Case
A man aged 30 years presented to the general practitioner (GP) with a history of moderate pain and eyeball protrusion in his right eye immediately after being in handstand position. Symptoms began three months prior; however, they ceased spontaneously after 2–3 minutes. One week prior, he noted symptoms worsened and took almost one hour to resolve. On questioning, the patient revealed he was a professional acrobat. He had no other symptoms, including diplopia, hair loss, weight loss or any other personal or familiar history of ophthalmic and/or systemic diseases. His blood pressure was 101/64 mmHg. Physical examination was negative for skin lesions and/or hair loss. Ocular examination revealed no signs of conjunctival injection, chemosis, eyelid oedema, retraction and/or lag (a higher-than-normal upper eyelid) or restricted extraocular movements. There were no signs of an infectious process, such as fever, palpebral oedema, tenderness and/or redness. Visual acuity, confrontation visual field testing and pupillary responses were normal. No proptosis was observed before and after performing the Valsalva manoeuvre. However, after instructing the patient to stand on his hands, proptosis was noted in the right eye (Figure 1). Colour perception was normal (Ishihara test). Fundus evaluation with a direct ophthalmoscope disclosed an apparently normal optic nerve. Laboratory tests, including thyroid function tests, were negative. Therefore, the GP referred the patient to a tertiary eye care centre for further investigation.
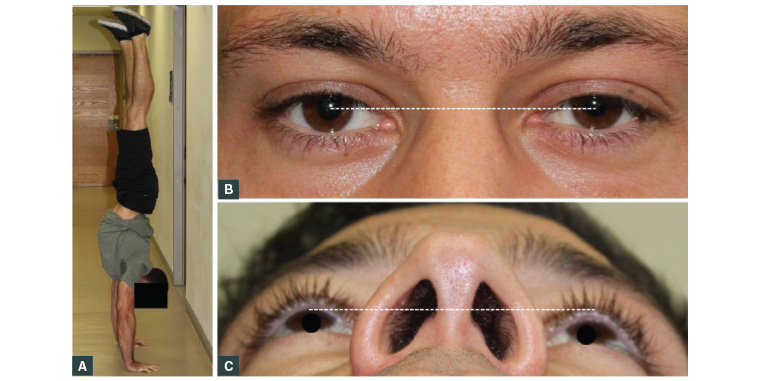
Figure 1. Clinical photographs taken of the patient at the first visit
A. Patient in handstand position; B. Clinical photograph depicting subtle proptosis of the right eye; corneal reflex appears slightly lower from the upper eyelid when compared with the left eye (white line); C. Worm’s-eye view showing marked proptosis of the right eye (white line)
Question 1
What is the most likely diagnosis?
Question 2
What differential diagnosis should be considered?
Question 3
What tests are recommended for patients with proptosis?
Answer 1
Although uncommon, the most likely diagnosis is an orbital varix. Orbital varices comprise up to 2% of orbital masses.1 They are vascular lesions of the orbit known as ‘venous vascular malformations’.2 A study performed by Shields et al revealed that vasculogenic lesions (17%), including orbital varices, followed by inflammatory (11%) and lymphoid or leukaemic lesions (10%) were the most common causes of orbital masses and simulating lesions.1 No diagnostic criteria exist; however, fluctuating periorbital pain, varying degrees of proptosis, haemorrhage, and thrombosis in association with increased venous pressure may indicate an orbital varicosity.3 A handstand position, as with other Valsalva manoeuvres (eg coughing, bending, straining), increases venous pressure. Table 1 shows the main differential diagnosis of vascular lesions of the orbit.2,4
| Table 1. Most common differential diagnosis of the vascular lesions of the orbit2,4 |
| Lesion |
Age (years) |
Sex |
Does the lesion increase in size with Valsalva? |
Pain |
Proptosis |
Haemorrhage |
Spontaneous involution |
| Capillary hemangioma2 |
0–6* |
F > M |
Yes |
Absent |
Develops slowly |
Very rare |
Very common |
| Cavernous venous malformation2 |
43–48† |
F > M |
No |
Rare |
Develops slowly |
Rare |
Absent |
| Orbital venous varices2 |
20–30 |
F = M |
Yes |
Rare |
Fluctuating |
Common‡ |
Common |
| Venous lymphatic malformation2 |
0–16 |
F = M |
No |
Present |
Develops slowly |
Common |
Absent |
| Orbital AVF4 |
33–82 |
M > F |
Yes |
Rare |
Pulsatile, progressive |
Common |
Absent |
*Most common orbital vascular tumour in children
†Most common orbital vascular lesion in adults
