In response to concerning evidence that people with mental illness have poorer physical health and lower life expectancies than those without a mental illness, the Fifth National Mental Health Plan identified improving the physical health of people with mental illness as a key priority.1
In the 2015 National Health Survey, 16% of Australians self-reported that they had both a mental health or behavioural condition and a physical health condition.2 The 2010 National Survey of High Impact Psychosis (SHIP), which surveyed 1825 Australians living with a psychotic illness on a range of topics including their physical health and health service use, reported higher rates of chronic physical illness and biomedical risk factors when compared with the general population.3–5
Information on the physical health of general practice patients in Australia with severe and/or long-term mental illness (SMI) is limited. This is despite data suggesting that most patients with a psychotic illness regularly visit a general practitioner (GP) to discuss a physical health condition.3,4
This study explored the sociodemographic characteristics of Australian general practice patients with a record of SMI. It compared the prevalence of selected physical health conditions and biomedical risk factors among these patients with patients who do not have a record of SMI.
Methods
A cross-sectional study was conducted using MedicineInsight, a national general practice dataset managed by NPS MedicineWise, with funding support from the Australian Government Department of Health.6 MedicineInsight extracts and collates longitudinal, de-identified patient data from clinical information systems (Best Practice and Medical Director 3), including patient demographics, clinical encounters (excluding progress notes), diagnoses and prescriptions.
There were 452 general practice sites that met the researchers’ standard data quality criteria (established for at least two years, no significant data interruptions and with at least 50 patients) and were included in the present study. Eligible patients were aged ≥15 years, had visited one of the general practices at least twice between 1 January 2017 and 31 December 2018, and were still alive at study end. Children were excluded because rates of mental illness begin to rise from adolescence onwards.7
The researchers developed coding algorithms for selected health conditions using coded and free-text data from the diagnosis, reason for encounter and reason for prescription fields. Patients were classified as having a severe mental illness if there was any record of schizophrenia or bipolar disorder at any time from the patient’s earliest record up to 31 December 2018. As a result of the nature of routinely collected data, information on depression or anxiety disorder severity was often missing, so patients with these conditions were included if they had at least two records of depression or an anxiety disorder recorded at least six months apart but within a consecutive two-year period at any time from the patient’s earliest record up to 31 December 2018. For the analysis, these two cohorts of patients (ie those with bipolar disorder or schizophrenia, and those with long-term depression or anxiety) were combined into a single group described as having SMI. A full list of the terms used to identify SMI is in Appendix 1.
Patients identified as having an alcohol or opioid use disorder (Appendix 1) but not SMI were identified but are not discussed further in this article. The general patient population (no SMI group) was defined as eligible patients with no record of SMI or alcohol or opioid use disorder.
Study outcomes
Sociodemographics included age, sex, socioeconomic status and remoteness. Patients’ postcodes were used to determine socioeconomic status using Australian Bureau of Statistics Index of Relative Socio-Economic Advantage and Disadvantage (IRSAD)8 and remoteness areas.9 Patients were classified as having hypertension, dyslipidaemia or one of the selected physical health conditions if such a diagnosis had been recorded at any point in the clinical record from the patient’s earliest record up to 31 December 2018. Information about smoking status and alcohol intake was collected from the clinical record. Patients were classified as being obese if body mass index (BMI) was recorded, or calculated using the most recently recorded weight and height, to be ≥30 kg/m2.
Statistics
Study outcomes included descriptive statistics (percentages and robust 95% confidence intervals [CI] that adjusted for clustering by practice). The age- and sex-standardised prevalence of each physical condition and risk factor for patients with SMI was calculated using direct standardisation of the MedicineInsight general patient population (those without SMI or substance use disorder; males and females only) as the reference population. Data manipulation and analyses were conducted using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA) and Stata/IC version 12.1 (StataCorp LP, Texas, USA).
The association between SMI and the two outcomes, physical conditions or risk factors, was explored via logistic regression (restricted to patients aged 15–75 years to avoid mortality attrition bias) using generalised linear modelling. The Stata svy command with logistic estimation was used to account for clustering by practice site. To adjust for potential confounders, purposeful selection of covariates and change-in-estimate criterion were used. The base model included SMI as the primary risk factor and age and sex as a priori confounders. Other potential confounders were added to the unadjusted model if their inclusion (one at a time) resulted in an absolute change to the odds ratio (OR) of 10% or greater. All confounders included in the final regression models for health conditions and biomedical risk factors were statistically significant at P value <0.05. The interaction between sex and age was tested for all regression models and did not have a statistically significant effect.
