The human acetabulum is shallower at birth than at any other time during development. The embryonic acetabulum begins as a deeply set cavity that almost entirely encloses the femoral head but gradually becomes shallower as birth approaches. This trend reverses after birth, with the acetabulum deepening, femoral head coverage increasing and hip morphology improving.1
Teleologically, it is possible that a temporarily increased hip range of motion in the third trimester is required to accommodate the lower limb within the limited intrauterine space. Postnatally, the sphericity of the femoral head and deepening of the acetabulum are expected to increase progressively through childhood.1,2
The wide spectrum of pathology affecting this process is named developmental dysplasia of the hip (DDH). Presentations can vary from an infant born with a fixed, irreducible dislocated hip through to mild acetabular dysplasia only diagnosed in adulthood.3 Management of this wide continuum of pathology requires careful consideration, because management varies greatly as the age of the child increases.4
DDH and its sequelae continue to have a major impact on healthcare, with the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) reporting that nearly 7% of total hip replacements in Australia are directly attributable to DDH.5
The emphasis of this article is on the management of DDH in infancy and the early years; management of DDH during adolescence and adulthood is not included.
Establishing the diagnosis
As previously stated by Williams, ‘repeated, carefully performed clinical examinations of the paediatric hip from newborn to walking age remain the best method for early detection of DDH’.6 This, combined with an understanding of the risk factors, will help in the early diagnosis and management of children with DDH (Table 1).
| Table 1. Developmental dysplasia of the hip: Referral guidelines |
| Initial work-up |
Suggested general
practitioner management |
When to refer to paediatric orthopaedics |
Clinical history
Risk factors:
- Female sex
- Breech delivery
- Intrauterine packaging deformities (eg plagiocephaly, foot deformities or torticollis)
- Family history of DDH
Physical examination
- Hip examination to check for instability with Barlow’s and Ortolani’s tests
- Limited abduction
- Deep uneven gluteal crease
- Leg length discrepancy
- Waddling gait after walking age
Investigations
- Hip ultrasonography if aged ≤6 months (paediatric ultrasonography service if possible)
- Plain X-ray if aged >6 months
|
Screening
- Screening ultrasonography if risk factors present in child aged <6 months
- Screening ultrasonography at six weeks of age for all breech presentation babies
- Plain film X-ray (anteroposterior pelvis with leg in extended position and ‘frog leg’ views) if risk factors present for a child aged
>6 months
Surveillance
- Surveillance anteroposterior pelvis X-ray at 12 months of age if child previously investigated for DDH (because of incidence of late‑presenting DDH)
|
Urgent
- Abnormal clinical examination
- Positive Barlow’s or Ortolani’s test
- Limited hip abduction
- Leg length discrepancy
- Abnormal ultrasound or X-ray
- To properly triage the referral, access to the radiological images is required to ensure that the radiological interpretation is correct
|
DDH, developmental dysplasia of the hip
Adapted from Department of Orthopaedics, Referral guidelines: Developmental dysplasia of the hip – DDH, Melbourne, Vic: Royal Children’s Hospital, 2020, Available at www.rch.org.au/ortho/for_health_professionals/Developmental_dysplasia_of_the_hip_%E2%80%93_DDH/ [Accessed 4 February 2021]. |
The priority is differentiating between neonatal hip instability, acetabular dysplasia and subluxation or dislocation of the hip, as severity of involvement (Figure 1) determines the treatment required to obtain a concentric reduction.
