Case
A boy aged eight weeks presented to a regional emergency department with 24 hours of worsening non-bilious vomiting (15–20 mL) after feeds and recurrent loose stools with mucus (4–6 episodes of each in the past day). The vomits were moderately intense (with some infant distress prior to vomiting) and mostly comprised of digested formula with some mucus. He had exhibited similar but milder symptoms since birth and had been trialled on several formulas, with some improvement on soy-based formula.
His mother described a transient bimalar rash developing after commencing formula feeding several weeks ago. Additionally, his father had cow’s milk allergy (CMA) as a child, and his mother had lactose intolerance.
The boy was born at 38 weeks’ gestation via an uncomplicated elective caesarean section after a straightforward pregnancy. His birth weight was 3.6 kg (70th percentile). At the time of examination (eight weeks of age), his weight was 5.3 kg (45th percentile). He was haemodynamically stable with an unremarkable abdomen and normal genitals. He was bright and alert between vomits and was admitted to the paediatric ward for observation and further assessment. He was reviewed by the paediatrician and considered to have possible CMA, so a trial of the extensively hydrolysed formula was recommended. He was discharged and his parents were instructed to re-present if there were worsening symptoms or red flags.
Question 1
What is CMA, and how is it managed?
Question 2
What are other differential diagnoses to consider?
Question 3
What are the red flags in a vomiting infant?
Answer 1
CMA is an immune-mediated reaction to milk protein and is the most common food allergy in infants aged <2 years, occurring in approximately 2%.1 It can present with an acute or delayed allergic reaction, the latter manifesting as vomiting, diarrhoea and irritability.2 A trial of soy or extensively hydrolysed formulas is usually the first-line treatment; however, a specialist referral may be warranted if the infant has ongoing symptoms or failure to thrive.2
Answer 2
Infant vomiting is a common presenting symptom for a variety of conditions that range from benign and mild to life-threatening (Table 1). It is important to consider factors such as age, duration and pattern of vomiting and associated symptoms to narrow down possible differentials.3,4 In young infants, the most common causes are physiological reflux, gastro-oesophageal reflux disease and dietary protein intolerance. As children age, the most common cause of vomiting becomes gastroenteritis.4
| Table 1. Differential diagnosis for vomiting infants (aged 0–1 years)2–5 |
| Condition |
Common characteristics and differentiating features |
| Gastro-oesophageal reflux (GOR) |
- Effortless, non-projectile vomits; small volumes
- Peaks at 3–4 months of age, generally stops by 12 months
- Ongoing appropriate weight gain
- ‘Happy spitters’
|
| Gastro-oesophageal reflux disease |
- GOR with adverse symptoms
- Symptoms are often non-specific, including irritability, feeding aversion and poor weight gain
|
| Food protein–induced enterocolitis syndrome |
- Profuse vomiting and diarrhoea
- Occurs 2–6 hours after ingesting trigger foods (eg cow and soymilk proteins)
|
| Gastroenteritis |
- Almost always associated with loose, watery diarrhoea
- Stools may contain blood/mucus, particularly if non‑viral cause
- Other common symptoms include fever, abdominal pains, myalgia and headaches
|
| Adrenal insufficiency |
- Chronic vomiting
- Most common cause (21-hydroxylase deficiency) is tested for in newborn screening
- Other symptoms include hypotension, ambiguous genitalia in females
- Hyponatremia, hyperkalaemia on biochemistry
|
| Hypertrophic pyloric stenosis |
- Projectile, non-bilious vomiting
- Occurs immediately after feeding
- Hungry after vomiting – ‘hungry vomiter’
- Palpable ‘olive’ in right upper quadrant secondary to the hypertrophied pylorus
|
|
Intestinal obstruction
Malrotation with/without volvulus
Intussusception
|
- Bilious vomiting
- Other symptoms include abdominal distension and pain, with signs of peritonism if prolonged presentation
|
| Inborn errors of metabolism |
- Rare; presentation depends on the type of metabolic disorder
- Recurrent vomiting with dehydration
- Associated growth/developmental delay
|
|
Infections
Urinary tract infection
Meningitis
|
- Fevers
- Focal signs and symptoms (eg neck stiffness, malodourous urine)
|
Answer 3
Red flags in a vomiting infant are:2–5
- signs of severe dehydration
- severe abdominal pain/distension
- haematemesis/haematochezia
- recurrent bilious vomiting
- projectile vomiting
- disproportionate haemodynamic compromise
- high-grade fever
- focal neurological changes/altered consciousness/head trauma.
