General practitioners (GPs) and general practice registrars initiate 51% of Australia’s opioid medications; half of these are prescriptions for chronic non-cancer pain.1,2 Thirty per cent of patients with chronic non-cancer pain are prescribed opioids, and more frequently strong opioids rather than weak.3 In Australian general practice, where 85.8% of consultations are funded by the Australian Government with no out-of-pocket cost to patients, the cost of chronic pain management is heavily shouldered by the public health system through Medicare.4
Medical, legal and disciplinary bodies have highlighted iatrogenic harms caused by escalating GP opioid prescribing.5,6 To address this issue, state and national Departments of Health, The Royal Australian College of General Practitioners (RACGP) and various stakeholders have developed interventions to reduce harms from prescription opioids (Table 1). These include up-scheduling codeine from over-the-counter to prescription-only, educational initiatives, real-time prescription monitoring (RTPM) programs and high-prescriber nudge letters that notify individuals of their outlier prescriber behaviours. These letters, typically sent to a proportion of prescribers with the highest prescribing rates, seek to ‘nudge’ practices from outlier to average. Several of these interventions have been implemented internationally, with varying effects on prescribing patterns and patient outcomes – although generally not resulting in significant improvements to guideline-concordant prescribing.7
| Table 1. Summary of federal initiatives targeting prescribers to improve opioid prescribing |
| Initiative/intervention |
Key points |
| Real-time prescription monitoring (RTPM) programs26,27,34,35,37–39 |
National system
- In February 2012, the Australian Government pledged $5 million for a national RTPM program, which did not eventuate. In May 2018, a subsequent Australian Government pledged $16 million for a national RTPM program
- Introduced as the National Data Exchange in December 2018 using the Electronic Recording and Reporting of Controlled Drugs (ERRCD) system
- The ERRCD is an updated version of the Tasmanian Drug and Poisons Information System Online Remote Access (DORA)
- Will require integration with state-based systems and jurisdictions
- States still allowed to continue with their state-based programs as long as they are compatible with the national system
Tasmania
- First introduced in 2009 for Department of Health policymakers/regulators
- Access to clinicians granted in 2011
- Currently optional use for prescribers and mandatory use for dispensers of Schedule 4 opioids and Schedule 8 medications
- DORA system
Victoria
- First introduced July 2018 for general practitioners (GPs), community pharmacists, prescribers and pharmacists in hospital emergency departments
- Currently mandatory use for prescribers and dispensers
- SafeScript system
Australian Capital Territory
- First introduced March 2019 for GPs, community pharmacists, prescribers and pharmacists in hospital emergency departments and outpatient clinics across the Australian Capital Territory
- Optional use for prescribers and dispensers
- Provides weekly reporting of Schedule 8 medications (not real-time)
- DORA system
New South Wales
- Proposed $30 million for state-based RTPM in 2020–2021 budget
- Currently has ERRCD system (monthly reporting) in place with capability to enable RTPM
Western Australia
- Currently has a telephone information service that collects information on all dispensing data of Schedule 8 medications from community pharmacies
- Intention to launch a modified version of ERRCD in late 2020 (pending)
- Will be available to GPs, community pharmacists, prescribers and pharmacists in hospital emergency departments and outpatient clinics across Western Australia
Northern Territory
- Potentially waiting for national system for RTPM
- Currently has weekly reporting of Schedule 8 medications through the Northern Territory Drug Monitoring System
South Australia
- Introduced ScriptCheckSA as a state-based RTPM in 2020
- Planned as a mandatory system following a 12-month period of voluntary use for prescribers and dispensers
Queensland
- Proposed state-based system called Q-Script in 2019
- Delay in implementation
- Currently has monthly reporting of Schedule 8 medications available to dispensers only
|
Up-scheduling of codeine29
|
- Implemented 1 February 2018
- No codeine-containing medications available over the counter in Australia
- Therapeutic Goods Administration up-scheduled codeine (in all doses) to a Schedule 4 medication (prescription only)
|
Medicare high-prescriber notifications36
|
- 2018–2019 campaign
- Top 20% of GPs who had highest rates of opioid prescribing sent notification letters (signed by Australia’s Chief Medical Officer on behalf of the Department of Health)
