Primary healthcare (PHC) services in Australia deliver comprehensive, continuous, preventive and treatment services within community settings and include a broad range of healthcare providers, including general practitioners (GPs), nurses, allied health professionals and pharmacists who work together to provide a first point of contact for patients within the healthcare system. These services are usually provided through general practices (or PHC centres) that deliver ‘comprehensive, continuous and person-centred care’.1 While PHC services are diverse and wide ranging, the management of complex and chronic disease represents a key responsibility and challenge for PHC providers. As the chronic disease burden places increasing pressure on the healthcare system, greater collaboration between GPs and other healthcare professionals is required to provide high-quality care that is responsive to such demands.
Non-dispensing pharmacists (NDPs), also referred to as clinical pharmacists, practice pharmacists or general practice–based pharmacists, are pharmacists who ‘deliver professional services from or within a general practice medical centre with a coordinated, collaborative and integrated approach with an overall goal to improve the quality use of medications of the practice population’.2 While pharmacists traditionally deliver care through independent services, there is increasing recognition of the value of integrating pharmacists into primary services as part of a team-based model to provide collaborative and effective care.3 Within this model, NDPs deliver a range of clinical services, both directly to patients and to other healthcare professionals, to optimise medical therapy, provide medical management services, promote medication safety initiatives, improve health literacy and educate and empower patients to employ effective medication self-management.3,4 This role does not include medication dispensing services, such as those provided in community pharmacy settings. Statements released by the Australian Medical Association and The Royal Australian College of General Practitioners (RACGP) promote the integration of NDPs into primary care to improve the quality use of medications, reduce adverse drug events, as well as to provide a financial benefit to the healthcare system, although the RACGP acknowledges that ‘more robust research relevant to the Australian healthcare context is required to understand the true effect on health outcomes’.3,5
This team-based model of care is already in place in healthcare systems overseas, including in the USA and the UK, and a body of evidence exists to support its benefit to patients and other healthcare providers. However, this model has not been readily adopted in the Australian context, and there is a lack of robust evidence examining its effectiveness in Australia. Several international systematic reviews and an umbrella review have explored the effectiveness of pharmacist involvement in the management of patients with chronic disease in a range of healthcare settings by investigating changes in biomedical markers, in prescribing quality, medication adherence and in patient-reported outcomes.6–9 These reviews explored a range of pharmacist interventions delivered in diverse healthcare settings, including in community pharmacies. To better understand the effect of integration of NDPs into PHC settings, an umbrella review of existing systematic reviews and meta-analyses was conducted.
Methods
Umbrella review methods and objective
Umbrella reviews systematically review and summarise the evidence from multiple existing systematic reviews and meta-analyses to allow for rapid review of the evidence base for a particular issue to inform policy makers and clinical decision makers.10
This umbrella review aimed to determine the effectiveness of the integration of NDPs into PHC settings on patient outcomes, such as biomedical markers, prescribing quality and patient-reported outcomes. Integration was defined broadly as any intervention that involved co-location of pharmacists within PHC settings and/or pharmacists who worked as part of multidisciplinary and/or interdisciplinary healthcare teams using a range of integrative processes. These processes include informational methods (shared electronic healthcare records), care coordination for shared assessments and governance frameworks (such as formal partnerships) to deliver a range of clinical services both directly to patients and to other healthcare professionals.11
Literature search
A search of the literature was undertaken between August and December 2019 using PubMed, CINAHL, the Cochrane Database of Systematic Reviews and the JBI Database of Systematic Reviews to identify all relevant systematic reviews and meta-analyses regarding the integration of NDPs in PHC. In addition, a manual review of the reference lists of systematic reviews was performed.
The search strategy, developed in conjunction with a trained librarian, was conducted using the following MeSH and natural language terms and was adapted for each database: (pharmacists OR pharmaceutical services OR non-dispensing pharmacist OR clinical pharmacist OR pharmaceutical care) AND (primary healthcare OR general practice OR family practice OR patient care team OR community health service OR community health centre OR primary care OR outpatient care OR family medicine OR multidisciplinary healthcare team OR team-based care) AND (systematic review OR review). The search terms used were purposefully broad to allow identification of all possible relevant publications. After deliberation, it was decided not to include search terms relating to patient outcomes, as this narrowed the search and eliminated relevant publications. Rather, all publications were manually screened to determine whether patient outcomes were the outcomes of interest. Two independent reviewers (CS and SC) screened the titles and abstracts of all publications for eligibility (based on the inclusion criteria outlined below) and examined the full text of those considered eligible. Searches were limited to English-language articles and those with human participants; a set date range of 1990–2019 was used.
