Previous national and state-based surveys have generally found self-reported influenza vaccination uptake in adults aged ≥65 years, who are predominantly vaccinated in general practice,1 to be fairly high (70% or greater) and similar to or better than that in other countries with developed economies.2 However, the limited data available on vaccination uptake in adults aged <65 years with high-risk medical conditions have suggested substantially lower uptake,3 as also found in other countries such as the USA and UK.4 Since the Australian Childhood Immunisation Register was expanded to the whole-of-life Australian Immunisation Register (AIR) in 2016,1 analyses of AIR data to date have identified substantial underreporting of influenza vaccination in adults.1,5 For example, influenza vaccination uptake recorded in the AIR for adults aged ≥65 years was 46.3% in 2018, although previous national surveys have reported approximately 70% coverage in this age group.1 Influenza uptake estimates in younger adults are likely even less accurate as a result of underreporting of vaccinations administered in workplaces, pharmacies and other non–general practice settings.1
While there are some data on the knowledge, attitudes and beliefs of Australian general practice providers in relation to influenza vaccination for children6 and pregnant women,7 there are limited data in relation to adults.3 The present study focused on two key high-risk adult groups: those aged ≥65 years, and those aged 18–64 years with a medical condition associated with an increased risk of influenza and complications.8 The aim of the study was to examine how influenza vaccination is delivered in general practice from the perspectives of general practitioners (GPs) and general practice nurses (GPNs), to make recommendations as to how to enhance program delivery and address any challenges.
Methods
Theoretical framework
This exploratory descriptive qualitative study was underpinned by the Capability–Opportunity–Motivation model of behaviour change (COM-B model; Figure 1).
9 To engage in a specific behaviour (B), the COM-B model proposes that at any time, a person must have physical and psychological capabilities (C) and have the physical and social opportunities (O) to undertake the behaviour.
9 Critically, the person must want to undertake the behaviour (motivation [M]). In this context, the behaviour is identifying the need for, discussing, recommending and/or delivering influenza vaccination despite barriers and competing factors.
10 The COM-B model recognises the importance of understanding behaviour in context (in this case, general practice) and why a particular strategy (in this case, recommending influenza vaccination of high-risk adult populations) may not be as effective as it could be.
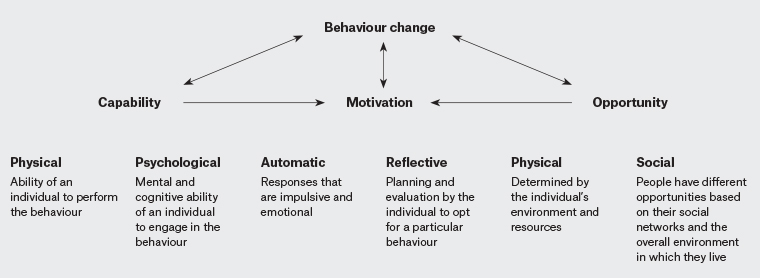
Figure 1. The Capability–Opportunity–Motivation model of behaviour change9
Recruitment
The study involved two participant groups – GPs and GPNs. Participants were recruited via an email invitation distributed by Healthed (a private provider of continuing professional development/education to health professionals) and by the Australian Primary Health Care Nurses Association to their mailing lists. The email contained a letter of introduction and a participant information sheet outlining details of the study and a consent form. Potential participants contacted a member of the research team (SR) by email or telephone to indicate their willingness to participate.
Thirty-eight expressions of interest to participate were received. Thirty potential participants met the criteria of being either GPs (n = 15) or GPNs (n = 15). On receiving further information and one follow-up email, 14 participants were recruited: GPs (n = 6) and GPNs (n = 8). Reasons for non-participation included lack of time to be interviewed, no financial incentive and no further response.
Data collection
An interview guide with questions aligned with the COM-B model was piloted and then refined (Box 1). All interview data were collected in January and February 2019, by an experienced qualitative researcher (SR). The interviews were conducted by telephone (ranging in duration from 22 to 43 minutes), audio-taped with permission and transcribed verbatim by SR. Three participants asked to review their transcripts; none returned any comments.
| Box 1. Semi-structured interview questions |
- Tell me how implementation of influenza vaccine in adults is addressed currently in your practice.
- What opportunities exist to discuss, recommend and deliver immunisation with adults over 18 years of age with chronic disease?
- What barriers exist to discuss, recommend and deliver immunisation with adults over 18 years of age with chronic disease?
- What opportunities exist to discuss, recommend and deliver immunisation with adults over 65 years of age?
- What barriers exist to discuss, recommend and deliver immunisation with adults over 65 years of age?
- What motivations exist for you as an individual practitioner in primary care to discuss, recommend and deliver immunisations with adults over 18 years of age with chronic disease and with adults over 65 years of age?