- 3400 urban GPs notified
- 1400 regional and remote GPs notified
- Followed similar campaign of high antibiotic prescribing notifications in 2017
|
| National Prescribing Service (NPS) MedicineWise |
- Opioid prescribing education and training programs delivered to GPs in 2015 and 2019
- Sessions about various aspects of chronic pain and current evidence-based recommendations
- Recent program introduced in October 2019, ‘Opioids and the bigger picture when treating chronic pain’ educational visit available as one-to-one sessions with GPs or small-group practice meetings
- Available at www.nps.org.au/professionals/opioids-chronic-pain
- Prescriber peer group norm comparisons provided in personalised NPS feedback letters in late 2019
|
| The Royal Australian College of General Practitioners’ opioid prescribing guidelines |
- Published online in 2017
- Prescribing drugs of dependence in general practice is currently Australia’s main evidence-based GP opioid prescribing guidelines
- Part A: Clinical governance framework
- Part B: Benzodiazepines
- Part C1: Opioids
- Part C2: The role of opioids in pain management
- Available at www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/drugs-of-dependence
|
Conceptualising GP attitudes towards these interventions using an established model of behaviour change may help improve prescribing. The Capability–Opportunity–Motivation model of behaviour change (COM-B model) provides a comprehensive taxonomy of behaviour change functions, and postulates that interactions between these three primary components facilitate behaviour change (Figure 1).8 Capability, referring to both physical and psychological capability, also refers to guideline use, environmental restructuring and modelling. Social and physical opportunity are closely tied to capacity; opportunity for change requires capacity but may, in turn, demand it. Finally, reflective processes (such as planning) and autonomic (emotional) processes drive motivation to change. The COM-B model has been used frequently as a framework to explore the drivers of clinician behaviour change in a range of contexts, including prescribing behaviour change.9–11 Australian systems-level initiatives aimed to reduce overprescribing of opioids target all three domains of the COM-B model, including capability (education, guideline use and RTPM), opportunity (up-scheduling codeine) and motivation (high-prescriber nudge letters), as presented in this article.
The aim of this study was to explore GP knowledge and attitudes towards Australian system-level opioid-prescribing interventions using the COM-B model.
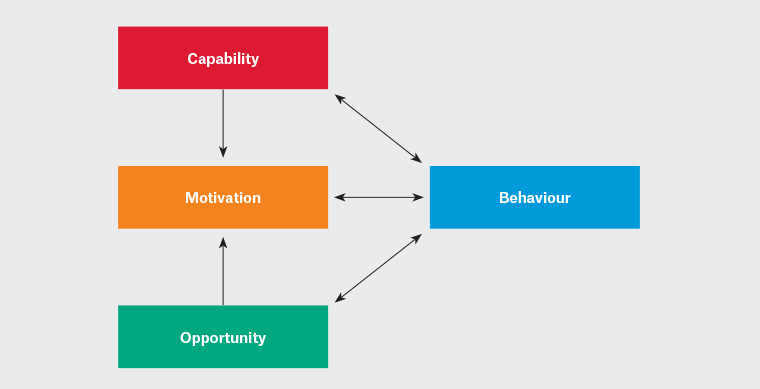
Figure 1. The Capability–Opportunity–Motivation model: a framework for understanding behaviour
Reproduced from ‘The behaviour change wheel: A new method for characterising and designing behaviour change interventions’8
Methods
Study design
This study used a qualitative approach best suited to an in-depth exploration of relationships between knowledge, attitudes and behaviours. A secondary analysis of previously collected data was used to answer a new research question: What are GP attitudes towards system-level opioid prescribing interventions and what are the implications of them for future behaviour change interventions? These were reported in accordance with the COREQ checklist.12,13 The primary qualitative studies of 2018 and 2019, undertaken by the same authors, involved 30–60-minute interviews with GPs and general practice registrars based in Victoria and New South Wales (NSW) and explored GP opioid prescribing practices more generally.
Low-risk ethics approval was granted for the Victorian and NSW studies by Monash University (approval number 12504) and University of Technology Sydney (approval number ETH18-2399), respectively. All participants gave written informed consent to participate.
Participants
Victorian participants were eligible if they were professionally registered GPs or registrars with no active or previous restrictions in opioid prescribing. Registrars were enrolled in Australian GP training programs. NSW participants were eligible if they self-reported practising as a GP, and had experience in prescribing opioids for cancer pain.
Recruitment
Victorian GPs with RACGP or Australian College of Rural and Remote Medicine Fellowship were recruited from 600 invitations using the Monash Practice-Based Research Network. Registrars were recruited from invitations on closed general practice registrar Facebook groups and email lists. Gift cards to the value of $100 (GPs) and $50 (registrars) were offered. Interviews were undertaken between April 2018 and February 2019; the Victorian state RTPM called SafeScript was introduced in July 2018.
