational activities as a result of combined bending and twisting forces.8 A fracture of both bones at the same level of the forearm suggests a bending force was applied, while fractures at different levels suggest that a rotational force has spiralled through both bones and the intervening interosseous membrane.9 Greenstick fractures can affect any region of the forearm, and clinical deformity is common.9,10
Acceptable fracture angulation is that which does not require manipulation and is dependent on the capacity to remodel and restore normal alignment. The most important determinant is the time until skeletal maturity, which, as a general rule of thumb, occurs at 14 years of age for girls and 16 years of age for boys.11 Many guidelines stratify angulation for those aged <8–10 years, and those aged ≥10 years. Fifteen-degree angulation and 45° malrotation are considered acceptable in children aged <10 years, while 10° angulation and 30° malrotation should be applied for those aged ≥10 years (Table 1).12–14
| Table 1. Acceptable displacement guidelines |
| Fracture type |
Age <10 years |
Age ≥10 years |
Notes |
| Buckle fractures |
<25° angulation |
<15° angulation |
|
| Distal third greenstick or complete fractures |
<15° angulation
<1 cm shortening |
<15° angulation
<1 cm shortening |
Beware of distal radioulnar joint dislocation |
| Middle and proximal third greenstick or complete fractures |
<15° angulation
<1 cm shortening |
<10° angulation
<1 cm shortening |
Beware of radial head dislocations with ulnar fractures and plastic deformity |
| Physeal fractures |
<50% displacement
<30° angulation |
<25% displacement
<25° angulation |
Avoid delayed referrals |
Malrotation can be difficult to assess. As a guide, the radial styloid should face opposite the bicipital tuberosity of the radius, and the ulnar styloid should face opposite the coronoid process of the ulna.15 The majority of forearm growth occurs at the wrist; therefore, a greater degree of angulation can be accepted for distal forearm fractures when compared with more proximal fractures as the remodelling potential is higher.16 Radial and ulnar deviation have less potential to remodel, and rotational deformities have no potential to remodel.14 Clinical deformity often provides a clue that orthopaedic intervention is required.
Greenstick fractures are inherently unstable and will continue to angulate if not adequately splinted (Figure 1). With an appropriately moulded cast or ‘front and backslab’ application, the intact cortex will maintain a degree of stability. Aftercare includes one X-ray immediately after cast application if fracture manipulation was required, and one follow-up X-ray after 7–10 days to document maintenance of position. If reduction is maintained, one further clinic visit at 5–6 weeks post-fracture for removal of the cast is all that remains.17 X-rays to check union are not required in the majority of cases.17
Distal third radius and ulna fractures in older children are suitably managed with immobilisation that does not extend above the elbow. In young children, extending the splint or cast above the elbow may assist to prevent slippage of the immobilisation device on the chubby forearm (Figure 1B). Acute fractures can be managed safely in volar and dorsal (sandwich-style) slabs that extend up to the metacarpophalangeal joints but leave them free to move. Midshaft and proximal third fractures require immobilisation of the elbow joint.
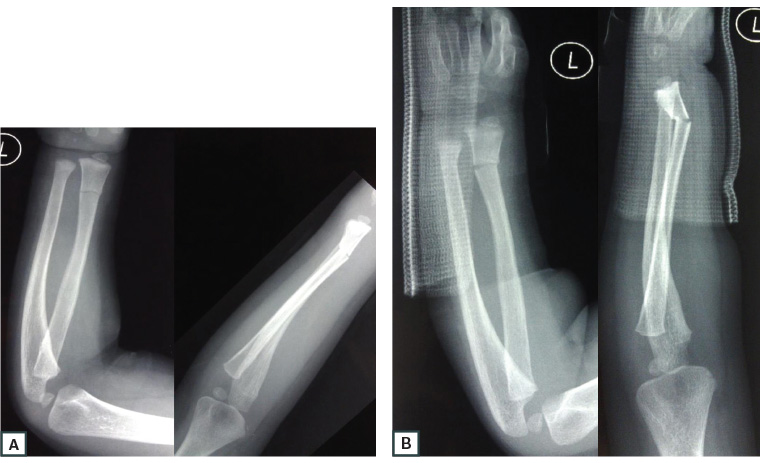
Figure 1. Anteroposterior and lateral X-rays of the forearm and wrist showing a greenstick fracture of the distal radius in a child aged three years
A. X-rays at initial presentation; B. The short, volar splint has slipped at follow-up and provided inadequate immobilisation. The fracture has displaced. Extending immobilisation above the elbow in young children and applying volar and dorsal slabs provides better fracture stability.
Plastic deformity refers to increased bowing to the radius or ulna without an obvious fracture line due to multiple microfractures along the length of the deformity.9 Management is similar to greenstick fractures, and reduction is indicated on the basis of the degree of deformity. Follow-up can be simplified as for greenstick fractures.17 Plastic deformity and isolated greenstick fractures of the ulna can be associated with radial head dislocation (Monteggia injury), and it is critical that this is not missed.
