Background
‘What is “good” posture?’ is a common question from patients and a contentious topic among health professionals that is further complicated by commercial interests. Reconciling the evidence regarding posture with a patient’s individual context is important to optimally manage presenting patients.
Discussion
This article provides a viewpoint on the mounting yet established research evidence suggesting posture deserves less focus when managing pain, and the importance of understanding when to provide specific postural advice. It argues that, in general, posture is less relevant than movement itself, and creating change in patients’ behaviour and beliefs requires understanding, physical examination, clear communication and not necessarily deeming the role of posture as irrelevant.
Posture is a contentious subject among health professionals and the wider public. It holds strong cultural, political and societal meanings, but these ingrained beliefs are often unsupported by evidence. ‘Good’ posture is generally idealised as being ‘straight’ and ‘upright’, while ‘bad’ posture is associated with slumping and stooping. Physiologically, each of these postures or movements loads tissues differently. It is often the context of the total force through particular musculoskeletal tissue (tissue loading) that is key, rather than set definitions of good and bad.
In this article, posture is defined as the position of the human body, including all appendages at any moment in time. However, often as health professionals, and a wider society, we are mainly concerned with sustained postures; that is, how we sit and how we stand.
History of postural beliefs
Posture is a cultural obsession, spanning thousands of years. Ancient Greek philosophers determined upright posture was ‘linked to the divinity and intelligence of human beings’.1 This idea persisted through history, and upright, rigid posture was widely adopted for correct military drills during the 16th century. Over the 17th and 18th centuries, ‘good’ posture came to signify health, strength and beauty. ‘Bad’ posture became an indicator of not only disability but also moral degeneration, commonly described in racial sciences in the early 20th century.2 These ideas of posture were also a pillar of the Royal Central Institute of Gymnastics in Stockholm in the early 1800s, an antecedent of modern physiotherapy.3 The postural dichotomy of ‘good’ and ‘bad’ posture causing and contributing to pain and disability became endemic in medical science and societal beliefs and is still present to this day. Korakakis et al, when surveying 544 physiotherapists in 2019, found the vast majority considered upright lordotic sitting postures as optimal,4 a view shared by lay community members when assessing ‘optimal posture’.5
Some credence can be given to this historical ideal, as severe progressive kyphosis is a hallmark of untreated spinal tuberculosis or Pott’s spine, one of the oldest diseases known to mankind and associated with significant morbidity and mortality.6 Similarly, spinal deformity resultant of other spinal infections or conditions such as skeletal dysplasia was also associated with disability and poor health prior to the advent of modern medical care and early diagnosis/intervention.7
However, in the absence of such disease, this dichotomous relationship of ‘good’ and ‘bad’ posture is not supported by the evidence. As far back as 1967, John Keeve, a professor in public health, presented work supporting his statement ‘there are no scientific facts to substantiate the benefits of this (postural) aesthetic ideal, yet a great deal of attention is devoted to “correcting faulty posture”’.8 This is also supported by more recent work. A cross-sectional study of 1108 Australian teenagers found that while forward/slumped neck postures were associated with a higher incidence of depression, they had no association with neck pain and headaches, challenging widely held beliefs about the role of posture in neck pain.9 This finding was also shown in a recent meta-analysis by Mahmoud et al, in which forward head posture was not correlated with incidence of neck pain in adolescents and older adults (aged >50 years).8 The same meta-analysis did find a weak correlation in adults (aged 18–50 years), but when studies with poor-quality assessment were eliminated, these findings were not significant.10 The same analysis also suggested that in those with neck pain, increased pain was associated with increased forward head posture in older age groups.10 This is not supported by more recent studies and again brings into question the relevance of generalised cohort studies on posture and pain.11,12
Similar evidence exists for back pain, with a recent systematic review finding no link between slumping postures and pain, as well as any other lumbar posture and pain.13 Awkward postures were also shown to have no correlation with pain.14 In fact, a recent study interviewing participants with low back pain (LBP) showed even proportions of participants described sitting upright as their best (relieving) and worst (aggravating) posture.15 This study further highlights context and individual preference as important factors for identifying appropriate posture.
