Background
General practice is now completely computerised yet still largely reflects the habits and culture of the paper records that these computer programs have replaced. Technology is advancing rapidly, and computers are poised to start interacting (or intruding) in the consultation in new ways that practitioners (GPs) will once again need to understand and integrate.
Objective
The aim of this article is to describe the developing trends in computing, data and intelligence, and demonstrate to GPs how to best use the examination room computer to enhance care of patients, prepare for upcoming revolutionary changes and continue to connect with patients.
Discussion
Using two real-world examples, this article explains the complexity of the changing environment and implications for the patient–doctor relationship, and offers guidance for change.
Technology is increasingly encroaching into the doctor–patient consultation space, moving beyond the relatively straightforward applications in medical records. Consider the following two ‘real-world’ scenarios using technologies that are current, tested and available or will be deployed soon.
In the first scenario, the consultation is with an established patient who has diabetes, chronic obstructive pulmonary disease and depression. The consultation appears routine, and the diagnosis is cellulitis. But when the antibiotics are prescribed, the clinical software warns that the patient is at high risk (≥80% chance) of needing to attend the emergency department in the next 30 days.1
In the second scenario, a patient comes in to see their general practitioner (GP) and confidently states, ‘I have pneumonia and would like some antibiotics!’ When their GP asks how they can be so confident, they say, ‘I have been sick for days with a fever and a cough, and when I coughed “into” my smartphone app it told me I have pneumonia’.2
What is your initial reaction to these two scenarios? These real-life clinical situations represent validated, accurate applications of computing and artificial intelligence technologies. Yet both ‘disrupt’ the traditional views of the doctor–patient relationship. Practitioners’ reactions to, and subsequent treatment of, patients in these and other future technology scenarios must be faced and prepared for.
Since the turn of the century, general practice in Australia has been effectively completely computerised.3 Australia joins jurisdictions such as the UK, New Zealand and parts of Europe in that regard, although countries such as the USA still lag behind. Electronic health record (EHR) use in the USA in particular has been driven by administrative and central needs rather than clinical needs, and the doctor–patient relationship has been disrupted.4 Therefore, Australia’s current EHR position permits a prime test bed for the future of computerisation. The technology change process to date has been complex, yet Australian GPs have shown themselves to be flexible in adapting to this new technology. The integration of artificial intelligence, new data sources and patient access to data are examples of a new wave of technological change that is coming and will challenge general practice yet again.5 The traditional relationship must expand to become a true triadic one, with the computer an equal partner.6 Figure 1 reconstructs the traditional relationship (patient agenda + doctor agenda = outcome) into a three-way relationship. The ‘human’ aspect is understood – they are complex beings who have social, cultural and many other influences. The computer is also complex; an expression of programming, information sources, even culture. The examples above represent an amalgam of information, artificial intelligence and medical and programming input. Just as humans can have unconscious biases, so too can the computer.
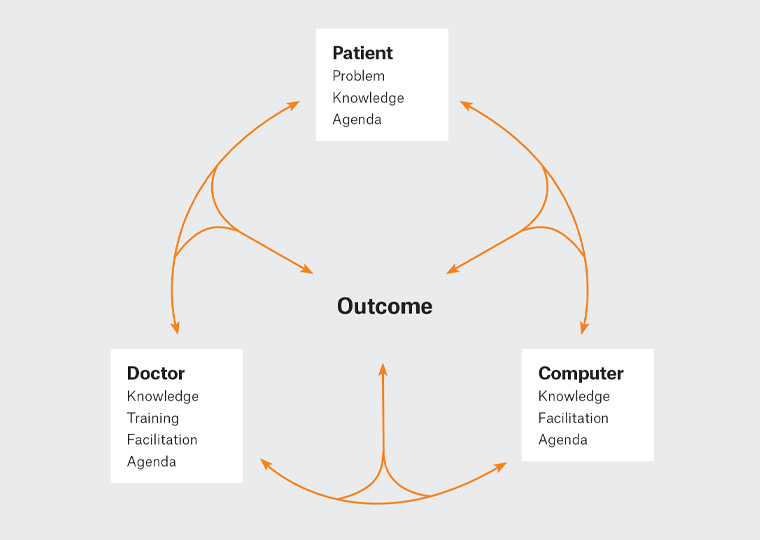
Figure 1. The triadic consultation6
Reproduced with permission from Oxford University Press: Pearce C, Arnold M, Phillips C, Trumble S, Dwan K, The patient and the computer in the primary care consultation, J Am Med Inform Assoc 2011;18(2):138–42, doi: 10.1136/jamia.2010.006486.
