Case
An independent, underweight (body mass index [BMI] =14.5 kg/m2) woman aged 83 years presented to the general practice with a one-day history of worsening left lower quadrant pain, difficulty mobilising and vomiting without abdominal distension. She had no history of falls or trauma but had increasing pain on walking that now required a walking stick. She had a past medical history of asthma. There was no surgical history. She lived with her family and previously mobilised independently. Clinically, her observations were all within normal limits. However, she had left groin tenderness exacerbated with extension of the hip, scant bowel sounds and hypoaesthesia of the anteromedial aspect of her thigh. There was no palpable inguinal lump, pelvic bone tenderness, pain on rotation of the hip or bruising noted in the abdomen or lower limb.
Question 1
What differential diagnosis should be considered?
Answer 1
The differential diagnosis can be broadly considered as pelvic and lower limb pathology. One should initially exclude any underlying trauma that may suggest pathological lower limb fractures or a metabolic origin with minimal trauma. Serious considerations should exclude hip pathology (neck of femur fractures), irreducible groin hernia (inguinal direct or indirect, femoral) or aneurysms. Other differentials to consider include lymphadenopathy, urinary tract infection, gastroenteritis, appendicitis, diverticulitis, inflammatory bowel disease, bowel obstruction (even in a virgin abdomen due to congenital bands or Meckel’s diverticulum), lumbar disc pathology and testicular disorders (in males).
Case continued
The patient was sent to the emergency department for further investigations given her increasing pain. Biochemical markers revealed normal full blood examination and electrolytes. A venous blood gas analysis showed a slightly elevated lactate level of 1.33 mmol/L (reference range 0.3–1.3 mmol/L). A pelvic X-ray did not demonstrate any fractures, and a chest X-ray was unremarkable. A supine and erect abdominal X-ray showed dilated small bowel loops with air fluid levels. Urgent surgical review was coordinated, and an oral and intravenous contrast-enhanced computed tomography (CT) scan rapidly followed (Figure 1). The CT confirmed a small bowel obstruction secondary to an incarcerated left obturator hernia. All the patient’s observations remained within normal limits, but pain continued to increase with time. The patient subsequently underwent laparoscopic repair of the obturator hernia with no bowel resection, and she made an uncomplicated recovery.
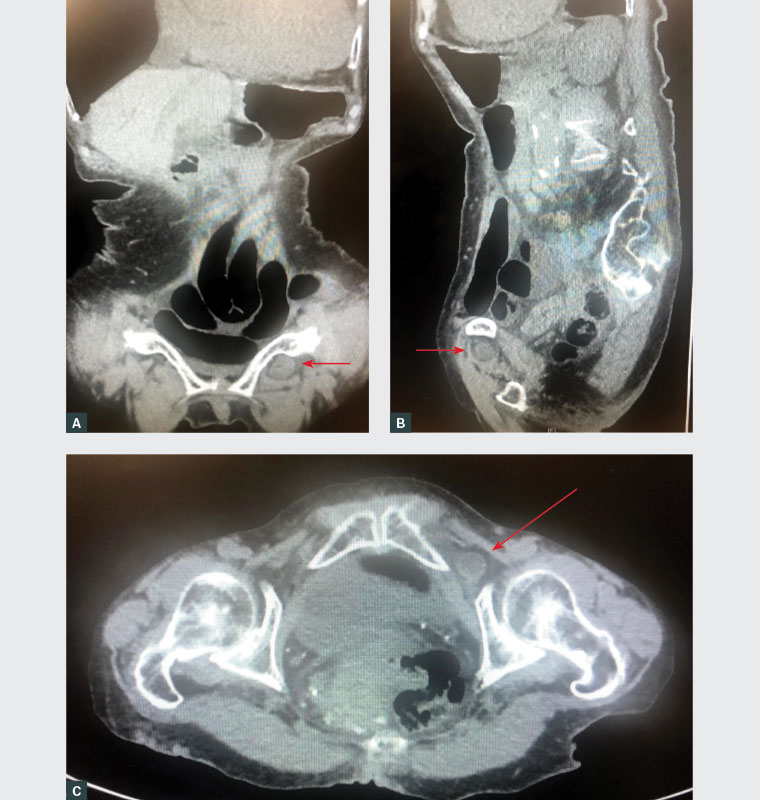
Figure 1. Computed tomography scans demonstrating small bowel obstruction secondary to a left‑sided incarcerated obturator hernia (arrows)
A. Coronal view; B. Sagittal view; C. Axial view
Question 2
What is the natural history and aetiology of an obturator hernia?
Question 3
How is this condition diagnosed?
Question 4
What is the appropriate management of this condition?
Question 5
What is the prognosis for this condition?
Answer 2
An obturator hernia is a rare clinical condition of the pelvic floor, generally unpalpable (occult), that accounts for approximately 1% of all hernias. The most common presentation in almost 90% of cases is intestinal obstruction of unknown cause in an elderly, underweight (BMI ≤18.5 kg/m2) woman with no earlier abdominal operations.1 An obturator hernia occurs when loss of the protective tissue of the obturator canal allows extraperitoneal tissue or intra-abdominal content to course from the pelvis to the proximal inner thigh. The obturator foramen lies inferior to the pelvic acetabulum, superiorly bound by the superior pubic ramus and inferiorly by ramus of ischium. It contains the obturator nerve, artery and vein surrounded by a fat cushion.2
The risk factors for primary groin hernias include family history, chronic obstructive pulmonary disease, smoking, low body mass index, chronically raised intra-abdominal pressure and collagen vascular disease.3 Adult males commonly present to general practice for groin hernias, but the obturator hernia is 6–9 times more likely to occur in underweight, multiparous women who are in their seventh decade of life and older.4 Anatomically, this may be explained by the more oblique female pelvis and greater transverse diameter in females, and laxity of the pelvic floor.5 Obturator hernia occurs in three stages, from extraperitoneal fatty tissue infiltration of the canal to hernia sac formation and protrusion of intra-abdominal content with clinically significant symptoms. The sac usually contains the small bowel but may also include the appendix, omentum, bladder or fallopian tubes. It is more common on the right side than the left as the sigmoid colon usually protects the obturator canal.6 Patients almost always present without a palpable lump; they commonly have features of intestinal obstruction, with an estimated mean onset of symptoms of approximately one week.7 As a result of its high morbidity and mortality, an obturator hernia should be considered in the differentials for elderly underweight women presenting with symptoms of bowel obstruction or pain over the thigh and hip.