Ethics
This study was approved by The Royal Australian College of General Practitioners’ National Research and Evaluation Ethics Committee (19-003) and the MedicineInsight independent external Data Governance Committee (DG 2019-011) in April 2019.
Results
Of the almost 1.94 million patients eligible for this study, 173,861 (9.0%; 95% CI: 8.5, 9.4) had a record of SMI (Figure 1). The mental illnesses most commonly recorded were long-term anxiety (108,660 patients) and long-term depression (93,578 patients). Many patients had more than one mental illness (Table 1).
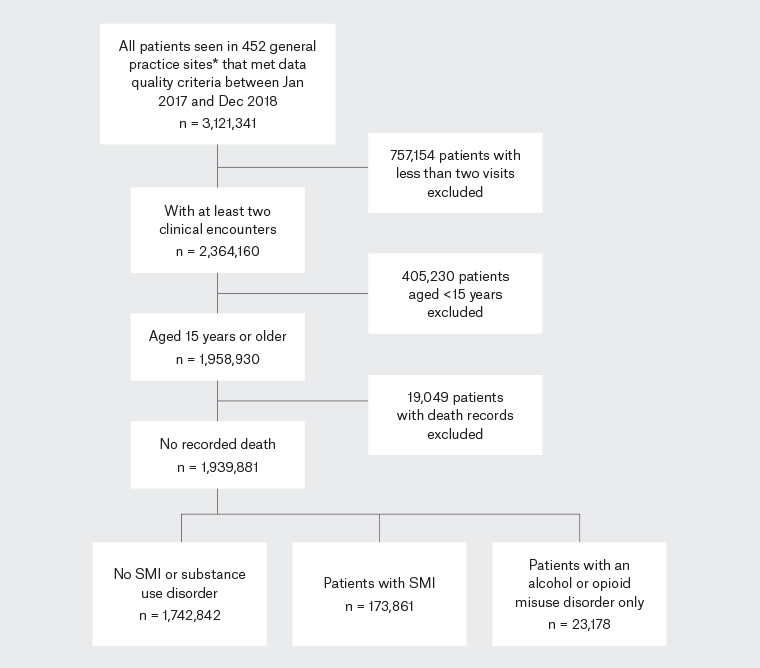
Figure 1. Patient eligibility
*The term ‘general practice site’ is used to describe one or more practices that share the same installation of the clinical information system (CIS). For example, one organisation may consist of a number of geographically diverse general practices that all share the same CIS, or a site may be a single general practice. There were 497 individual general practices included in the 452 general practice sites.
| Table 1. Patient prevalence of SMI* in the MedicineInsight general practice population (n = 1,939,881) |
| Mental illness* |
All eligible MedicineInsight patients |
| Number |
% (95% CI) |
| Any SMI |
173,861 |
9.0 (8.5, 9.4) |
| Schizophrenia |
15,156 |
0.8 (0.7, 0.9) |
| Bipolar disorder |
23,788 |
1.2 (1.2, 1.3) |
| Long-term anxiety disorder |
93,578 |
4.8 (4.5, 5.1) |
| Long-term depression |
108,660 |
5.6 (5.2, 6.0) |
| Any SMI plus a substance use disorder |
13,766 |
0.7 (0.6, 0.8) |
*Patients may have more than one type of SMI
CI, confidence interval; SMI, severe and/or long-term mental illness |
Women made up a larger proportion of people with SMI (64.4%; 95% CI: 63.6, 65.3) than in the population without SMI (57.0%; 95% CI: 56.5, 57.6; Appendix 2). While the average age of both groups was similar (48.5 years, compared with 47.9 years), significantly more patients were aged 35–64 years, and significantly fewer aged 15–24 years and ≥75 years, in people with SMI when compared with the group without SMI (Figure 2). The distribution of rurality and socioeconomic status was similar (Appendix 2).
