This article is the second in a commissioned series on paediatric orthopaedics.
Rotational malalignment of the lower extremity in the growing child is a common cause of concern for parents and can be a potential cause of hip, knee and ankle pain.
Torsional deformity is usually first noticed by parents or carers of toddlers as in-toeing or out-toeing. Most rotational variants fall within the range of normal childhood rotational development and require no treatment.1 It is generally accepted that rotational changes plateau after the age of 8–10 years, but there remains much debate about the threshold whereby normal transitions into malalignment.1–3
It is important to recognise that while most rotational deformities correct at skeletal maturity with normalisation of the foot progression angle (FPA), the compensatory rotation may occur in the hip, knee or foot.2,3 Insufficient compensation in any of the lower limb segments may result in mechanically disadvantaged lever arms, potentially causing overuse pathology or a predisposition to injury.4 Pathological rotational abnormality can cause difficulty with gait and has been implicated in hip abductor pathology, femoral acetabular impingement (FAI), patellofemoral joint (PFJ) instability or pain, ankle instability, midfoot pain as well as early-onset arthritis.4–6
Natural history
‘Knowledge of what is possible is the beginning of happiness.’
– George Santayana7
Limb development begins in the fifth week in utero with the appearance of limb buds. Progressive intrauterine molding then causes external rotation at the hip, internal rotation of the tibia and variable posturing of the foot.1,4,8 At birth, the mean femoral anteversion is approximately 40°, but this is masked by the relative external contracture at the hips. Postnatally, the lower limbs continue to de-rotate in children who are developmentally normal, with the tibia externally rotating 15–20° and the femur externally rotating 25° by the age of 8–10 years. At skeletal maturity, adolescents normally walk with approximately 5–10° of external FPA, comprised of roughly 15° femoral anteversion and an average of 23° external tibial torsion (ETT).3,9,10
Rotational problems are more frequent in patients with neuromuscular disease. These problems worsen with age. This is due to a variety of causes including muscle imbalance, contractures and a lack of weight bearing. Pathological rotational abnormalities in this cohort do not self-resolve; if required, osteotomies are the most reliable method of correction.11,12
Clinical assessment
A thorough evaluation of rotational problems requires a detailed clinical and functional history as well as a targeted examination to differentiate normal variability from structural pathology.
Step one: History-taking
History-taking should ascertain the reason for the review, such as parental concern about abnormal gait, and define the nature of any pain or functional deficit. It should also assess any intrapartal issues and record any concerns about developmental milestones.
It is important to ascertain any familial history of hereditary disorders with musculoskeletal involvement, including skeletal dysplasias, developmental dysplasia of the hip (DDH) or the hereditary motor sensory neuropathies (HMSN).
Patient-reported outcomes to measure health-related quality of life have recently been introduced to allow for more sophisticated assessments of a patient’s functional deficits due to rotational axis pathology.5 Measures such as the 36-Item Short Form Health Survey (SF-36) explore the mental component of health as well as the physical aspects of disease to aid in shared decision making.
Step two: Examination of gait
Toddlers do not walk in the same way as adults; children settle into a mature gait by the age of four years. Until then, their gait is immature, with a wide-based gait, hyperflexed hips and knees, abducted shoulders, extended elbows and relative internal FPA (Figure 1).1,2 It is important to document this for monitoring purposes.
Toddlers begin walking with relative internal rotation and externally rotate to an FPA of 10° external rotation by the age of eight years, with little change into adulthood.13,14
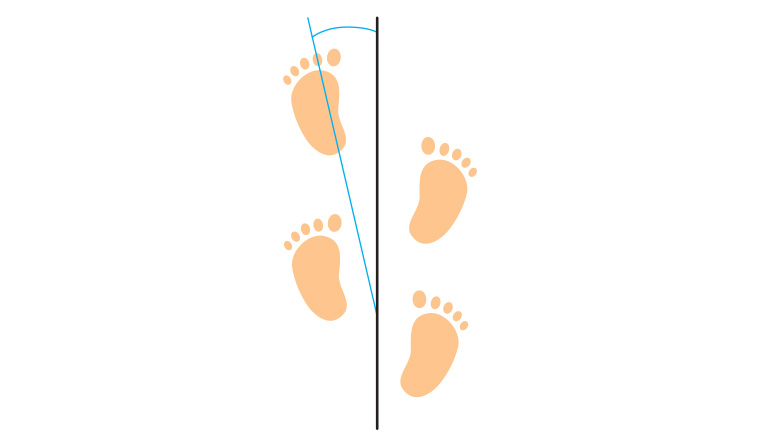
Figure 1. The foot progression angle is the angular difference between the axis of the foot and the line of progression (an imaginary line along which the patient walks). It represents the sum of femoral torsion, tibial rotation and foot shape, and is influenced by muscular forces and weightbearing.8
Step three: Determining rotational profile
After observational gait analysis, visualisation of the patient’s coronal and sagittal alignment can reveal limb asymmetry or an underlying syndromic condition.