Answer 3
Obturator hernias are generally small and, because of their pelvic location, almost always present without a lump, unlike inguinal hernias. The symptoms can be very nonspecific and vague, unlike the classical features of an inguinal hernia, highlighting the importance for clinicians to have a strong understanding of the natural progression of the disease. A comprehensive abdominal examination with particular attention to the groin region, assessing for a palpable mass, is important when looking for a hernia.
8 However, it is important to note that in the presence of an obturator hernia, clinical examination may not reveal this classic sign of a palpable mass in the groin, despite being associated in most cases with symptoms of intestinal obstruction. Table 1 outlines common signs specific to strangulated obturator hernia.
9 The Hannington-Kiff sign is reported as more specific than the pathognomonic Howship–Romberg sign;
10 however, clinical signs are examiner dependent.
| Table 1. Key clinical signs of obturator hernia |
| Signs |
Description factors |
| Obturator neuralgia |
Intermittent or constant hypo- or hyperaesthesia or cramp-like sensation in the inguinal crease to the anteromedial aspect of the thigh. |
| Howship–Romberg sign |
This sign is considered pathognomonic for obturator hernia presenting with pain in the medial thigh by compression of the nerve against the hernia. The pain is usually exacerbated by extension, adduction or medial rotation of the hip (present in 25–50% of cases). The pain is usually relieved by flexion of the thigh. |
| Hannington-Kiff sign |
This refers to an absent adductor reflex in the thigh from obturator nerve compression. Percussion of the adductor muscle 5 cm above the knee results in contraction. Contralateral comparison often shows hyperactivity and a normal ipsilateral patellar reflex. |
| Bruising of the femoral triangle |
A faint bruise below the medial inguinal ligament is a consequence of bowel infarction with exudation of blood into the upper thigh. |
Ultrasonography may be useful in distinguishing a groin hernia from lymphadenopathy; however, CT is considered the standard for accuracy and specificity in the diagnosis of an obturator hernia. If there is suspicion of incarceration or doubt of the diagnosis, general practitioners should seek expert advice early and refer to their local emergency department for urgent surgical review to reduce mortality from diagnostic delay.
Answer 4
Early investigation of thin, elderly women with clinical symptoms of intestinal obstruction in the abdomen without any previous surgery or thigh pain beckons immediate surgical referral to optimise diagnostic confirmation and minimise therapeutic delay to surgery. The factors associated with increased mortality have been attributed to poor physiological reserves, pre-existing medical conditions, a higher incidence of bowel strangulation, and delay in diagnosis and management due to vague signs and symptoms. The misdiagnosis of an inguinal or femoral hernia does not have the high rates of morbidity and mortality of an obturator hernia. Minimally symptomatic inguinal hernias may be carefully observed, provided there are no symptoms of obstruction, strangulation or ischaemia. The management in these cases can be referred to a surgeon and can be followed expectantly, with an estimate that 75% of patients will require surgery within 10 years.11 However, if one suspects an obturator hernia, an immediate referral to the emergency department with swift surgical review is warranted. The difference in management between an inguinal and obturator therein lies within the diagnosis and time to theatre that affects the clinical outcomes and mortality.
The obturator hernia is treated surgically using various repair techniques including laparotomy and laparoscopic approaches. The basic principle is reduction of hernia sac contents, excision of the sac and repair of the abdominal wall defects. Kogha’s study on laparoscopic repair of obturator hernias used laparoscopic transabdominal preperitoneal repair to reduce the bowel followed by tacking the prosthetic mesh, unless contraindicated by infection or cases of peritonitis. These results showed lower post-operative complications and post-operative length of stay when compared with laparotomy.12 Routine intraoperative assessment should include evaluation of obturator, femoral and inguinal areas bilaterally, looking for potential associated hernia defects. There are significant risks of intestinal perforation and bowel necrosis that necessitates resection, contributing to the high mortality rate. The senior author favours laparoscopic management in his practice, consistent with the growing international literature that has shown it to produce less post-operative pain and shorter hospital stays.12 The patient in this case study underwent laparoscopic repair with a good outcome, but she required ongoing allied health input for a safe, functional return to home.
Answer 5
Although obturator hernia is rare, it is associated with high morbidity and a mortality rate up to 70%.13 Most patients are elderly and often have associated comorbidities, additionally compounded by unfavourable surgical outcomes attributed to anastomotic problems.14
Key points
- An obturator hernia can present in a vague and nonspecific manner, contributing to its diagnostic challenge.
- Suspicion for an obturator hernia should arise on assessment of thin, elderly women with bowel obstruction, particularly where intermittent symptoms or medial thigh pain are present.
- Although very rare, an obturator hernia is considered to have one of the highest mortality rates of abdominal hernias.
- If in doubt, surgical referral should be sought early to optimise diagnostic confirmation and reduce surgical delay to theatre.