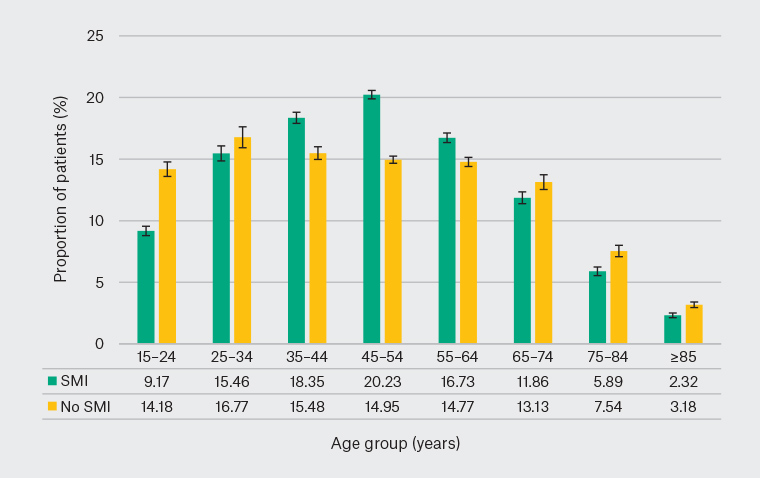
Figure 2. Age distribution of the patient populations with and without severe and/or long-term mental illness (SMI)
Having a record of SMI increased the likelihood that a patient would be identified as having each of the biomedical risk factors (Table 2). Patients with SMI were more than twice as likely to be smokers or risky drinkers and were significantly more likely to have hypertension or dyslipidaemia or be identified as being obese.
| Table 2. Prevalence and odds of having a biomedical risk factor among Australian general practice patients with and without SMI |
| Risk factor |
Prevalence* in patients with SMI (n = 173,831) |
Prevalence in population without SMI† (n = 1,742,735) |
Odds ratio (95% CI)‡ |
| % (95% CI) |
% (95% CI) |
Crude |
Adjusted |
| Dyslipidaemia |
25.21 (24.47, 25.96) |
17.67 (16.98, 18.35) |
1.69 (1.63, 1.76) |
1.79 (1.72, 1.86) |
| Hypertension |
27.25 (26.81, 27.69) |
22.11 (21.24, 22.99) |
1.40 (1.35, 1.45) |
1.48 (1.44, 1.53) |
| Moderate-to-heavy drinker |
4.71 (4.23, 5.25) |
2.29 (2.07, 2.51) |
2.27 (2.10, 2.47) |
2.32 (2.15, 2.51) |
| Obesity |
29.04 (28.17, 29.92) |
18.56 (17.80, 19.31) |
2.00 (1.94, 2.06) |
1.91 (1.85, 1.97) |
| Current or past smoker§ |
46.88 (45.72, 48.04) |
30.11 (29.24, 31.01) |
2.25 (2.17, 2.34) |
2.24 (2.17, 2.32) |
*Age- and sex-standardised to the non-SMI population
†Patients with neither SMI nor a substance use disorder
‡Logistic regression modelling only included patients aged 15–75 and who were identified as male or female (n = 1,734,331). All models were adjusted for sex and age only.
§Smoking status was missing for 7.0% of the SMI population and 15.2% for the non-SMI population.
CI, confidence interval; SMI, severe and/or long-term mental illness |
Almost three-quarters of patients with a record of SMI (71.1%) had at least one of the selected physical health conditions, compared with 53.6% of people without SMI (Table 3). The odds of having at least one physical health condition among patients with SMI was double that of patients without SMI (adjusted OR: 2.2; 95% CI: 2.1, 2.3).