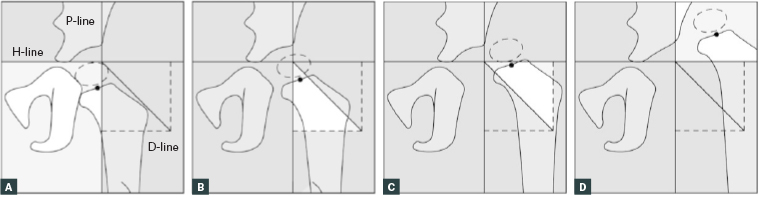
Figure 1. International Hip Dysplasia Institute classification for severity of developmental dysplasia of the hip (not requiring the presence of an ossific nuclei).18 H-line is Hilgenreiner’s line, drawn through the top of the triradiate cartilages bilaterally. P-line is Perkin’s line, drawn perpendicular to the H-line at the superolateral margin of the acetabulum. D-line is the diagonal line drawn 45° from the junction of H-line and P-line. H-point is the midpoint of the superior margin of the ossified metaphysis.
A. Grade I: the H-point is at or medial to the P-line; B. Grade II: the H-point is lateral to the P-line and at or medial to the D-line; C. Grade Ill: the H-point is lateral to the D-line and at or inferior to the H-line; D. Grade IV: the H-point is superior to the H-line.
Reproduced with permission from Narayanan U, Mulpuri K, Sankar WN, Clarke NM, Hosalker H, Price CT, Reliability of a new radiographic classification for developmental dysplasia of the hip, J Pediatr Orthop 2015;35(5):478–84, doi: 10.1097/BPO.0000000000000318.
Neonatal hip instability is laxity limited to the hip joint capsule and is influenced by hormonal and genetic factors.7–10 This laxity has a natural tendency to correct itself, with 95.3% of hips returning to normal morphology by 12 weeks of age.11
The spectrum continues to more severe forms of dysplasia with worsening hip instability, to the established hip subluxation with significant hip dysplasia, some of which may then progress to frank hip dislocation.3,4,11,12
Imaging for DDH
Ultrasonography
In the presence of risk factors or with an equivocal clinical examination, ultrasonography is the reference standard in children aged <6 months (before the proximal femoral ossific nucleus is visible).13
The Graf method subscribes to a table of α and β angles to provide a quantitative classification system,2 while the dynamic (Harcke) technique for position and stability has qualitative definitions.14 New ultrasonography techniques using three-dimensional probes and machine learning have built on existing two-dimensional ultrasonography techniques to produce three-dimensional renderings of the infant hip joint15,16 to improve interobserver reliability.
Radiography
After the age of five months, the femoral epiphyseal ossification centre begins to obscure sonographic landmarks.13,17 The pelvic radiograph is the benchmark for surveillance of acetabular development, especially with the introduction of the International Hip Dysplasia Institute (IHDI) classification method, which demonstrates excellent interexaminer reliability even when ossific nuclei are absent or delayed.18
Magnetic resonance imaging
Magnetic resonance imaging (MRI) has the benefit of being non-invasive and offers a level of anatomic detail that allows for differentiation of ossified and unossified structures. It is an excellent modality in the intra-operative period, usually after reduction and spica casting, to assess the concentricity of reduction.17
Hip MRI protocols enable efficient and accurate evaluation of the hip cartilaginous anlage, the ligamentous and soft-tissue abnormalities that may obstruct successful reduction,17 without exposure to ionising radiation. Table 2 lists anatomic structures and the respective MRI findings in DDH.