‡Most common cause of spontaneous orbital haemorrhage
AVF, arteriovenous fistula; F, female; M, male |
Answer 2
Eye pain and proptosis may be associated with sight- and life-threatening conditions; thus, all information regarding the onset, laterality, severity and spontaneous resolution of symptoms should be obtained. Thyroid eye disease, the most common cause of unilateral and bilateral asymmetric proptosis, must be excluded.5 However, thyroid eye disease is usually associated with eyelid retraction and lid lag.5 Orbital cellulitis – characterised by fever, rapid-onset inflammation and severe pain on extraocular movements – should be ruled out.6 Tumours including optic nerve sheath meningioma and glioma, orbital rhabdomyosarcoma and primary melanoma, leukaemic and lymphoid lesions, and metastases must be immediately excluded. However, malignant lesions rarely present in the setting of acute-onset proptosis.1,6 It is also important to consider cystic lesions,1 ptosis and diplopia caused by idiopathic orbital inflammation,7 vasculitic processes and osseous or cartilaginous lesions.1
Answer 3
In a patient with proptosis, visual acuity, colour perception, confrontational visual fields and the pupillary response (mainly for the presence of relative afferent pupillary defect) are straightforward tests that can be performed by the GP to assess for the presence of compressive optic neuropathy. Although slit-lamp examination is recommended, it is not always available in the primary care setting. Thus, the direct ophthalmoscope may be useful to detect alterations that warrant immediate evaluation by an eye care specialist.
Hertel ophthalmometry is an office-based procedure that measures the axial position of the eyes. Values range depending on the population studied. In Caucasian males, a value of 16.5 mm with a difference <2 mm between the eyes is considered normal.8
Case continued
The orbit and oculoplastic specialist performed Hertel ophthalmometry, which measured 16 mm at rest; however, after instructing the patient to stand on his hands, proptosis of the right eye was noted, and Hertel ophthalmometry measured 19 mm. Slit-lamp evaluation revealed a healthy ocular surface, with no staining, and a normal intraocular pressure. The optic nerve and retina were also normal.
Question 4
What imaging studies are recommended?
Answer 4
Imaging techniques can easily identify an orbital varix. In patients with an orbital varix, ultrasonography of the orbit reveals an anechoic bulbar lesion that, when it exhibits intrinsic blood flow during the Valsalva manoeuvre, is indicative of a varix. Doppler ultrasonography depicts reversal of flow toward the transducer during the Valsalva manoeuvre.2,9 Nevertheless, a dynamic contrast computed tomography (CT) scan in prone position or while performing the Valsalva manoeuvre is the gold standard. Orbital CT shows an enhancing lesion that increases in size while in prone position or while performing the Valsalva manoeuvre. Moreover, calcified phleboliths may be observed.9 When thrombosed, orbital varices may or may not show contrast enhancement; thus, a thrombus extending to the cavernous sinus may go unnoticed.3
Case continued
After the patient assumed a handstand position for one minute, a CT scan was performed, and it showed a well-defined soft tissue mass of 16.8 × 12.1 × 16 mm located mid-inferiorly to the medial rectus muscle with slight superolateral globe displacement (Figure 2). Orbital ultrasonography (Figure 3) depicted a lesion with similar characteristics to those found on the CT scan. After exploring with colour Doppler, no blood flow was observed within the mass, but multiple adjacent low-flux vessels were present. These findings confirmed the diagnosis of an orbital varix.