Inclusion criteria
Inclusion criteria used for this review were determined in accordance with the PICO scheme (Population, Intervention, Comparison, Outcome), as outlined in Table 1.10 Inclusion criteria consisted of:
- systematic reviews or meta-analyses (hereinafter referred to as included reviews)
- reviews that examined pharmacists as a member of a PHC team and/or were integrated or co-located within a PHC setting
- reviews that primarily examined adults with chronic disease
- reviews that included patient outcomes.
| Table 1. PICO (Population, Intervention, Comparison, Outcome) scheme of inclusion criteria |
| Parameter |
Description |
| Population |
Inclusion: adults (aged over 18 years), chronic disease, any sex, any country, any ethnicity |
| Intervention |
Inclusion: pharmacist integrated or co-located in PHC setting, provision of direct patient services or participation in the PHC team
Exclusion: pharmacist based in community pharmacy or inpatient setting, or undertaking dispensing role |
| Comparison |
Usual care, lack of intervention |
| Outcome |
Inclusion: patient outcomes (biomedical measures, prescribing quality or appropriateness, medication adherence)
Exclusion: financial outcomes, analysis of interprofessional relationships |
| PHC, primary healthcare |
Patient outcomes were inclusive of changes in biomedical measures, prescribing quality or medication adherence. Articles were excluded if they were unpublished or not clearly a systemic review or a meta-analysis, if they concerned health professionals other than pharmacists, if they investigated pharmacists in a community pharmacy or inpatient setting or if the pharmacist undertook a dispensing role.
Study selection
In total, 589 publications were identified from searching the electronic databases, and an additional two publications from manual searching (500 in PubMed, nine in the Cochrane Database of Systematic Reviews, 28 in CINAHL, 52 in the JBI Database of Systematic Reviews and two from manual searching). Of the 591 publications initially identified, five reviews were selected to include in the umbrella review after removal of duplicates and exclusion of publications that did not meet the inclusion criteria. A PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram outlining the included and excluded studies is presented in Figure 1.12
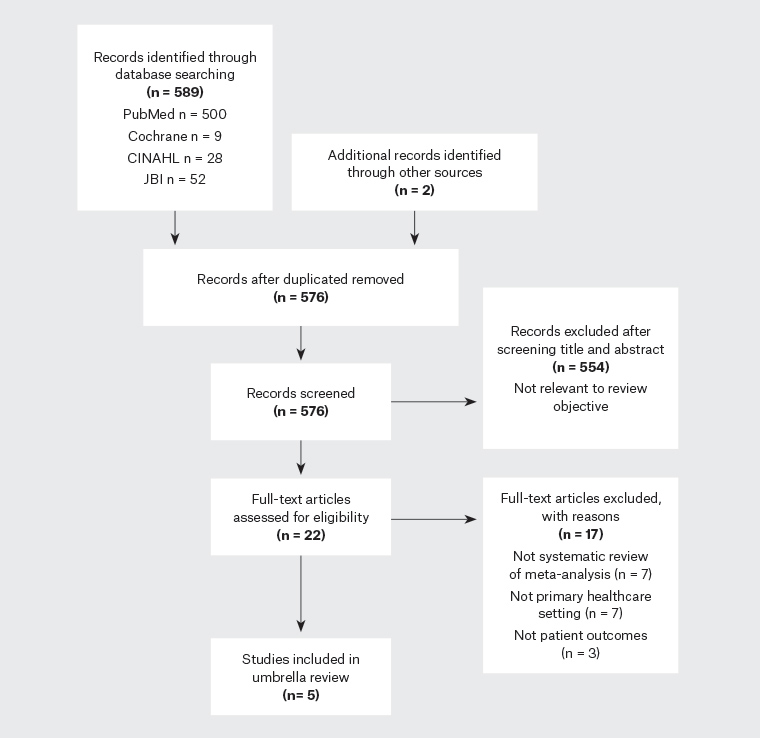
Figure 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of included and excluded studies
Results
Assessment of methodological quality of included studies and quality of evidence
Eligible reviews were assessed for methodological quality using the critical appraisal tool for systematic reviews and research syntheses developed by The Joanna Briggs Institute (Appendix 1).10 Each element of the checklist was designated as being met, not met, unclear or not applicable. This tool allows for an assessment of the quality of the included reviews and was not used as part of the inclusion criteria.
Data extraction and characteristics of included studies
For each eligible review, the following data were extracted: author, year, journal of publication, objective(s) and outcome(s) of interest, type of review, participants, setting, number of databases searched, date range of database search, publication date range, number of studies, types of studies, country of origin and conclusions provided by the authors (Appendix 2).
Of the five included reviews,13–17 all presented a systematic review of the evidence, and two also presented a meta-analysis.14,16 Studies examined in the included reviews comprised randomised controlled trials (RCTs), non-RCTs, quasi-RCTs, cohort studies, controlled before and after studies and pretest–post-test studies.