| Table 3. Prevalence and odds of having a physical health condition among Australian general practice patients with and without SMI |
| Condition |
Prevalence* in patients with SMI (n = 173,831) |
Prevalence in population without SMI† (n = 1,742,735) |
Odds ratio (95% CI)‡ |
| % (95% CI) |
% (95% CI) |
Crude |
Adjusted |
Confounders included in the model |
| One or more conditions |
71.13 (70.33, 71.93) |
53.61 (52.27, 54.95) |
2.36 (2.27, 2.45) |
2.19 (2.12, 2.26) |
Sex, age, current/past smoking, obesity |
| Arthritis |
27.40 (26.70, 28.10) |
18.71 (17.87, 19.54) |
1.76 (1.69, 1.84) |
1.62 (1.57, 1.68) |
Sex, age, dyslipidaemia, hypertension, current/past smoking, obesity |
| Asthma |
22.18 (21.56, 22.81) |
13.31 (12.88, 13.73) |
1.89 (1.83, 1.96) |
1.78 (1.72, 1.83) |
Sex, age, obesity |
| Atrial fibrillation |
3.58 (3.47, 3.70) |
3.08 (2.89, 3.27) |
1.10 (1.04, 1.16) |
1.09 (1.05, 1.14) |
Sex, age, dyslipidaemia, hypertension, current/past smoking, obesity |
| Back pain |
35.09 (34.18, 36.02) |
19.42 (18.79, 20.04) |
2.42 (2.34, 2.49) |
2.12 (2.06, 2.18) |
Sex, age, current/past smoking, dyslipidaemia |
| Cancer |
19.44 (18.56, 20.34) |
14.90 (13.99, 15.82) |
1.47 (1.40, 1.55) |
1.39 (1.34, 1.45) |
Sex, age, current/past smoking, obesity |
Cardiovascular disease§
|
10.19 (9.94, 10.46) |
6.68 (6.31, 7.05) |
1.62 (1.55, 1.70) |
1.50 (1.46, 1.54) |
Sex, age, dyslipidaemia, hypertension, current/past smoking, obesity |
| Chronic kidney disease |
2.39 (2.17, 2.63) |
1.64 (1.48, 1.79) |
1.58 (1.49, 1.69) |
1.35 (1.27, 1.43) |
Sex, age, dyslipidaemia, hypertension, current/past smoking, obesity |
| Chronic liver disease |
0.57 (0.52, 0.62) |
0.17 (0.16, 0.19) |
3.75 (3.41, 4.12) |
3.03 (2.77, 3.32) |
Sex, age, hypertension, current/past smoking, moderate-to-heavy drinking, obesity |
| COPD |
7.39 (6.99, 7.82) |
3.27 (3.07, 3.47) |
2.78 (2.64, 2.94) |
2.27 (2.17, 2.36) |
Sex, age, dyslipidaemia, hypertension, current/past smoking, obesity |
| Gastro-oesophageal reflux disease |
29.05 (28.15, 29.97) |
14.93 (14.31, 15.54) |
2.51 (2.42, 2.60) |
2.22 (2.16, 2.29) |
Sex, age, dyslipidaemia, current/past smoking, obesity |
| Heart failure |
2.55 (2.39, 2.72) |
1.55 (1.42, 1.68) |
1.79 (1.65, 1.93) |
1.54 (1.43, 1.67) |
Sex, age, dyslipidaemia, hypertension, current/past smoking, obesity |
| Osteoporosis |
8.63 (8.31, 8.97) |
6.15 (5.77, 6.54) |
1.58 (1.51, 1.66) |
1.49 (1.43, 1.55) |
Sex, age, dyslipidaemia, hypertension |
| Type 2 diabetes |
9.94 (9.63, 10.26) |
7.16 (6.84, 7.49) |
1.52 (1.47, 1.58) |
1.19 (1.15, 1.22) |
Sex, age, dyslipidaemia, hypertension, current/past smoking, obesity |
*Age- and sex-standardised to the general population
†Patients with neither SMI nor a substance use disorder
‡Logistic regression modelling only included patients aged 15–75 and who were identified as male or female (n = 1,734,331). Potential confounders included age, sex, socioeconomic status, remoteness, smoking status (current/past), obesity, moderate-to-heavy drinking, dyslipidaemia and hypertension.
§Includes coronary artery disease, peripheral vascular disease, stroke and transient ischaemic attack
CI, confidence interval; COPD, chronic obstructive pulmonary disease; SMI, severe and/or long-term mental illness |
The most prevalent of the selected physical health conditions among all patients were back pain, gastro-oesophageal reflux disease (GORD), arthritis and cancer (Table 3). The risk of every single physical health condition was significantly higher for patients with SMI when compared with patients without SMI. Having SMI was correlated with a doubling of the odds of back pain, COPD and GORD, and tripled the odds of chronic liver disease. The odds of cardiovascular disease, heart failure, dyslipidaemia, hypertension and osteoporosis were associated with at least a 50% increase for patients with SMI, while the odds of type 2 diabetes increased by 19%.
