Case
A man aged 23 years presented to a new general practitioner requesting treatment for his gout. He had been living in Australia for four years after emigrating from Bangladesh. He described a one-year history of gout in his right knee and left ankle, diagnosed after a high serum uric acid level. The only other medical history reported was asthma and allergic rhinitis. He had experienced constant pain with minimal improvement despite a six-month course of febuxostat and courses of prednisolone and nonsteroidal anti-inflammatory drugs (NSAIDs). A cortisone injection into his knee one month prior was somewhat helpful; however, his ankle pain persisted. On examination, he had a moderately swollen left ankle, with mild tenderness laterally but no overlying erythema. The ankle was warm but not hot, with slightly limited range of movement due to the swelling.
Question 1
What are the red flags in this history that raise suspicion for another diagnosis?
Answer 1
The red flags in this history that raise suspicion for another diagnosis are:
- It is a chronic oligoarthritis. Gout presents as an acute monoarthritis that usually only lasts for up to 1–2 weeks, even if untreated.1
- There has been no aspirate identifying urate crystals in the joint.
- Large joints are involved. This is atypical because gout usually starts in small joints.
- Two joints are involved at the same time. In gout this happens later, in the stages of inter-critical gout or chronic tophaceous gout.
- It has not improved with therapy (ie NSAIDs).
- The patient is a young man and from a country with higher rates of infectious diseases.
Question 2
On clinical suspicion of gout, which investigations should be performed?
Answer 2
A definitive diagnosis of gout requires confirmation of monosodium crystals under polarised microscopy, by aspiration of an affected joint, bursa or tophus. This is important to exclude infection and also because gout frequently requires lifelong urate-lowering therapy. Serum uric acid concentration should be checked; however, this may be normal in patients with acute gout, and hyperuricaemia alone is not diagnostic of gout. Assessment of renal function is required, as impaired renal function is both a risk factor for and a possible complication of gout. A plain X-ray to assess for joint damage and investigation for a secondary cause of gout should be considered.2
Case continued
A full blood examination, inflammatory markers and biochemistry, ankle X-ray and ultrasonography with joint aspiration were arranged. The results are shown in Table 1.
| Table 1. Initial investigation results |
| Blood tests |
Result |
| Full blood examination |
Within normal limits |
| Inflammatory markers |
C-reactive protein: 41 mg/L (reference range 0–5 mg/L) |
| Erythrocyte sedimentation rate: 23 mm/h (reference range 1–20 mm/h) |
Biochemistry
|
Creatinine: 70 μmol/L (reference range 60–110 μmol/L) |
| Estimated glomerular filtration rate: >90 mL/min (reference range >59 mL/min) |
| Uric acid: 0.33 mmol/L (reference range 0.20–0.50 mmol/L) |
| Calcium: 2.38 mmol/L (reference range 2.15–2.55 mmol/L) |
| Corrected calcium: 2.30 mmol/L (reference range 2.15–2.55 mmol/L) |
| Gamma-glutamyl transferase: 66 U/L (reference range 5–50 U/L) |
| Other results within normal limits |
| Imaging |
| X-ray and ultrasonography of left ankle |
The radiographs show no fracture or focal lesion.
No erosive disease is present, but there is prominent soft tissue oedema medially. Sonographically this corresponds to complex synovial fluid extending from the joint and around the tendons. There is associated hyperaemia. Gout seems likely.
The superficial fluid was aspirated. Informed consent was obtained following discussion of the risks and benefits. Chlorhexidine skin preparation. Under ultrasound guidance, a 22 G needle was used to sample the fluid and material has been provided to the pathology service. |
| Microscopy and culture |
| Joint aspiration from left ankle |
Crystals not detected.
Leucocytes: +++
No organisms seen.
No growth aerobically or anaerobically after seven days’ incubation.
Radiology comment: After a negative aspirate in a patient suspicious for gout, there is likely to be a role for dual energy computed tomography … to assess for spectral evidence of monosodium urate deposition. |
Question 3
What are other possible causes of a chronic inflammatory oligoarthritis?
Answer 3
Other possible causes of a chronic inflammatory oligoarthritis include:
- reactive arthritis
- atypical-onset rheumatoid arthritis
- juvenile idiopathic arthritis
- oligoarticular psoriatic arthritis
- HLA-B27-associated arthritis
- septic arthritis (eg chronic bacterial, fungal or mycobacterial).
Case continued
Five days later, the patient’s ankle pain was worse, associated with purulent discharge from the aspiration site and night sweats. He was referred immediately to the emergency department. In hospital, a magnetic resonance imaging scan showed a large, infected collection directly extending into the calcaneus. A whole-body bone scan identified an additional right patella focus. The patient underwent washout and debridement of the calcaneal abscess and the right patella and pre-patella bursa, with samples sent for microscopy, culture and sensitivity, acid-fast bacilli (AFB) culture, fungal culture, crystals and rapid polymerase chain reaction (PCR) testing. A computed tomography scan of the chest found a moderate right pleural effusion, which the patient recalled had been found on a chest X-ray previously. AFB culture and rapid PCR testing on a sample taken from the left calcaneal abscess were positive for tuberculosis, and he was therefore diagnosed with disseminated tuberculosis.