The studies examined in the included reviews were heterogenous in regard to the integration of NDPs into PHC teams. Involvement of the NDP in the healthcare team ranged from short educational visits from pharmacists to PHC providers, to pharmacists who had a regular relationship with a clinic or health centre, to fully integrated NDPs who were permanently employed by a primary care organisation, had a significant clinical role within the practice and had shared access to information systems and administrative support. One review assessed pharmacists who provided direct patient care within a healthcare team; however, this study involved a number of settings, such as hospital outpatient clinics, community pharmacies, community clinics and primary care physician offices.16 Only 10 of the 35 included studies in this review specified that the nature of the pharmacist intervention was a ‘collaborative practice agreement’.16 All other reviews specified PHC or a related term as a search or inclusion criterion.13–15,17 Only one review assessed the impact of the degree of integration of NDPs into healthcare teams on patient health outcomes in PHC settings.13
All reviews primarily examined interprofessional collaboration between pharmacists and general practitioners (GPs). In terms of characteristics of the patient populations assessed, only two specified particular age ranges (>65 years and >18 years).15,16 Across the included reviews, patients were either categorised according to a particular chronic disease, or were considered more broadly as patients prescribed multiple medications, those at risk of an adverse health issue or those at risk of a medication-related adverse event. Chronic diseases or medication-related issues considered in the reviews included hypertension,13–15,17 dyslipidaemia,13–15,17 diabetes,13–16 metabolic syndrome,13,14 heart failure,13 depression,13,14 osteoporosis,13 cardiovascular disease,13,14 pain,14 chronic obstructive pulmonary disease (COPD),14 menopause14 and polypharmacy.17 One study only investigated diabetes.16 None of the included reviews identified if participants were from marginalised groups, such as Aboriginal and Torres Strait Islander peoples or those residing in remote geographical locations.
In terms of interventions, all reviews considered pharmacist interventions that were educational, clinical or both, and included direct patient services (eg medication reviews) and involvement in team-based care (eg providing recommendations to other healthcare providers or participating in team-based decision making). All reviews, with the exception of one, stipulated that the comparison group was usual care or no intervention.17
Outcomes examined across the included reviews were also heterogenous, consisting of biomedical markers (blood pressure, glycated haemoglobin [HbA1c], cholesterol, lipids, Framingham Risk Score), changes in prescribing practices (prescribing quality, reduction of inappropriate prescribing) and medication adherence, as well as patient-reported factors, such as quality of care, quality of life and satisfaction. Four reviews examined biomedical or clinical markers,12,14,16,17 including HbA1c,13,14,16 lipids,13,14,16,17 blood pressure13,14,16,17 and the Framingham Risk Score.14 Improvement in prescribing practices, medication adherence and the detection of medication-related problems were also outcomes assessed in four reviews.13–15,17 One review focused on changes in prescribing quality by examining the reduction in inappropriate prescribing using one of the following three tools: The American Geriatrics Society Beers Criteria, Screening Tool for Older Persons Prescriptions/Screening Tool to Alert doctors to Right Treatment (STOPP/START) and the Medication Appropriateness Index (MAI).15 Reviews also considered secondary outcomes, such as improvement in quality of care,13,17 improvement in health-related quality of life13,15,17 and patient satisfaction.15,17 One review examined 89 health outcomes inclusive of clinical health outcomes (biomedical markers; eg HbA1c or blood pressure), patient-reported health outcomes (eg quality of life) and proxies of health outcomes (eg medication errors).13 One review also contained a cost analysis of the included studies;17 however, this was disregarded for the purposes of the umbrella review, as cost was not an outcome of interest.
Discussion
Findings
The included reviews examined a range of interventions that were either pharmacist led or involved a pharmacist for a range of diseases or medication-related problems. While most of the studies that were examined in the included reviews were conducted in PHC settings (general practice, family medicine clinic, community health centre), some included hospital outpatient clinics and community pharmacies in their analysis.16 Due to the specific inclusion criteria used, only five reviews were considered eligible for inclusion. Because of this significant heterogenicity and small number of included reviews, a narrative synthesis of the evidence was considered the most appropriate method to discuss the findings.