Hip rotation is best examined with the patient prone, hip extended and knee flexed to 90°; the tibia and examination couch are useful reference points. Increased hip internal rotation is indicative of femoral anteversion, while the opposite may be representative of femoral acetabular, retroversion and impingement (Figure 2).13–16
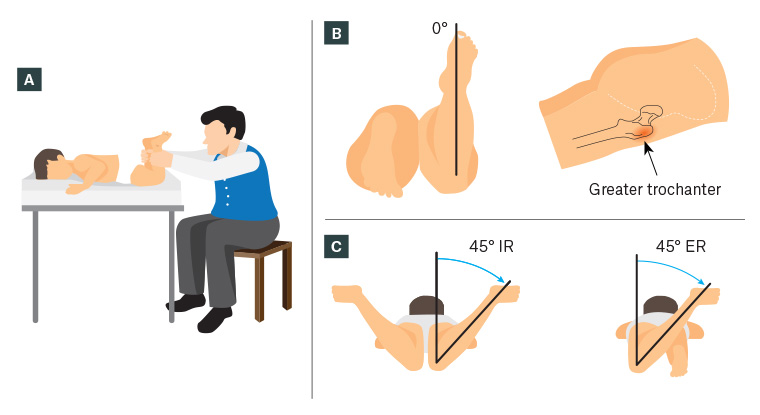
Figure 2. Prone examination of hip rotation
A. Author’s preferred method of measuring hip rotation; B. Measuring anteversion using the trochanteric prominence angle test (Craig’s test); C. Hip internal rotation (IR) and external rotation (ER)
The transmalleolar axis represents tibial rotation in relation to the longitudinal axis of the thigh; the thigh–foot axis is an amalgamation of this measure with hindfoot rotation. A deformity through the ankle joint or in the foot can alter the interpretation of the thigh–foot axis (Figure 3).11–14,17
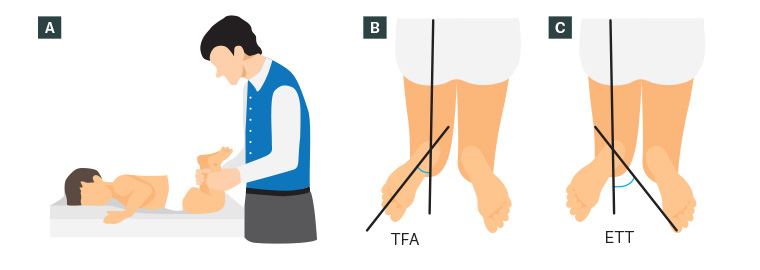
Figure 3. Measurement of tibial torsion
A. Author’s preferred method of measuring tibial torsion; B. Assessing thigh–foot angle (TFA); C. Measuring external tibial torsion (ETT) using the transmalleolar angle
Examination of rotational deformity in the foot segment uses the heel bisector line, which is drawn through the midline axis on the plantar aspect of the foot.18–20 A thorough rotational profile assessment with a sound grasp of expected normal values for each segment allows for early recognition and diagnosis of rotational abnormalities in the growing child.
Step four: Indications for referral
Some red flags to trigger a referral to paediatric orthopaedic surgery include asymmetrical deformity, rotational values that exceed normal limits for age (Tables 1, 2 and 3), recurrent tripping in a school-aged child that affects activity participation, and rigid or progressive deformities.