NSW GPs were recruited via email listservs, GP conferences/forums, and groups concerned with pain and/or cancer (eg the Translational Cancer Research Centres NSW). GP practices were directly recruited (telephone and email), after selection using a quasi-randomised approach using Google Maps, and stratified according to Australian Bureau of Statistics remoteness structure for purposeful sampling.14 Participants were reimbursed in accordance with Australian Government funding for a 20–40-minute consultation ($71.70). RTPM did not exist in NSW at the time of this study, although it had been proposed.
Research team and reflexivity
Victorian interviews were undertaken by PP, a practising GP and PhD candidate. CB (Senior Lecturer) and DM (practising GP and Professor of General Practice) guided the research. NSW interviews were undertaken by TL, a social scientist and academic, aided by a palliative care nurse working as a research assistant. Participants were aware of the interviewers’ credentials.
Data collection
Ten to 20 semi-structured open-ended questions were used to explore personal experiences. This article focuses only on participant attitudes towards systems-level initiatives; findings of the primary aims have been reported separately.13,15 Self-reported responses were not corroborated with quantitative measurements. No interviews were repeated.
Data collection in Victoria was guided by the four-phase Interview Protocol Refinement; the NSW study used a framework for prescription-related decision-making by Raisch.16,17 Five further Victorian GP interviews, nine Victorian registrar interviews and five NSW GP interviews were undertaken after data saturation to confirm diversity and consensus in views.
Interviews were audio-recorded and professionally transcribed. Victorian participants reviewed their unedited transcripts and amendments were agreed upon before coding. No verification was conducted for the NSW sample. Reflective journals were kept throughout.
Data analysis
Braun and Clarke’s six-phase theoretical framework was adopted for thematic analysis, guided by the COM-B model.8,18 Data were managed using QSR N-Vivo software. Practices to ensure rigour in the secondary analysis process were guided by Ruggiano.12
Initial codes were generated by PP and TL from review and independent line-by-line coding of 10 transcripts. Data were discussed and reviewed, transcripts recoded using an agreed revised coding scheme, and refined into themes. Guba and Lincoln’s criteria of trustworthiness, transferability, confirmability and dependability were used to ensure quality of data and coding.19
Results
Participant characteristics
The Victorian sample included 20 GPs (10 men and 10 women) and 20 GP registrars (eight men and 12 women). Registrar ages ranged from 26 to 41 years. Three were outer regional trainees and 17 were metropolitan. All GPs practised in metropolitan Melbourne. Ten participants were over 10 years post-Fellowship, four were 5–10 years post-Fellowship, and six received their Fellowship less than five years ago.
The NSW sample included 17 GPs (eight men and nine women). Ages ranged from 32 to 70 years. Nine participants practised in metropolitan Sydney, six in inner regional and two in outer regional areas. Five participants had practised for more than 30 years, three for 21–30 years, three for 11–20 years, two for 5–10 years, and two for less than five years.
Table 2 provides exemplar quotes from participants coded against each component of the COM-B model. Those that seem most important for future systems-level behaviour change interventions are discussed in greater detail in the remainder of this article.
Click to view Table 2
Capability domain of the COM-B model
Education and training
The study found 33 of 40 Victorian participants were unaware of the RACGP Prescribing drugs of dependence in general practice guidelines. Many participants felt interventions designed to improve knowledge, including guidelines and academic detailing, were targeted at unsafe or ignorant doctors – not themselves. They believed their own knowledge was satisfactory, and as a result these initiatives were rarely used. Older GPs felt the RACGP guidelines were more useful for junior doctors.
It’s nice to have thorough documents that cover everything in detail but that’s more appropriate for someone in hospital or GP training. When it’s somebody out in practice, you need something that is more focused to whatever their need is. (GP 20 Victoria)
Key barriers therefore related to beliefs about capability and reflective motivation.
RTPM programs and Prescription Shopping Information Service
Victorian participants felt RTPM programs provided useful clinical information and generally had positive beliefs about the consequences of this intervention. Many participants interviewed after July 2018 had used SafeScript (after it was introduced but before it was mandated). NSW participants did not have experience using RTPM but still felt positively towards the concept. Prescribers believed these initiatives helped identify drug-seeking behaviours and increased GP confidence in declining to prescribe: ‘If you tell them you’re going to phone the doctor shopping line, often they just walk out’ (GP 18 Victoria). These initiatives also provided perceived sanction to prescribe opioids for patients unfamiliar to the GP and not flagged on these systems. Participants felt this helped new patients to access opioids if they thought it was indicated.
However, participants felt the threshold for identification by the Prescription Shopping Information Service was too high and therefore unsafe or unreliable. Participants hoped this service would be superseded by more reliable RTPM. Despite the environmental context (ie mandated use), some Victorian participants believed RTPM was still not fail-proof.