In four reviews, pharmacist intervention had a positive effect on blood pressure, producing reductions in both systolic blood pressure (SBP) and diastolic blood pressure.13,14,16,17 However, only two reviews stated that these reductions were statistically significant.16,17 Pharmacist intervention was also found to reduce HbA1c in three reviews,13,14,16 and cholesterol in four reviews.13,14,16,17 One study assessed all three of these biomedical markers in patients with diabetes, and found that pharmacist intervention reduced HbA1c, SBP and low-density lipoprotein cholesterol, with significantly improved outcomes compared with the comparison group (P <0.01).16 One review assessed the impact of pharmacist intervention on the 10-year Framingham Risk Score and found a statistically significant reduction in cardiovascular risk (–1.83%).14 However, only two studies were included in this assessment. One review assessed 51 surrogate clinical health outcomes (eg blood pressure, cardiovascular risk, HbA1c) and found a positive effect of pharmacist intervention in 67% (a statistically significantly difference following the intervention compared with controls).13
Three of the reviews assessed prescribing quality. Pharmacist interventions were found to reduce inappropriate prescribing and improve prescribing quality.14,15 Positive effects on medication-related problems and medication adherence were reported.14 One study found that pharmacist intervention showed an improved MAI score and reduced inappropriate prescribing compared to the control group.15 One trial included in the review found that ‘pharmaceutical care’ provided by community pharmacists had no effect on appropriate prescribing.15 Another review found that, while medication reviews and patient prescribing advice achieved one or more of the outcomes of interest in seven of the eight included studies,17 some studies showed no statistically significant improvements and were of poor design.
Other outcomes assessed included secondary or patient-reported outcomes, such as quality of life and patient satisfaction. These were the not the focus of any of the included reviews, and the discussion of these is limited. However, of those reviews that did comment on quality-of-life outcomes, pharmacist interventions were found to have little or no effect on quality of life.13,14,16
Some authors commented on factors considered important to promote the success of NDP integration into primary care teams. In particular, multifaceted interventions (medication reviews, adherence assessments, advice, monitoring) were more likely to improve outcomes, as were those that encouraged verbal and written communication with GPs and patients.14,15 Access to medical notes was also deemed important for success.15 One review assessed the impact of the degree of integration of an NDP into the PHC team on health outcomes.13 Integration was categorised as either none, partial or full, based on organisational, informational, clinical, functional and normative integration. The review found that the degree of integration did not impact health outcomes overall. However, full integration of an NDP (one who is permanently employed as part of a multidisciplinary team with shared access to information and administrative support) had a positive effect on patient-centred pharmacy services (for patients with multimorbidity), such as resolving medication errors (70% of patient-centred services with fully integrated NDPs showed improved health outcomes).13
Limitations of the included reviews
Most of the studies included in the systematic reviews discussed were conducted outside of Australia. Only five of the total studies were conducted in Australia.13,16,17 This limits the applicability of the results to the Australian healthcare context. Also, a number of authors commented that the methodological quality of many of the included studies was poor,14,15,17 and all reviews stated that significant heterogenicity across interventions and outcomes made aggregation and generalisability of results difficult.13–17 There was also a paucity of description pertaining to the type of integrated care delivered in the study interventions; therefore, a meaningful analysis of multidisciplinary and/or interdisciplinary integration was not feasible.
Limitations of this umbrella review
To adhere to the methodology of an umbrella review, data were extracted from secondary, rather than primary, literature. As such, there was limited evaluation of the primary studies examined by the included reviews. There was significant heterogenicity of the populations, interventions and outcomes of interest in the included studies. This limits the degree to which this review can draw conclusions regarding the impact of the integration of NDPs into PHC settings and patient outcomes. Due to the nature of an umbrella review, only systematic reviews and meta-analyses were included. As such, other publications that may offer useful insights were not included.
Implications
The aggregated results from the included reviews suggest that the integration of an NDP in PHC settings can improve patient outcomes and quality of care. Biomedical markers, such as HbA1c, blood pressure and cholesterol, improved with pharmacist intervention across a number of trials. Pharmacist intervention also improved quality use of medications and reduced inappropriate prescribing. There was no effect on quality of life. Greater integration of pharmacists into the healthcare team, with access to medical records and administrative services, as well as shared goals and responsibilities, may improve patient outcomes.
Research in this area is heterogenous, and therefore, it is difficult to draw strong conclusions. Standardisation of populations, interventions and/or outcomes could improve the quality of research and allow for better applicability and generalisability. In particular, strategies that encourage better pharmacist integration into PHC teams to deliver multifaceted interventions need further investigation.18 The potential for pharmacists and community pharmacy to influence patient chronic disease outcomes can be constrained by a lack of pharmacist time (in lieu of dispensing medications), limited integration and interprofessional collaboration with clinicians to increase patient continuity of care (eg lack of access to medical records and respectful partnerships) and suboptimal timing to influence patient outcomes.8 A further evaluation of programs with integrated pharmacists within general practices and other PHC services, especially for subpopulations that tend to be underserved in regard to medication management, may help inform optimal models of care for intervention and for financing.19 A clearer understanding of ways to reduce barriers to pharmacist integration might better harness their pharmaceutical skills in PHC settings.
Conclusion
PHC services in Australia, comprising a range of healthcare providers, are faced with the challenge of addressing increasingly complex and chronic disease. When integrated into primary practice, NDPs provide a range of clinical services within a team-based model of care that can improve patient outcomes and quality use of medications. Overall, the results of the included systematic reviews and meta-analyses suggest that the integration of an NDP has a positive effect on patient outcomes.