| Table 1. Mean femoral anteversion over time grouped by sex25 |
| Age (years) |
Mean femoral
anteversion (female) |
Standard deviation |
Mean femoral anteversion (male) |
Standard deviation |
| 3 |
40° |
19.6 |
27° |
19.1 |
| 4 |
38° |
23.9 |
30° |
18.3 |
| 5 |
37° |
20.6 |
21° |
17.9 |
| 6 |
31° |
21.4 |
23° |
20.0 |
| 7 |
31° |
23.3 |
16° |
15.1 |
| 8 |
27° |
19.9 |
12° |
13.9 |
| 9 |
18° |
18.0 |
13° |
17.7 |
| 10 |
17° |
17.8 |
10° |
13.3 |
| Table 2. Mean tibial torsion for both sexes over time25 |
| Age (years) |
Mean external tibial torsion |
Standard deviation |
| 3 |
34° |
6.4 |
| 4 |
35° |
6.2 |
| 5 |
35° |
5.8 |
| 6 |
33° |
6.2 |
| 7 |
34° |
6.9 |
| 8 |
35° |
6.3 |
| 9 |
36° |
4.9 |
| 10 |
36° |
4.9 |
| Table 3. Mean thigh–foot angle for both sexes over time1 |
| Age (years) |
Mean thigh–foot angle |
Standard deviation |
| 3 |
5° |
12.6 |
| 4 |
8° |
11.3 |
| 5 |
9° |
9.3 |
| 6 |
10° |
11.6 |
| 7 |
12° |
7.3 |
| 8 |
14° |
7.3 |
| 9 |
16° |
5 |
| 10 |
18° |
7.6 |
Management of individual segments
Femur
Femoral anteversion describes the inward rotation of the femoral neck that results in medial torsion of the femur during gait. There is a huge variation in anteversion: the average at birth is 40°, with reduction as a child matures to approximately 14–18° as an adult.16 Females generally have more femoral anteversion than males. Although it is most commonly idiopathic, it can be associated with conditions that cause abnormal muscle forces on a growing skeleton such as DDH, cerebral palsy or HMSN.
Idiopathic femoral anteversion does not predispose individuals to functional deficits or increase their risk of osteoarthritis of the hip.6 The most common presentations are in-toeing when the child walks (internal FPA), tripping or falling often and sitting in a ‘W’ shape with their knees bent and legs splayed behind.14 This often resolves as the child grows towards adulthood, and reassurance and observation is often the only treatment required. Surgical intervention is generally not considered prior to the child reaching 9–10 years of age to ensure that treatment is based on the rotational profile at skeletal maturity.
In adolescence, complaints of groin and thigh pain may be due to hip instability, gluteal fatigue or FAI, all of which are caused by the unfavourable hip lever arm due to increased femoral anteversion. A cause for an urgent referral to an orthopaedic unit would be concern for slipped capital femoral epiphysis, which can be diagnosed with plain radiographs consisting of anteroposterior pelvis and frog leg views. Anterior knee pain in this cohort can be attributed to miserable malalignment syndrome, PFJ pain and instability due to a combination of increased femoral anteversion and excessive external tibial torsion.11 In severe cases, surgical correction requires osteotomies with soft tissue surgery to augment the repositioned lever arms.
Tibia
There is a mild degree of physiologic out-toeing during normal gait at skeletal maturity. This external FPA is due to the normal ETT. The most common presentation of a rotational deformity involving the tibia is excessive internal tibial rotation and may either be congenital or developmental.1,3,8,13 The majority of patients have bilateral limb involvement, and it is imperative to determine if the abnormal torsion is purely a rotational problem or if it is combined with an angular deformity.14
While most torsional deformities may not affect a child’s function, abnormal tibial torsion may exacerbate foot deformities. For example, internal tibial torsion in a child with residual clubfoot may cause them to trip excessively. Excessive ETT in a child with cerebral palsy exacerbates the proximal femoral anteversion deformity.12
Foot and ankle
Metatarsus adductus (MTA), medial deviation of the metatarsals at the tarsometatarsal joint, is a clinical diagnosis in an infant. The lateral foot border is convex instead of straight, and a medial foot crease is present when there is a more rigid component. It is important to distinguish this diagnosis from a clubfoot or, in rarer situations, a skewfoot.18
Imaging prior to four years of age is rarely indicated because there is insufficient ossification and most cases of flexible MTA resolve spontaneously.14 Infants with rigid MTA may require serial manipulation with casting prior to walking age.19 In severe cases, surgical intervention may be required20 to achieve a balanced, shoeable foot.
Pes planovalgus, commonly termed a flat foot, is combination of three components: the valgus hindfoot, flattening of the medial longitudinal arch and abduction of the forefoot.21 Asymptomatic flexible planovalgus feet are common in toddlers and often resolve spontaneously as the plantar fascia and spring ligament stiffen with improved tibialis posterior activation in adolescence. The deformity can remain in hypermobile or obese children; persistent pes planovalgus must be differentiated into flexible or rigid deformities.
A symptomatic, rigid planovalgus foot always needs investigation, as this is pathological. Causes can include tarsal coalition, congenital vertical talus and congenital tendoachilles contracture. Treatment begins with non-surgical options such as insertable orthoses, which can alleviate pain by improving the foot lever arm but will not physically alter a flat foot.22,23 Surgical options are available depending on the pathology.24
Conclusion
Abnormalities in the lower limb rotational profile of children can be of great concern to parents and carers. In most cases, the complaint is a normal variant of growth and development, and the problem resolves without treatment as the child grows. A focused history and targeted clinical examination, together with an understanding of what is normal, will determine whether a complaint requires further evaluation.