| Table 2. Magnetic resonance imaging findings of the anatomic structures involved in developmental dysplasia of the hip |
| Anatomic structures |
Imaging findings |
| Acetabular morphology |
Shallow, dysmorphic acetabulum with abnormal cartilage anlage |
| Femoral morphology |
Delayed ossification of non-spherical femoral head |
| Labrum |
Labral hypertrophy (limbus) with mucoid degeneration |
| Pulvinar |
Pulvinar hypertrophy with fibrofatty proliferation |
| Ligamentum teres |
Hypertrophy with contraction of the transverse acetabular ligament |
| Hip capsule |
Patulous and redundant joint capsule |
Goals of treatment
Obtaining a concentric reduction
A concentric reduction refers to a situation in which the femoral head is well docked in the acetabulum. It is required for the long-term goal of a congruent, spherical hip at skeletal maturity.12,19 Reduction of the hip is relatively straightforward in neonatal hip instability, but if the hip subluxates and remains incongruent while braced, soft tissue obstacles to reduction may develop, obstructing concentric reduction of the femoral head into the acetabulum (Figure 2).3,4,17
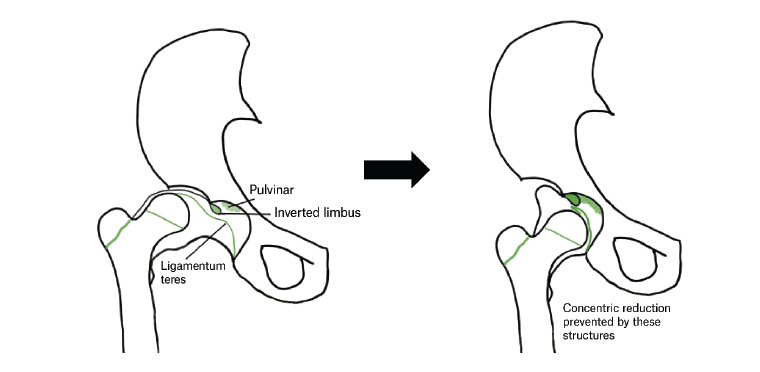
Figure 2. Intra-articular obstacles to concentric reduction of the hip in patients with developmental dysplasia of the hip
Maintaining reduction and stability of the hip
Once reduction of the hip has occurred, it is imperative to maintain the reduction until the hip is stable and is developmentally normalising.20 There are several contributing factors that affect persistent hip instability, primarily bony deformities in the coronal and transverse planes. Many hips affected by DDH have excessive femoral anteversion, abnormal acetabular version, coxa valga and residual acetabular dysplasia (Figure 3).19,21
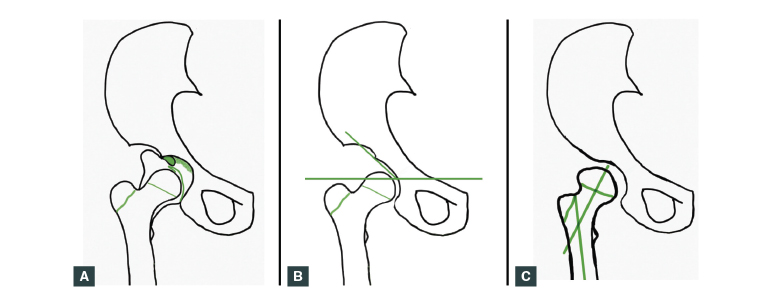
Figure 3. Potential causes of residual instability in developmental dysplasia of the hip
A. Patulous and redundant capsule; B. Acetabular dysplasia; C. Proximal femoral anteversion and coxa valga
Stimulating development of normal hip morphology
Timely DDH treatment uses the hip’s ossification potential to obtain a reduced, stable and developmentally appropriate hip while aiming to avoid the complications of growth disturbance and osteonecrosis.22,23 Early reduction facilitates normal acetabular development and reduces the need for later pelvic surgery. A concentric reduction normalises the joint forces, which stimulates remodelling and reorientation of the growing hip.4,9,12,24,25
Avoiding complications
Interruptions to proximal femoral growth, and osteonecrosis of the femoral capital epiphysis presumably occur as a result of vascular damage to the proximal femur during hip reduction and stabilisation.20,25,26 Care must be taken at each step of treatment to minimise the risk of iatrogenic injury.
Treatment options
Hip abduction bracing
In a child aged <4 months, an ‘abduction brace’, commonly the Pavlik harness or Denis Browne hip abduction brace, is used for an unstable hip.23–25 The semi-rigid immobilisation of the Denis Browne brace is preferred to the Pavlik harness in the older child who is beginning to roll.