Discussion
This large study increases understanding of the physical health conditions and biomedical risk factors of general practice patients with a record of SMI. While the SHIP provided some information on GP visits among people with a mental illness, it focused on people with a psychotic illness whereas this study also included patients with long-term depression and long-term anxiety disorders.
Consistent with other Australian studies, there was an association between having SMI and physical ill health.2–5 For every biomedical risk factor and health condition investigated, this risk was higher for people with SMI than for those without SMI. The proportion of MedicineInsight patients with SMI with a recorded diagnosis of kidney disease, arthritis, back pain or asthma was similar to figures reported among SHIP respondents. However, a smaller proportion of MedicineInsight patients had a record of cardiovascular disease, diabetes, hypertension, obesity or dyslipidaemia than in the SHIP.3,4 For example, 9.9% of MedicineInsight patients had a record of diabetes, compared with 20.5% of SHIP respondents. These differences may be due to the inclusion of patients with long-term depression or anxiety disorders in the MedicineInsight cohort. People with a psychotic illness are at particular risk of cardiovascular events and diabetes, due to the illness itself and the side effects of medicines used to manage psychosis.3–5 Therefore, a study that only includes such patients is likely to report higher rates of these conditions than one that also included people with depression or anxiety disorders.
The Fifth National Mental Health Plan has made explicit reference to the use of electronic medical records to develop and measure indicators of physical health in people with mental illness.1 The present study goes some way towards developing a baseline for measuring future changes among Australian general practice patients.
This is a cross-sectional study and cannot provide information on causality or temporality. It cannot distinguish if patients were initially diagnosed with mental illness, which then led to poorer physical health, or vice versa. The reasons for poorer physical health among people with a mental illness are complex. The medicines used to manage mental illnesses can have side effects that increase the risk of physical illness. Mental health treatment may be prioritised over treatment of physical health conditions, patients may experience barriers to accessing healthcare and patients may be more likely to be exposed to lifestyle risk factors and socioeconomic disadvantage. Being diagnosed with physical health conditions can also have an adverse impact on mental health.1,10,11 It would be interesting to further explore causality using MedicineInsight data to identify a cohort of patients newly identified as having a mental health condition but no physical health condition, or vice versa, and follow them over time.
As a result of the nature of routinely collected data, information on whether a patient had mild, moderate or severe depression or anxiety was often missing. For this reason, duration of illness was used as a proxy of severity. However, this means patients with long-term but mild or moderate depression or anxiety (not normally considered to have SMI) may have been included and potentially reduced the strength of associations seen in this study.
Practice participation in the MedicineInsight program is voluntary, and practices are not randomly selected. As such, practices and GPs working in them may differ from the average Australian general practice. However, when compared with Medicare Benefits Schedule data, MedicineInsight patients have similar demographics to all patients who visit a GP.6 While the study attempted to control for confounders, it is possible that some residual confounding is present (eg if the marker of socioeconomic status based purely on patient postcode is relatively insensitive). In addition, the study relies on the extraction of information from clinical information software and may underestimate prevalence if information is not recorded in a field accessible to MedicineInsight. Patients may attend multiple practices so may be double counted if they attend multiple MedicineInsight practices – previous work estimates this to be fewer than 4.0% of patients.6 Similarly, data on patients who also attend non-MedicineInsight practices will be missing.
Similar to other Australian studies, these findings highlight the importance of addressing physical health needs in people with SMI.2–5,10,11 Three-quarters of Australians with a mental illness who seek medical help during a year consult a GP rather than specialist mental health services, and Australians with a psychotic illness visit a GP on average nine times per year.4,11 While people with a mental illness have a high morbidity burden, many of the risk factors and conditions identified are modifiable or manageable. If risk factors precede physical or mental health conditions, then GP management of these risk factors becomes increasingly important. Efforts to manage physical health conditions that may exacerbate mental illness, or vice versa, may improve patient wellbeing.