Clinical applications
Clinically, context is the most important factor when considering posture in presenting patients. Consider a patient with symptomatic spinal stenosis; prolonged standing or positions of relative spinal extension often lead to worsening symptoms and disability, generally eased with positions of spinal flexion such as relaxed sitting.16 In this case, advice to maintain an upright posture is in conflict with their condition.17 Neck and head posture can influence jaw function and may be relevant in patients with temperomandibular pain.18 Thoracic and scapular posture can influence respiratory mechanics and rotator cuff function.19,20 A detailed clinical history may be important for identifying specific aggravating and easing positions. This can provide specific context relevant to the patient and will give clinicians insight into what specific postural advice to provide the presenting patient (Figure 1).
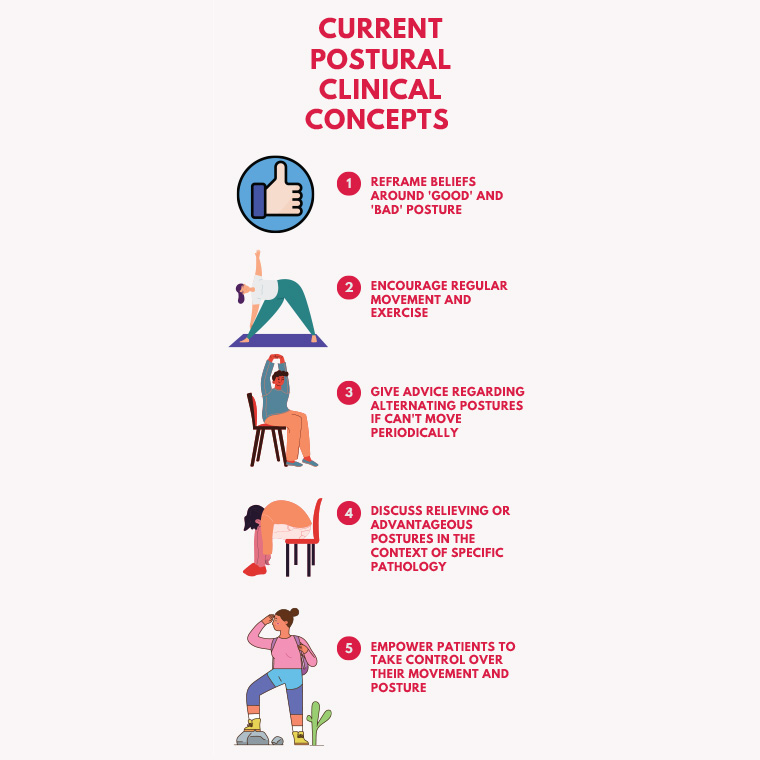
Figure 1. Tips on providing postural advice
Additionally, posture may also provide insight into a presenting patient’s psychological state. As mentioned earlier, Richards et al found that forward/slumped neck postures in teenagers are significantly associated with a higher incidence of depression.7 This may add further clinical context for in-rooms assessment – while it is definitely not a sole indicator of mental health issues, it may add further weight to clinical suspicion.
Assessment of posture is therefore not irrelevant, rather just needs to be considered in the context of the individual patient. Contextual considerations are outlined in Table 1.
| Table 1. Points to consider when developing an appropriate paradigm in which posture should be considered and addressed |
| Patient history |
- How long are postures sustained in work, home, recreational activities?
