Case
A student aged 15 years was brought by his mother in early 2019 to a Malaysian suburban primary care clinic. He had a four-day history of cough associated with right-sided chest pain on deep inspiration. The patient and his mother denied any significant past medical or family history.
Examination revealed a tall adolescent with a body mass index of 18.2 kg/m2. His temperature was 37.3 °C, blood pressure was 120/70 mmHg, pulse rate was 87 beats/min and respiratory rate was 19 breaths/min. The patient’s posterior pharynx was inflamed. He had multiple small (<0.5 cm) non-tender cervical lymph nodes. Chest expansion and air entry were reduced over the right upper lung, with dullness on percussion. Other examination was not significant.
Question 1
On the basis of the clinical features, what diagnosis must be considered?
Question 2
What is the most appropriate initial investigation to order?
Answer 1
Despite the short history and absence of classical symptoms of fever, night sweats and weight loss, tuberculosis (TB) must be considered because it is endemic in Malaysia with a rising incidence.1
Answer 2
The most appropriate initial investigation is urgent chest radiography.
Case continued
Chest radiography (Figure 1) showed consolidation in the right upper lobe with cavitation within (hallmark for TB) and right upper lobe fibrosis evidenced by elevation of the horizontal fissure.
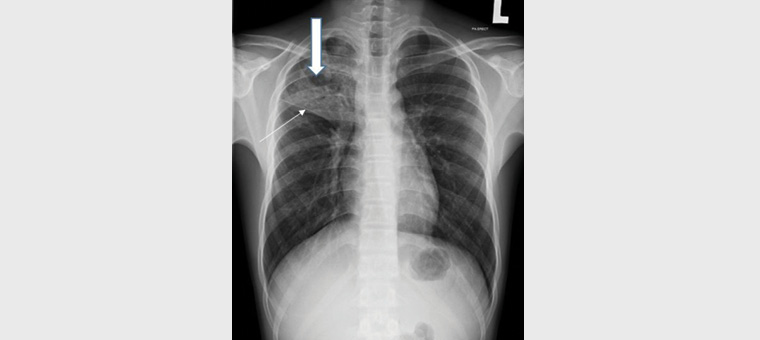
Figure 1. Chest radiograph from 2019 shows consolidation in the right upper lobe with cavitation within (thick arrow). Elevation of the horizontal fissure (thin arrow) and right hilum represents right upper lobe fibrosis.
TB was confirmed by a positive sputum test using the preferred light-emitting diode fluorescence microscopy.1
After a discussion with the patient and his mother about the diagnosis, the patient’s mother admitted that he had first contracted pulmonary TB in 2017 and was treated until early 2018, when he was pronounced ‘cured’. Their reason for non-disclosure was fear of discrimination and stigmatisation.
Question 3
What are the common reasons for non-disclosure of TB by patients and their families?
Answer 3
Globally, the most common reason for non-disclosure is stigmatisation due to the association of TB with poverty, risk of transmission and death.2,3 In Malaysia, TB has been perceived as shameful.4 The level of awareness is low;4–6 in one study of people living in Kudat, Sabah, participants expressed that getting TB was embarrassing (41%), too sensitive to discuss (16%) and a disgrace to the family (4%).4 Overall, attitudes towards patients with TB are poor, as most people would avoid meeting them.5,6 This is not unlike the current stigmatisation of COVID-19.7
Case continued
Over the years, there was a strong history of TB involving different generations of the patient’s family (ie grandfather, granduncle, parents and siblings) infected at different times. The family of eight lived in a small, crowded single-storey terrace house with three rooms. To avoid a recurrence after completing treatment in 2018, the patient was moved to live with an uninfected aunt.
Question 4
Is there a genetic basis for TB susceptibility?
Question 5
What is the importance of establishing whether this recurrent TB is a relapse or re-infection?
Answer 4
Recent evidence has shown a genetic basis for TB susceptibility beyond close contact.8,9 However, the current prohibitive cost for molecular testing precludes its routine use in TB control.
Answer 5
The importance lies in disease management. Relapse, defined as reactivation of the original infecting TB strain, must be managed by a TB specialist. Conversely, re-infection, defined as a new TB bacilli strain infection, can be managed in primary care with the standard first-line six-month regimen: two months of daily ethambutol, isoniazid, rifampicin and pyrazinamide followed by four months of daily rifampicin and isoniazid.
True relapse can only be confirmed with molecular techniques such as whole-genome sequencing. As these expensive tests are not readily available in Malaysia, chest radiography and response to treatment are used to differentiate relapse from re-infection. Chest radiography performed at the time of initial diagnosis of TB in 2017 (Figure 2) showed left upper zone consolidation with complete resolution following treatment in 2018 (Figure 3). The new infection is in the right lung (Figure 1).
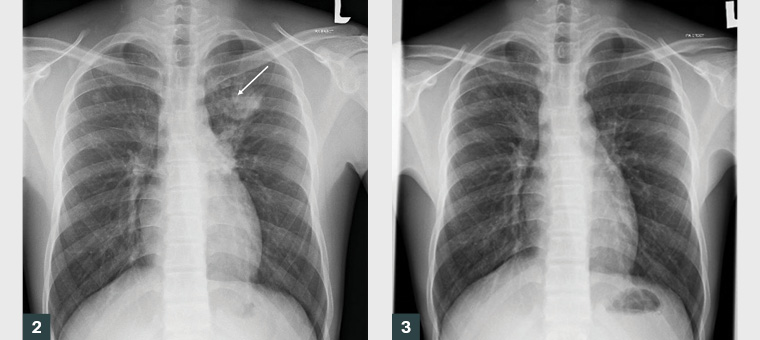
Figure 2. Chest radiograph from 2017 at initial diagnosis of pulmonary tuberculosis shows a focal area of consolidation (arrow) in the left upper zone.
Figure 3. Chest radiograph from 2018 shows complete resolution of the left upper lobe consolidation, with no residual changes following tuberculosis treatment.
Case continued
As this may have been a recurrent infection, the patient was referred to a chest physician for further management.1 The specialist ruled that this was most likely a new infection, based on the different anatomical location (Figures 1 and 2) and complete resolution after TB treatment (Figure 3). The patient was referred back to primary care for management.
Question 6
What public health measures must be taken to prevent transmission of active pulmonary TB?
Question 7
Beside diagnosis, what other problems are anticipated with adolescents with TB?
Answer 6
Public health measures1 include early disease detection, mandatory disease notification, meticulous contact tracing and screening, self-isolation and use of surgical masks.
Answer 7
Medication adherence and treatment completion are particularly problematic among adolescents.10 Direct observation of treatment by healthcare staff or a family member, text messaging reminders and home visits can prevent non-adherence.1
Key points
- Pulmonary TB in the young can present acutely without classical constitutional symptoms.
- When signs and symptoms are incongruent, it is important to broaden the differential diagnosis.
- Beware of non-disclosure of stigmatising diseases during an initial patient encounter