Question 4
What are the risk factors for tuberculosis infection?
Answer 4
The risk factors for tuberculosis infection include:
- travel to or emigration from an area with a high incidence of tuberculosis, especially healthcare workers
- tuberculosis exposure, especially contacts of an active case within the past five years
- living in over-crowded conditions (eg institutions, some Aboriginal and Torres Strait Islander communities)
- human immunodeficiency virus infection
- history of a positive purified protein derivative skin test or interferon-gamma release assay result
- history of prior tuberculosis treatment.3,4
The countries accounting for the majority of tuberculosis cases are shown in Figure 1.
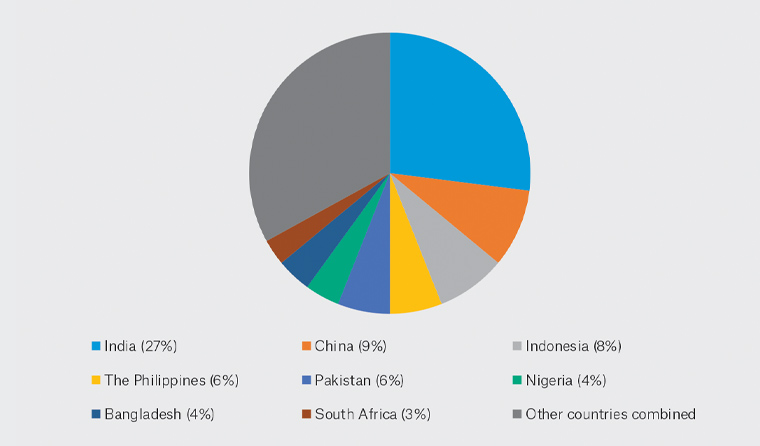
Figure 1. The eight countries that account for two-thirds of the total number of tuberculosis cases worldwide5
Question 5
What are the clinical features with which tuberculosis may present?
Answer 5
In Australia, over 50% of cases will present with pulmonary symptoms;3 however, there is also a wide range of non-pulmonary symptoms to be aware of, as detailed in Table 2.
| Table 2. Possible presenting features of tuberculosis3,4,6 |
| Systemic features |
Malaise
Fatigue
Night sweats
Fever (can be intermittent)
Anorexia
Weight loss |
| Pulmonary tuberculosis |
Chronic cough
Haemoptysis |
| Tuberculous meningitis |
Headache
Mental state changes +/– coma
+/– Fever |
Skeletal tuberculosis
|
Spondylitis: Back or neck pain +/– stiffness, +/– lower limb paralysis
Arthritis, most commonly of the hips, knees, ankles, elbows, wrists and shoulders
Osteomyelitis
Note: Radiographic changes may lag for weeks to months behind the onset of pain |
| Genitourinary symptoms |
Both men and women:
Flank pain
Dysuria
Frequent urination
Men:
Painful scrotal mass
Prostatitis
Orchitis
Epididymitis
Women:
Can mimic pelvic inflammatory disease |
| Gastrointestinal symptoms |
Non-healing mouth or anal ulcers
Difficulty swallowing
Abdominal pain
Malabsorption
Diarrhoea
Haematochezia |
| Ocular symptoms |
Blurred vision
Photosensitivity
Flashes
Floaters
Eye redness |
| Elderly patients |
May not present with typical tuberculosis symptoms and may instead present with a non-resolving pneumonitis |
| Blood test features |
Leukocytosis
Anaemia
Hyponatraemia |
Question 6
On suspicion of tuberculosis, which investigations would you order to confirm the diagnosis?
Answer 6
The diagnosis of extrapulmonary tuberculosis requires investigations and sampling directed at the affected organ system. Radiologists and microbiology laboratory staff should be notified that tuberculosis is being considered. A chest X-ray and sputum microscopy (with acid-fast stain), culture and sensitivity should be arranged for patients suspected of having either pulmonary or extra-pulmonary tuberculosis.2 The diagnosis of pulmonary tuberculosis, even when there is low clinical suspicion, is important not only for the patient but also for public health safety in regard to the transmissibility of infection.
Key points
- Confirmation of the diagnosis of gout is important, particularly in a patient with atypical features for gout, to exclude other potentially serious causes and also because gout requires lifelong treatment.
- Certain factors increase a patient’s risk for having tuberculosis, and it is especially important to consider tuberculosis in patients with these risk factors.
- Tuberculosis can present with a range of pulmonary and extra-pulmonary symptoms.