SafeScript is a very, very good idea. But again, SafeScript would only be a guide. It would not actually stop these doctors from prescribing, but it will flag them. Maybe that will stop them from [prescribing]. (Registrar 7 Victoria)
Opportunity domain of the COM-B model
Codeine up-scheduling
Despite some initial concerns, neither NSW nor Victorian participants reported substantial increases in codeine requests or drug-seeking behaviours. Although this intervention was generally positively perceived, reservations related to motivation and social opportunity. Three participants believed that up-scheduling was just a money-making exercise by the government, that codeine overuse/misuse was not really a problem to start with, and that addressing codeine alone would not help.
Sometimes it’s hard to see the big picture, to seek out a bird’s eye view of the overall global effect when you’re just focused on one particular drug – as is the case with codeine. (GP 11 NSW)
A small number of GPs were concerned about under-treatment for patients who previously self-managed pain with over-the-counter codeine. Participants felt these people might be hesitant requesting codeine from GPs, and therefore at risk of untreated pain.
It’s a big hassle for people to come in for a [codeine] script. People get annoyed having to come in and pay for their doctor to give them a script to then [pay for] the medication. So, it’s been a bit of a double-edged sword. (Registrar 10 Victoria)
Motivation domain of the COM-B model
High-prescriber notifications
Participants in both states were equally confronted by the 2018 Australian Government Medicare high-prescriber nudge letters. Much of the justification of negative attitudes towards this initiative stemmed from automatic and reflective motivation, particularly emotional responses. One participant explained:
I recently received a letter telling me I was 99% higher prescriber than my peers. That got me very upset until I phoned my [medical indemnity organisation] and was met with a laugh and told many of my peers had got the same letter, so I think the guidelines are actually out of touch. (GP 12 Victoria)
Other participants who had received the letters believed their opioid prescribing was safe, and explained they had many patients who were elderly, had cancer pain or required palliative care. Participants felt they had been unfairly targeted, and that true outlier prescribing was demonstrated by GPs who had younger patient populations, less chronic disease or did not provide palliative care to justify their comparable higher opioid prescribing rates.
Many participants perceived the nudge letters to be overly paternalistic and persecutory in ethos, particularly as the letters had been signed by Australia’s Chief Medical Officer. A small number of participants expressed a belief that the Australian Government developed this intervention to transfer responsibility from the system to the individual.
What really gets me – the governments [think] they can solve the problem for the cost of sending a letter to several thousand GPs, and they’ve done their bit in terms of caring about poor outcomes in our health world. (GP 11 NSW)
Participants referred to similar, older Medicare-driven interventions (including opioid permits and authority prescriptions requiring telephone approval from the Department of Health) that they believed were burdensome for both prescribers and patients, and threatened GP autonomy. Many participants believed they were better placed to judge the safety of opioids for individual patients than government bodies, highlighting an interaction between capability and motivation.
The perception that certain interventions were targeted at other doctors and not the participant was again observed for the nudge letters. Participants worried that colleagues who received these might be less likely to prescribe opioids in the future even when these were required, risking suboptimal patient management.
If only it could be part of a structured, thought-through, compassionate program. It worries me that you’re going to have a group of GPs that get this letter and go ‘Oh, geez, I’m going to get into trouble if I do this. I’m not going to see this person again. I’m not going to give them any treatment’. (GP 13 NSW)
Discussion
This study was the first to explore Australian GP attitudes towards systems-level interventions aiming to reduce opioid overprescribing. The researchers conceptualised these interventions using the COM-B model to show various underlying behaviour change factors contributing to engagement and use of these initiatives. This study reports generally positive attitudes towards RTPM and codeine up-scheduling. High-prescriber nudge letters sent by the government were perceived to be overly paternalistic, and potentially threatened the prescribing of adequate analgesia. Guidelines and education were considered useful in principle, but uncommonly used.
The negative attitudes expressed by GPs in this study towards nudge letters should be considered within the context of quantitative findings that these techniques can reduce overprescribing of antibiotics.20 Pain is inherently biopsychosocial and often carries an emotive component to symptom presentation and treatment goals.21 Potentially, GPs may feel unfairly targeted by opioid-prescribing nudge letters (more so than antibiotic nudge letters) because they had genuine good intentions to treat a patient’s chronic pain and reduce suffering.15,21 The present findings also highlight complex issues of stigma relating to opioid prescribing. While stigma among patients is well described, this study is among the first to highlight the discrimination felt by physicians who perceive their caseload to require higher-than-average opioid prescribing.22 Government policy decisions resulting from outlier prescriber identification may contribute to these processes of stigma.23 Participants perceived the nudge letters, specifically, to be unnecessarily persecutory, overly paternalistic and felt their prescribing autonomy was threatened.