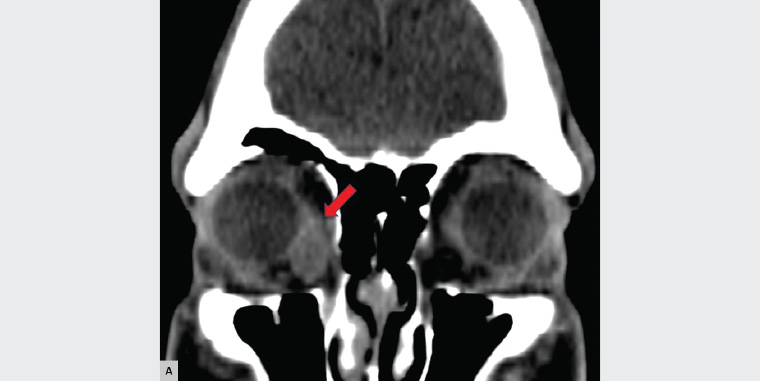
Figure 2. Coronal non–contrast enhanced computed tomography scan showing a right orbital mass (red arrow) with well-defined borders located mid-inferiorly to the medial rectus muscle and slight superolateral globe displacement
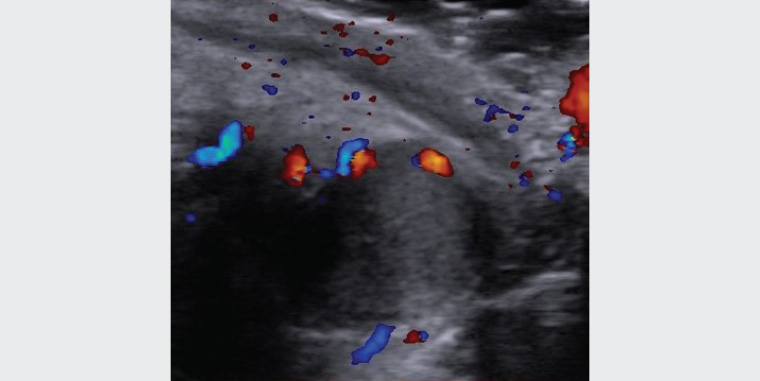
Figure 3. Doppler colour ultrasound showing low-flow vessels adjacent to the mass and absent internal blood flow
Question 5
What is the treatment for orbital varices?
Answer 5
Most orbital varicosities are asymptomatic and compliant with conservative management with serial imaging follow-up.10 Surgery is required in the presence of disfiguring proptosis, severe pain and vision loss related to optic nerve compression.3 Excision of the varix via a transconjunctival anterior orbitotomy approach is the treatment of choice. The transconjunctival approach is associated with a lower incidence of complications (eg postoperative eyelid malposition, scar formation), better aesthetic outcomes and a more rapid recovery when compared with a transcutaneous approach. Thus, it may be considered the gold-standard surgical approach when accessing the inferior orbit.11 Unfortunately, recurrences (14.3%) are common.12 Recurrences usually occur because of an incomplete excision secondary to the inability to elicit venous distension during surgery.10 To avoid subtotal excision, the surgeon must excise the varix as close to the orbital apex as possible. In cases of posterior or deeper varices, embolisation with microcoils, as well as glue and/or n-Butyl cyanoacrylate injection may be performed to reduce intraoperative bleeding.2,10
Case continued
Although this case was amenable for conservative management, a shared decision to surgically remove the varix was made on the basis of the patient’s profession. The varix was totally excised via an anterior inferior transconjunctival orbitotomy (Figure 4). A tissue sample was sent to the pathology department, which reported a dilated venous structure with an irregular wall and thrombosis. At 12 months’ follow-up, the patient had complete resolution of symptoms. At the same visit, Hertel ophthalmometry was performed, which revealed no proptosis before and after instructing the patient to assume a handstand position.
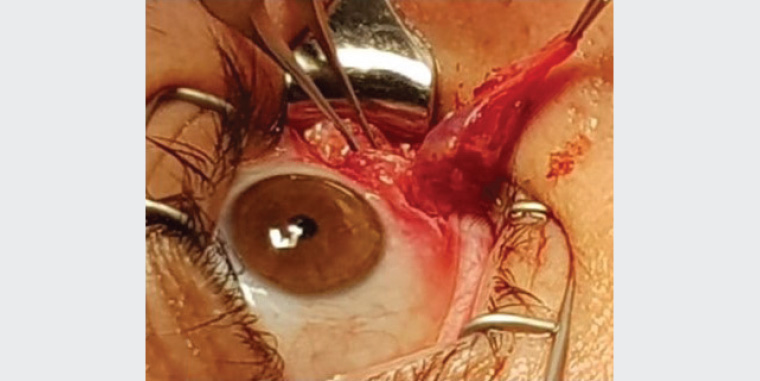
Figure 4. Photograph illustrating the thrombosed right orbital varix excised via an anterior inferior transconjunctival orbitotomy approach
Key points
- An orbital varix is an uncommon cause of orbital mass that is usually amenable to conservative management.
- A thorough clinical history and physical examination aided by laboratory tests and imaging studies are required to exclude potentially sight- and life-threatening diseases.
- In a patient with proptosis associated with severe pain, vision loss, relative afferent pupillary defect, decreased colour perception and/or signs of infection, urgent specialist referral is required to rule out potentially sight- and life-threatening diseases.