- Patient beliefs regarding posture
- Occupational demands
- Physical activity history
|
| Physical examination |
- Is posture providing insight into non-mechanical influences (psychological state, confidence)?7
- Mechanical influences that load or offload tissues
- Does altering posture during examination change pain, joint range of motion or muscle function relevant to the patient?
|
| Management |
Address beliefs:
- Correct faulty beliefs (eg that bad posture = pain)
- Explain the evidence in a context relevant to the patient
- Remove the guilt related to posture by reframing language and understanding of posture
Advice and counselling:
- Encourage movement
- Discus pain-relieving postures in the context of specific pathology
- Ensure consistent messaging from the healthcare team to avoid confusion
Patient review:
- Check understanding of previously discussed concepts
- Support and encourage, changing beliefs and habits can take time
|
Posture versus movement
As discussed, current evidence does not support the dichotomous idea of ‘good’ and ‘bad’ posture being linked to pain. However, sustained postures can significantly contribute to pain. Bontrup et al found that there was a significant association between less movement between postures when sitting and increased risk of chronic LBP in a sample of call centre workers.21 This finding is reflected by Hanna et al,22 highlighting LBP risk showed a strong correlation with increasing time sitting but not seated posture.
With the current plethora of evidence suggesting ‘sitting is the new smoking’, movement and changing positions to reduce time in sustained postures are likely more important than posture itself. Even in adults achieving the World Health Organization’s targets for weekly exercise, sedentary behaviour of as little as four hours daily is linked with increases in both morbidity and mortality.23 Educating and empowering patients to feel confident about this will ideally allow them to manage many ‘postural’ conditions; priority is given to movement and changes in position, with less time and energy spent on finding the ideal posture. Although there is no consensus on the best way to break sedentary posture, a recent review summarised key points that clinicians can consider with patients to reduce sedentary postures, as shown in Table 2.24
| Table 2. Strategies to reduce sedentary posture24 |
| Method of reducing sedentary posture |
Specific examples |
| Task substitution |
- Alternate tasks so that different muscle groups or parts of the body are being used
- Alternate between sitting and standing while completing tasks
|
| Task interruption |
- Ensure breaks are taken, especially where there is high task invariability
- Use short breaks to perform stretching or suitable exercise to offload muscle groups used during sedentary tasks
- Use natural stopping points (between tasks, during/after phone calls, etc) to change position or stretch
|
| Increasing incidental exercise |
- Use stairs instead of the elevator
- Take part in walking meetings
- Walk or stand during meal breaks
- Use active methods for commute (walk, bike, bus, etc)
|
Posture and obesity
Obesity is a well-documented significant contributor to increased morbidity and mortality, but recent evidence suggests that it also affects postural adaptions.25 A recent cross-sectional study of 420 students found a statistically significant increase in the prevalence of knee valgus, exaggerated thoracic kyphosis and lumbar hyperlordosis in students who were overweight and obese.26 This finding is shared by several other studies, but so far there has been no clear evidence of this change in posture directly causing pain.27,28 However, as discussed previously, this is important to consider within an individual’s context. Consider an adolescent who is overweight playing a high-impact sport, such as basketball or netball, presenting with anterior knee pain. Increasing knee valgus, a sign of poor rotational control of the lower limb, increases anterior knee loads.29 Therefore, correcting this posture, and consequently improving control over knee valgus, would likely be key to reducing symptoms and maintaining participation. However, it is important to keep in mind that not everyone with increased knee valgus will experience pain because of this.
Conclusion
Posture is almost certainly associated with pain and morbidity, but this is likely to be a much weaker association than previously thought. There is also a strong argument that this association is more attributed to sedentary behaviour, which inherently involves sustained postures. However, in cases of clear pathology and/or specific context for the presenting patient, specific postural advice may be necessary to reduce tissue load, compression and sensitivity and to reduce ‘postural fear’. This is done with the evidence of a clinical history and physical examination. More broadly, it is important that clinicians ensure the language used promotes movement and reduces fear or fixed beliefs about posture and its role in spinal pain. Overall posture is a complex interaction of multiple factors, and a broad-brush approach of ‘good’ and ‘bad’ is not applicable.
Key points
- The concept of ‘good upright posture’ and ‘bad slouched posture’ is unsupported by research evidence.
- Patient history and beliefs and clinical examination are important for considering patient-specific contexts before giving advice.
- Clinician language and communication can help reduce fear and improve understanding.
- Movement is more important than any given posture.