Complete fractures
A complete fracture disrupts the entire cortex, with resultant deformity and angulation. These are often found in higher-energy injuries, such as falls from a height, sports and road traffic accidents.18 Complete fractures may occur in any location and commonly affect both the radius and ulna. The lack of any cortical continuity allows for complete displacement as well as shortening, which may appear as ‘bayonet’ deformity on the lateral X-ray. Despite complete fracture of the bones, the thick periosteal sleeve often remains intact, providing some stability. Parents and clinicians alike are often surprised to learn that 100% displacement and bayonet apposition of the distal radius and ulna will completely remodel as long as the angulation remains within acceptable limits, and at least two years of growth remain.14,19 Acute orthopaedic advice or emergency department review is warranted for displaced greenstick or complete fractures.
Growth plate injuries
Salter-Harris fractures involve the growth plate. The classification system, first proposed in 1963, grades fractures from I to V.20 It is remembered with the ‘SALTR’ acronym: Straight across the physis, Above the physis extending into the metaphysis, Low to the physis extending into the epiphysis and articular surface, Through the physis going above and below, and cRushed. Growth plate fractures account for 30% of all long bone fractures.21 Their incidence peaks during the pre-adolescent growth spurt and, given the relative difference in skeletal maturity, girls present on average 1.5 years earlier than boys for similar fracture locations.21
The risk of growth plate damage with fracture increases with increasing Salter-Harris grade.10 The distal radius physis contributes 75% of forearm length, and damage to this growth plate can cause significant disability. Delayed manipulation of fractures or remanipulation of fractures that have lost position beyond seven days is ill-advised because of the risk of further disrupting the physeal blood supply and high rates of growth arrest.9,16 Acute referral and close review is warranted, particularly for high-energy injuries.
Fracture-dislocation
In cases of isolated radius or ulna fracture, particularly with significant angulation or displacement, it is important to check the elbow and wrist joints to rule out an associated dislocation.
Galeazzi fracture-dislocations involve a fracture of the distal third of the radius and dislocation of the distal radioulnar joint at the wrist.22 These account for 3% of paediatric distal radius fractures.23
Monteggia fracture-dislocations, first described in 1844, involve a fracture of the ulna associated with dislocation of the proximal radius (radial head).24 They typically occur in children aged between four and 10 years22,24 as a result of a fall onto an outstretched hand. The elbow is forced into hyperextension, the forward momentum dislocates the radial head, and the ulna, burdened with the full force of the fall, fails in tension.
Fracture-dislocations should be splinted to include the elbow and wrist to prevent forearm rotation. Urgent referral is warranted as rapid healing in children will make delayed reduction of the dislocation difficult.
Principles of management, referral and follow-up
Individual management is influenced by local resources, and knowledge of local referral pathways is helpful. GP management of a child with no appreciable clinical deformity may include pre-emptive immobilisation and outpatient radiology, followed by telephone advice or orthopaedic surgeon/fracture clinic referral as required, avoiding unnecessary trips to the emergency department. Communication with radiology departments can help direct patients appropriately following X-ray confirmation of a fracture. Advising the referral hospital whether your practice has cast-removal facilities can help with planning follow-up, particularly for patients in rural and remote areas.
Injuries with clinical deformity, neurovascular compromise or a concerning radiology report should be referred to the local acute orthopaedic service or emergency department. A telephone call prior to patient transfer can expedite management. Growth plate injuries require early review. Online resources provide general guidance as to when referral is required.6,16,25
As a general rule, forearm fractures and suspected fractures in children require early follow-up and formal follow-up after healing until normal range of motion is restored. This will minimise cases of missed injuries and unanticipated outcomes. It is important to remember that wrist sprains are uncommon in children.3 Appropriate follow-up depends on the fracture type and local circumstances and may include a fracture clinic, virtual fracture clinic, private orthopaedic clinic, general practice or a combination. True torus (buckle) fractures are stable injuries. Some hospitals may choose to apply a removable immobilisation device, provide written information to parents and forego formal follow-up for these fractures.6 This is appropriate, as long as the diagnosis is correct and the injury is not in fact an unstable greenstick fracture (Figure 1A).
Summary
The wide spectrum of forearm fractures and differences in age can create a daunting management matrix. Confident management of simple fractures by the GP, as well as appropriate referral, allows for an efficient healthcare system and optimal outcomes.
Key points
- True torus (buckle) fractures of the distal radius and ulna are inherently stable and may be managed with 3–4 weeks of immobilisation in a splint, or a soft cast that can be removed by parents. More complex fracture patterns should be discussed with an acute orthopaedic service via the local emergency department or referral to hospital.
- Greenstick fractures and plastic deformity are common in the midshaft of the forearm. The degree of angulation dictates whether reduction is necessary. Fracture reduction may be required for fracture angulation >15° in children aged <10 years and >10° in children aged ≥10 years. Discussion with an acute orthopaedic service or referral to the emergency department is recommended for these fracture types.
- Complete fractures, fractures involving the growth plate and any fracture with clinical deformity should be referred to an orthopaedic service or emergency department acutely.
- It is important to be wary of isolated complete radius or ulna shaft fractures/plastic deformation and always look for a concomitant dislocation of the proximal radio-capitellar or distal radioulnar joints.
- Follow-up until the child’s usual range of motion has returned is a safe approach to minimise missed injuries and unanticipated outcomes.