Motivation to engage with interventions may be influenced by this perceived paternalism. The study participants perceived many of these regulatory principles in moralistic binary terms: that the government intent is ‘good’ and the prescriber is ‘bad’. Several participants also describe feeling victimised by paternalistic approaches. Again, the binary nature of ‘victim’ (GP) and ‘villain’ (perceived government paternalism) is seen. This type of thinking places both prescribers and systems (governments) in danger of failing patients and patient-centred care. The participant views echoed those of a former RACGP President, that fear of persecution may place patients who need opioids (eg for cancer pain and palliative care) at risk of inadequate analgesia.24 However, the consequences of treating pain with opioids are complicated; titrating opioid dose to chronic pain intensity creates numerous harms.25
Conversely, participants in the present study were positive about RTPM, which has also received wide support from the Australian Medical Association, the RACGP and the National Coronial Investigation Service.5,26 However, many NSW participants were confused between RTPM (which was not available in NSW) and the older Prescription Shopping Information Service. Opioid analgesia regulation varies between states and territories; consistency may improve prescriber behaviour.6,26,27 Inconsistency between states has also been reported in the USA, affecting prescribing patterns by physicians.28
Although use of SafeScript is mandatory in Victoria, it is still possible to prescribe and dispense opioids despite patient alerts. The RTPM service is essentially a screening and flagging system but does not override prescribing intent. That is, physicians must engage with SafeScript but the decision to prescribe opioids still remains within the right and responsibility of the prescriber, not the SafeScript program. Long-term follow-up of opioid-prescribing behaviours after mandating use of SafeScript should also include patient-reported outcomes, in addition to prescribing rates, and qualitative insights into prescribing behaviour change.
The present study also highlights generally positive attitudes towards mandatory codeine up-scheduling from over-the-counter to prescription-only. The results contrast with published grey literature and position statements from key stakeholders such as the Pharmacy Guild of Australia.29 An Australian survey conducted before up-scheduling identified fears among pharmacists that codeine restriction would ‘burden regular GP appointments and time’, concerns not shared by GPs in their study, nor in ours.30 The participants in the present study expressed sentiments demonstrating both social and physical opportunity as enablers to change in their prescribing of codeine as a result of this initiative.
Improvements in incentivisation (eg through professional development programs) may increase use of the RACGP guidelines; reinforcements are commonly used to improve automatic motivation in the COM-B model. A study of NSW GPs found that only 31% of GPs usually employed most opioid analgesic guideline strategies.31 The present study supports findings of a systematic review that lack of awareness is the most common potential barrier to guideline implementation by physicians.32 It was also found that participant beliefs about capability may be a limiting factor; they felt guidelines were targeted at other GPs who were less expert in opioid prescribing than themselves. In the context of opioid prescribing behaviour change, these beliefs about capacity are a barrier to reflective motivation. While this study did not formally measure opioid-related knowledge and competency, several GPs made statements suggesting their expertise was limited in this area, suggesting their perceived lack of need for guidelines and other education may have been driven by poor insight. The present research joins a substantial body of research showing that clinician attitudes can be a barrier to uptake of guidelines requiring targeted strategies to change.32 Therefore, motivational strategies are needed to persuade GPs that educational opportunities are relevant to their clinical practice.
The primary limitation of this study was methodological difficulty in undertaking secondary qualitative analysis, which is less widely used than secondary quantitative analysis. Although recruitment procedures varied between the two studies, study protocols were comparable, as was the nature of enquiry in the interviews. As discussed previously, the NSW interviews were conducted by a social scientist, while the Victorian interviewers were conduc ted by a GP academic. The multidisciplinary research team undertaking this secondary analysis agreed that the interviews and emergent themes were similar enough to pool. To improve rigour, the researchers followed recommended published protocols that emphasised reliability and validity.12,33 Further limitations relate to heterogeneity of the Victorian sample (these participants predominantly practised in south-eastern metropolitan Melbourne and had been trained through the same two GP training programs) and likely sampling bias in the NSW GP study.15
Conclusion
GPs and GP trainees in Victoria and NSW shared attitudes towards systems-level interventions designed to improve opioid prescribing. In the context of the COM-B model, motivation was found to be the domain in most need of targeting by future strategies; the results suggest that beliefs about usefulness of the initiative in clinical practice and autonomy in prescribing may be important considerations in driving compliance. Nudge techniques may be perceived to be overly paternalistic and place patients at perceived risk of inadequate analgesia. Co-designing systems-level initiatives with end-users (GPs) may influence their success in Australia and internationally.