Infants with pre-existing chronic diseases and failure to thrive should also be identified as high risk.
Case continued
The boy’s parents trialled extensively hydrolysed formula; however, this was poorly tolerated, with a refusal to accept bottles and worsening vomiting, so they reverted to a soy-based formula.
Three days later, the boy re-presented with severe projectile vomiting immediately after every feed. His heart rate was 113 beats per minute, and he was lethargic and mildly dehydrated. Biochemically, he had a metabolic alkalosis with respiratory compensation but no overt electrolyte derangement and normal inflammatory markers.
He was readmitted for suspected hypertrophic pyloric stenosis (HPS). A nasogastric tube was inserted, and he received fluid rehydration intravenously. An initial abdominal ultrasound showed gastric outlet obstruction with significant gastric distension and narrowing of the gastric lumen; however, no hypertrophied pylorus could be identified.
Given the high clinical suspicion, he was discussed with a paediatric surgical team at a referral hospital. He was transferred the same day for further assessment. A repeat abdominal ultrasound showed a pyloric muscular wall thickness of 5.7 mm, supporting a diagnosis of HPS (Figure 1).
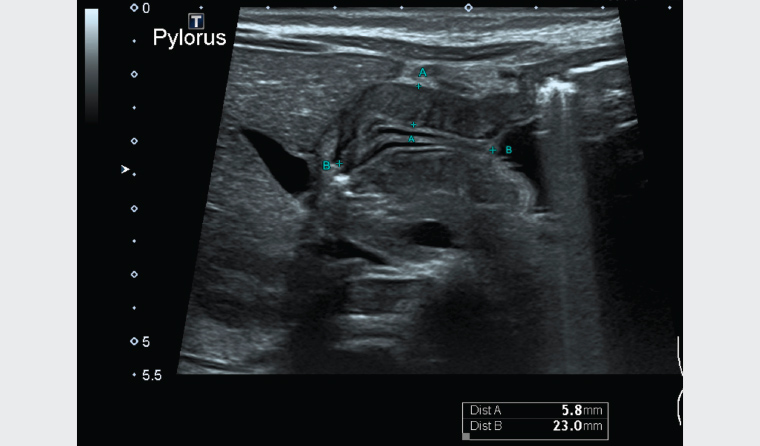
Figure 1. Abdominal ultrasound showing a pyloric muscular wall thickness of 5.7 mm (Distance A)
Question 4
What is HPS, and how common is it?
Question 5
What are the risk factors for HPS?
Question 6
How is HPS diagnosed and managed?
Question 7
What follow-up is required?
Answer 4
HPS is a disorder affecting infants, most commonly between the ages of two and 12 weeks, in which thickening of the pylorus leads to gastric outlet obstruction. It occurs in approximately three in 1000 live births and is thought to be due to a combination of genetic and environmental factors.6
Answer 5
Risk factors for HPS include male sex, preterm birth, firstborn child, formula feeding and use of macrolide antibiotics as infants (erythromycin and azithromycin).5
Answer 6
HPS is usually diagnosed with a combination of clinical assessment and imaging.6,7 Abdominal ultrasonography is the first-line imaging modality, with a pyloric muscle thickness >3 mm seen as the best discriminating factor.7,8 Experienced sonographers can yield a sensitivity and specificity of 97–100% and 99–100%, respectively.7 A fluoroscopic upper gastrointestinal series may be indicated if clinical assessment and ultrasonography are nondiagnostic; however, it is less preferred than ultrasonography because of the radiation exposure.7 Biochemically, a hypochloraemic, hypokalaemic metabolic alkalosis may develop as the disease progresses as a result of the ongoing large gastric losses.6
The definitive management for HPS is a pyloromyotomy – a curative surgical procedure during which the pylorus is incised to relieve the obstruction.9
Answer 7
Pyloromyotomies have excellent outcomes with minimal complication rates.9 After postoperative follow-up is completed, patients can revert to routine paediatric care to ensure appropriate feeding and growth.
Case continued
The patient had a successful laparoscopic pyloromyotomy with significant symptomatic improvement. On follow-up three months later, his weight was 8.9 kg (89th percentile), and he was growing well. He continued on soy-based formulas and had been commenced on solids. He was waiting to be seen by a paediatric allergy specialist for further evaluation of possible CMA.
Key points
- Vomiting in infants has a broad list of differentials, and determining the cause can be challenging.
- Parents should always be educated on the red flags in a vomiting infant.
- Pyloric stenosis should be considered in all vomiting infants, particularly if they are aged <3 months.