In children with dislocated hips, bracing may be applied but must be closely monitored and re-examined within two weeks to confirm concentric reduction both clinically and radiologically. If reduction is not achieved within this timeframe, bracing must be reconsidered and an alternative treatment method chosen.4,23,24
Complications of bracing include: failure to obtain and maintain reduction, leading to potential worsening of DDH with posterior acetabular insufficiency and deformation of femoral head cartilage anlage; femoral nerve palsy; inferior dislocation; and osteonecrosis.24,25,27 It is important to engage the parents of the child with pretreatment education, ongoing counselling and support during the course of treatment, as hip abduction bracing requires familial compliance to succeed.
Closed reduction, arthrography and spica cast application
If hip abduction bracing fails, or if the child presents at an older age, then a gentle closed reduction under general anaesthesia with spica cast immobilisation is the next option. An arthrography should be performed concurrently to ensure that the reduction has truly occurred and that there are no intra-articular obstacles that may prevent reduction.28 In some patients, an adductor contracture may prevent reduction, and this may be addressed with a proximal tenotomy of the adductor longus.
After closed or open reduction of the femoral head, the hip is held in flexion, abduction and internal rotation.18 The degree of abduction must be maintained in the ‘safe zone’, as insufficient abduction predisposes to re-dislocation, and excessive abduction potentially increases the risk of osteonecrosis.4,12,20,26 The stability of hip post-reduction is assessed clinically and radiologically. If the safe zone is achievable within an arc of 20–60° of abduction, a spica cast is applied prior to an MRI confirmation of concentric reduction.
Open reduction
The indications for an open reduction are failed closed reduction, a non-concentric reduction and excessive hip abduction in the spica cast. Open reductions can be performed medially or anteriorly and must manage all factors obstructing a stable concentric reduction. The patient is then immobilised in a hip spica cast prior to a transition into a hip abduction brace at the six-week mark.20,29,30
Although uncommon, re-dislocation following an open reduction is a serious complication and can markedly increase the rate of osteonecrosis. Recent modifications in technique have included transferring the ligamentum teres as a tenodesis20,30 and the development of arthroscopy-assisted techniques.31
Femoral osteotomy
The abnormal proximal femoral anatomy in DDH may predicate the need for a femoral osteotomy to achieve reduction, reduce tension and correct the joint forces around the hip.32–34 Fixation is achieved with a blade plate and can be performed to varise, de-rotate or shorten the proximal femur.
Acetabular osteotomy
Insufficient coverage of the femoral head or acetabular dysplasia may require pelvic osteotomy, especially in the late-presenting child, because of the unpredictable remodelling potential of the acetabulum. Techniques have been developed to address the problems encountered in acetabular dysplasia: an abnormally oriented acetabulum with adequate capacity or an overly capacious acetabulum resulting in a dislocatable hip.35–38
Conclusion
Recent advances in surveillance, diagnosis and management of the DDH spectrum (Table 3) have improved outcomes for many patients, but much remains to be discovered.25,39 In 2010, the IHDI initiated an international, multicentre prospective study at nine centres across Australia, North America and Europe in response to these evidence gaps in the management of infant and toddler DDH.
| Table 3. Recent advances in the care of patients with developmental dysplasia of the hip |
| Pathoanatomy |
- Evolving understanding of the affected anatomy in DDH
- Emerging knowledge about the genetic basis of DDH
|
| Surveillance |
- Improving sonographic techniques and better interpretation of ultrasonography
- Increasing use of MRI for confirmation of reduction
- Development of International Hip Dysplasia Registry
|
| Management |
- Increased availability of bracing care
- Ligamentum tenodesis to minimise re-dislocation rate
- Development of arthroscopy-assisted techniques
- Gore-Tex and water-resistant spica cast liners
|
| Prevention |
- Increased awareness of safe swaddling techniques
- Evolution of baby carrier slings to improve infant hip abduction
|
| DDH, developmental dysplasia of the hip; MRI, magnetic resonance imaging |
In the meantime, the universal tenet in DDH care remains that prompt diagnosis and management are the most important factors related to outcome; it is important to be cognisant about developmental hip pathology in asymptomatic patients through infancy and childhood.40