- What motivations exist for the practice in which you work to discuss, recommend and deliver immunisations with adults over 18 years of age with chronic disease and with adults over 65 years of age?
- How do resources impact on your ability to discuss, recommend and deliver immunisation to the adult groups discussed? Resources may be provider (personal) resources or resources at the practice level.
- Is there anything else you would like to add in relation to influenza vaccination in adults?
|
Data analysis
Two authors (SR, AW) used a qualitative content analysis approach. Deductive content analysis using an iterative process of a priori coding informed by the COM-B model was undertaken.9 Themes were identified and supported by participant quotes (Table 1).
Ethical approval for the research was granted by the University of Sydney Human Research Ethics Committee (Project No. 2018/899). Data were stored in a secure university server.
| Table 1. Themes and participant quotes |
| Capability–Opportunity–Motivation model of behaviour change component |
Key themes |
Examples of quotes from interviews |
Capability:
Physical |
- Safe administration of injection
- Record keeping
- Fatigue
|
‘End of the day the last thing you want is to engage with a patient who is reluctant to have the vaccine so doctor fatigue is a barrier.’ (General practitioner [GP] 5) |
Capability:
Psychological |
|
‘So where we are dealing with cognitive decline we are often worried about other things like self‑care, so often we are distracted by that and not thinking about flu immunisation as much … We get distracted.’ (GP 4)
‘We have a system, where the nurse initially triages the patient and does the initial blood pressure/pulse and sees if there is anything they can do, might collect urine and I rely a lot now on the nurses to see what this patient is being flagged for. Are they due for flu vaccination and to remind me. Tell the patient they are due and come back to me after you have seen the doctor.’ (GP 2) |
Opportunity:
Social |
- Opportunistic
- Reminder at 65 years
- Change in timing
- Younger and fitter people
|
‘Largely it is down to the relationships that GPs have with their patients.’ (GP 3)
‘When you are forthright, people don’t often say no.’ (GP 4)
‘I think we are very aware that Aboriginal people may get chronic disease a lot earlier than the general population.’ (GP 2)
‘When they ring up or when we are triaging we say have you had your flu vax. People who come in for routine [international normalised ratio tests], [vitamin] B12, things like that, we offer flu vax while we are there and discuss when they are due.’ (GPN 5)
‘When they come in for something else I opportunistically offer it then.’ (GP 3)
‘It’s like trying to hold them back at the door.’ (General practice nurse [GPN] 6)
‘To be across people who are living with these things and their condition is so much part of their lifestyle, they don’t think that it makes them much different to anyone else.’ (GP 4) |
Opportunity:
Physical |
- Environment
- Stock availability
- Privacy
- Role of pharmacies
|
‘1) We need good reliable supply of the vaccine, 2) to have nursing support for observation and administration of the process, 3) enough waiting room space, because we have so many doctors because the waiting room can be full of people just being observed, so space in the clinic. And space to treat any immediate complications so a resuscitation area.’ (GP 5)
‘If you haven’t got the vaccine, you can’t give it. That does happen.’ (GP 3)
‘All the practices in town lend within each other so we lend to other practices and if we think we are running out or low, they lend to us.’ (GP 2)
‘It’s privacy in the treatment room, so there’s no privacy.’ (GPN 4)
‘We have wall posters that are put up. During flu season someone sends them to us. They are usually around to remind people to get it done so that is useful.’ (GP 6)
‘We have people with English as a second language but it’s not so helpful to give them something in English. We can get brochures in a different language for childhood immunisations but not flu.’ (GPN 8)
‘I am concerned about potential hazards. So how would a pharmacist manage someone who has a syncopal collapse because they have freaked out because they are having a needle or if they have an allergic reaction? How do they manage confidentiality and medical records? The other problem with the pharmacy program is that there is fragmentation of healthcare so we are not getting info that patients have had vaccines and so we are flagging people down to say come and get your vaccine but they have already done it but we don’t know what they have had’. (GP 6) |
Motivation:
Basic/automatic |
|
‘I want to keep individuals and therefore the community safe.’ (GPN 4)
‘Sicker people are harder to work with.’ (GP 4) |
Motivation:
Reflective |
- Beliefs outside of practice delivery
|
‘I believe strongly in public health and it’s my job to promote health.’ (GP 6)
‘We do a couple of house calls and would take the flu jab to them.’ (GP 6)
‘For the past 15 years I have set up my practice at an agricultural event and each year I vaccinate about 500 people.’ (GP 5)
‘Primary care is not a unified state.’ (GP 4) |
Results
Fourteen participants, including six GPs and eight GPNs, were recruited. GPs were recruited from four states (New South Wales [NSW; 2], Victoria [2], Tasmania [1] and Queensland [1]), with experience in primary care ranging from five to 42 years. GPNs were recruited from four states (NSW [4], South Australia [2], Western Australia [1] and Queensland [1]), with experience in primary care ranging from five to 20 years. Of the 14 participants, seven were from metropolitan settings, five from regional settings and two from rural settings.