There are, however, two significant changes that need to be dealt with, one of which is incremental and one of which is new. The incremental change is the democratisation of data and information, which brings the patient increasingly into the focus of healthcare. In the 1960s, visionaries such as Balint7 and Szasz and Hollander8 challenged the traditional views of the consultation, and between them introduced the concept of patient-centred medicine.9 Nevertheless, the profession managed to maintain the power in this relationship by controlling the flow of information.10 Patients were still exposed to only the limited information revealed to them. In the new world, patients have access to the basic information (through initiatives such as My Health Record)11 in addition to the same levels of evidence that doctors have available (eg Google Scholar) and increasingly the same tools that doctors can use (eg the app in the second scenario).
The second, more fundamental, change relates to the medical role in managing patient care. What once was characterised as ‘diagnose, treat and prognose’12 will likely be turned on its head. In the past, experience and tradition were used to manage patients. Then the scientific method introduced the concept of ‘validated’ treatments. It was then that the GPs became patients’ medical information managers.13 In the new era, these two approaches will need to be blended. Computers are more reliable information managers, and much of that role will be taken. The new consultation will need to develop an approach that takes into account patient experience, provider satisfaction, better outcomes and value for money.
Fortunately, patients with medical concerns will always want a human to help them heal. Beyond conversation, there is diagnostic and therapeutic benefit in the physical examination/touch.14 Therefore, GPs must become masters of understanding the patient perspective and the ‘whole patient’ – effectively becoming a mentor. Importantly, the concept of how to care for the ‘whole patient’ must change. In the past, this referred to understanding the patient beyond the context of just the disease, in more human terms. Now, the definition of the ‘whole patient’ must extend to include the wider view of the patient’s available data, both the data in their chart or collected from the patient’s research. Doctors will also soon see patient-entered data transmitted from wearables and home monitors as well. It is now not just the patient ‘embodied’ (ie the physical person), nor the patient ‘inscribed’. The data that exists in the medical record but must also be patient ‘created’; a fusion of both human experience and data.
As a greater number of forms of patient data merge to create the ‘whole patient’, GPs are likely to need to find more time to review and evaluate the data, learn to synthesise the data and validate the reliability and trustworthiness of this data. The scope of these developing issues will need to continue to be addressed and acknowledged. This works in both directions, as patients (via My Health Record) will have more access to their own data, often without context. They will in turn be attempting to interpret their data, often without guidance.
It is possible use existing knowledge to make recommendations about how to use the computer in the new consultation. The computer is more than just a tool for the doctor; it is a third party to the consultation and can be valuable to both patient and doctor.6 The simplest guide for the use of the computer is to ‘RESPECT’ that balance in the consulting room:15
- Review the EHR prior to the patient entering the room – briefly review recent visits and any new information.
- Entrance – greet the patient and make sure you engage them before turning to the EHR.
- Say everything that you are doing – talk about what you are doing in the EHR, and what the EHR is doing.
- Position the computer so the patient is able to see the screen when necessary by putting the computer in the patient–provider–EHR triad.
- Engagement position – be in an engaging position during critical conversations with the patient. Face the patient and not the computer.
- Computer confidence – value the computer; speak positively about the EHR.
- Teach the patient through use of the EHR.
At this point it is beneficial to revisit the two scenarios presented at the start of this article. In the first (the risk of emergency department prediction), the computer is simply alerting the doctor–patient dyad of the patient’s risk for future escalated care. In this regard, it is simply a risk assessment tool that can be used along with the patient’s information and the GP’s knowledge of the patient, family, supports, etc to decide the best course of follow-up care. A GP’s course of action in Sydney may be different to what they would do if they were consulting in Hermannsburg.
With the second patient (who found their own ‘pneumonia diagnosis’), the traditional skills of diagnosis appear to have been usurped by the patient’s research. However, the GP still has a role in the examination, management and prognosis of the patient. The patient may actually end up having an upper respiratory tract infection, or they may have pneumonia. Here the GP would use diagnostic skills that the patient cannot currently obtain via a web search.
GPs give complex multisystem care for an incredibly diverse group of patients. They continue to have patients who expect them to be omniscient and to be their guides. Yet increasingly there will be patients who have access to greater amounts of information and thus have more input into their own care. The profession must learn to adapt these new technologies to meet the needs of patients in the new era. In the past decade, Australian general practice computerised with relatively little fuss and relatively few incentives. GPs managed to decipher what to do and how to do it. The professional is now at the beginning of the greatest change to how healthcare is delivered since the advent of evidence-based medicine, if not the scientific method itself. It is an opportunity to be ahead of the game, rather than follow.