COM-B analyses of influenza vaccination in general practice
Capability
Participants perceived that they possessed the physical capabilities, including both clinical skills (administering a vaccination safely, ability to deal with anaphylaxis and other emergency situations, and record keeping) and organisational skills (implementing different modes of vaccination delivery), to provide influenza vaccinations effectively. Practices were perceived to provide vaccinations via multiple modes – within consultations with individual patients on both a purposefully arranged and opportunistic basis, and by implementing ‘influenza clinics’ involving influenza vaccination of multiple patients during a specific time period, thus increasing practice vaccination capacity in a time-efficient manner. Although influenza clinics were a commonly reported model that was either GP or GPN led, other models such as local authority–run clinics also existed, and one participant also worked in this setting.
In contrast, participants reported challenges in psychological capability that reduced their ability to deliver influenza vaccination effectively. This was associated with forgetting to inquire about influenza vaccination status because of the complexity of presenting issues and time pressures within consultations. Overcoming these issues and increasing the psychological capability of general practice in delivering influenza vaccination was facilitated by the use of practice software and working as a team. Although practice software provided a means of identifying patients who required a vaccination and could facilitate active patient follow-up and recall, this was reported to be dependent on the variable quality of vaccination documentation recorded in the electronic medical record systems.
Participants reported teamwork between the GP and GPN. Within the team, each clinician had a specified role, often with the GPs reliant on the GPNs to triage patients and flag when vaccinations are required. This team approach increased the psychological capability of the practice to deliver influenza vaccination effectively by providing a ‘safety net’ to reduce the likelihood of missing people who needed influenza vaccination.
Opportunity
GPs and GPNs reported that patients in high-risk groups (notably those aged ≥65 years) actively sought opportunities to be vaccinated against influenza during consultations, indicating a high level of acceptance and normalisation of receiving an annual influenza vaccination. Many participants also discussed the implementation of annual dedicated ‘influenza clinics’ and reported opportunistically recommending and providing influenza vaccination during consultations.
Practice software systems that allowed recall and reminders to be sent to patients and resources such as leaflets and posters were helpful as additional reminders to patients. As influenza is seasonal, participants noted the pressure that running influenza vaccination clinics or providing opportunistic vaccination added to routine work.
Several participants commented on the lack of clarity regarding the optimal timing for influenza vaccination resulting from changes to guidelines in 2018.11 This was reported as confusing for patients and resulting in missed opportunities to vaccinate. Patient privacy was seen as an issue when the practice environment was busy and the treatment room was being used for multiple patients concurrently.
National policy that promotes and funds the influenza vaccine program provides an environment that facilitates uptake of the influenza vaccination. All GPs and four GPNs noted that the strong recommendation and funding of influenza vaccination under the National Immunisation Program for all adults aged ≥65 years, as opposed to only individuals with underlying medical conditions in the 18–64-year age group, made it easier to reach older adults. Opportunities to reach high-risk younger adults were afforded when patients were on GP Chronic Disease Management plans, which require regular appointments for review. However, patients with medical conditions who were under the care of a specialist physician were reported to be harder to reach.
GPs and GPNs raised concerns regarding pharmacies providing influenza vaccination for high-risk adult populations. While there was some acknowledgement that allowing pharmacists to administer influenza vaccine had positive outcomes, including increased access and opportunity to receive a vaccination, participants also noted what they perceived as a disruption and barrier to the individual’s continuity of care.
Other barriers included physical resources at a practice level that affected capability to maximise influenza vaccine delivery. Examples that were given included a lack of privacy for patients in treatment rooms when ‘usual care’ continues in influenza vaccination season. Fridge storage space was noted as a finite resource.
GPs and GPNs reported engaging in creative and pragmatic behaviours to create an environment that enabled physical opportunities to administer influenza vaccines to multiple patients over short periods. Strategies included instigating influenza clinics with extended hours held at weekends. Stock shortages, especially in the 2018 season, led to patients becoming upset and frustrated. However, some GP and GPN participants reported working in partnership with other practices locally to share vaccination supplies to meet supply and demand issues as needed.
Motivation
Participants perceived that GPs and GPNs held the innate motivation required to achieve high levels of influenza vaccination for their high-risk patients. For many participants, this motivation was influenced by an altruistic desire to keep individuals and communities healthy, and thus they viewed influenza vaccination as an important preventive strategy. These desires led to many participants actively seeking opportunities to administer the vaccine including during home visits, in residential care facilities and at local community events. Despite indicating high levels of motivation, factors such as provider fatigue and complex consultations were noted to have a negative impact on the administration of the influenza vaccine at times.
Discussion
The present study showed that GPs and GPNs reported having, in general, the capability, opportunity and motivation to effectively implement the influenza vaccination program in Australian primary care. However, challenges identified include time pressures, complexity of patient consultations, and vaccination supply inconsistencies.
General practice was found to use three main clinical models to implement the influenza vaccination program: 1) influenza vaccination clinics led by either GPs or GPNs, 2) planned vaccination-focused consultations and 3) opportunistic vaccination during routine consultations. The use of influenza clinics and opportunistic vaccination during routine consultations were the most common models reported. These models all offer opportunities to increase influenza vaccine uptake in the high-risk adult population. Opportunistic influenza vaccination has been shown to be an effective strategy in capturing less motivated patients who would be less likely to book a follow-up appointment12 and/or perceive that they do not need vaccination.13
The change in recommendations in 2018, which emphasised the benefit of timing influenza vaccination to ensure optimum protection (achieved 3–4 months after vaccination) in the peak months of influenza circulation (June to September),11 reportedly confused and angered consumers accustomed to vaccination as soon as the vaccine became available and became a barrier to both planned and opportunistic vaccination. Consistent health messages regarding the optimal timing of seasonal influenza vaccination and the ongoing benefits will be important to maintain motivation for future provider and patient engagement.
Pharmacy influenza vaccination was mentioned by all participants. While some recognised the benefits, most notably increasing access, there was consistent concern about governance and continuity of care. These concerns were perceived as barriers. Although other models such as council-run clinics exist, the same level of concern was not raised. This may be due to council-run clinics being an established service run by nurses with or without GPs, while pharmacist vaccination is new and involves a different professional group. Most pharmacist vaccinations are for influenza.14 If all pharmacists were required to provide details of vaccinations to a patient’s nominated GP, as is already the case in Victoria, Queensland and the Australian Capital Territory (although the extent of compliance monitoring is unclear), this could partly address these concerns and avoid the need to check AIR data, which are known to be underreported for influenza vaccination.14
Primarily, general practice approaches delivering influenza vaccines in high-risk adult groups are part of routine preventive care processes for patients aged ≥65 years or younger adults with chronic medical conditions. Motivation of the participants to deliver influenza vaccine to high-risk adults was clear. A term used to describe practitioners who see vaccines as having social value is ‘assertive physicians’.15 Some of the participants in the present study fitted this description because they sought to vaccinate at community events, as well as vaccinating housebound patients and those in long-term care facilities. The views of individual GPs are likely to influence whether active strategies are pursued beyond the clinic.16
Challenges identified to providing influenza vaccines included patient beliefs and structural issues such as inefficiencies in the supply chain. Additional challenges included physical space to accommodate extra patients in the clinic building and fridge space; at times, the ability to meet cold chain storage requirements affects general practice’s ability to make influenza vaccine delivery an integrated part of care. One of the greatest reported difficulties in delivering influenza vaccines was the lack of adequate and predictable vaccine supplies each year. Influenza vaccine supply issues have previously been identified as an issue with the potential to affect vaccination uptake.17 What was clear from the present study was that the motivation of participants towards delivering influenza vaccination did not change, but vaccination delivery could become fragmented when factors such as supply issues affected their capability and opportunity.
The participants reported that adults aged ≥65 years were easy to target, but younger adults with chronic medical conditions were harder to reach. This is in line with a previous study undertaken in the UK that noted younger patients often deemed themselves ‘too well to attend’ or were under the care of a consultant and therefore had less direct contact with their GPs.18
Challenges to vaccine delivery resulting from provider fatigue and complex consultations could be addressed by making influenza vaccination recommendations a whole-of-practice staff responsibility, such as engaging receptionists to remind patients.
Limitations
The small sample size may not be representative of the views of all GPs and GPNs. Participant time constraints curtailed the opportunity to probe deeply, although saturation across topics was reached.
Conclusion
This study shows that there is both capacity and motivation in general practice to deliver influenza vaccine to high-risk adults, consistent with the relatively high uptake achieved in Australia, particularly in older adults. To further enhance influenza vaccine uptake in high-risk adults, clear and consistent messaging about the optimal timing of influenza vaccine is needed to maintain patient trust, along with assured supplies of vaccine. To achieve this, a more efficient supply chain is needed, which will require collaboration across sectors including vaccine manufacturers, government agencies and general practice. These findings are also highly relevant to COVID-19 vaccination, given the key role of general practice in rollout and that vaccination may eventually be needed annually as with influenza.