Case
A boy aged 13 years presented with a painful red left eye persisting for two days. Initially noticed as a foreign body–like sensation on waking, the symptoms gradually worsened over 24 hours, with associated reduced vision. There was no history of trauma or foreign body entering the eye. He had no significant past medical history. Visual acuity in the right eye was 6/12 (6/6 pinhole), and in the left was hand movements at 30 cm (no improvement with pinhole). He was systemically well, afebrile and had no periorbital erythema. Intraocular pressure was normal. Ocular examination findings are shown in Figure 1.
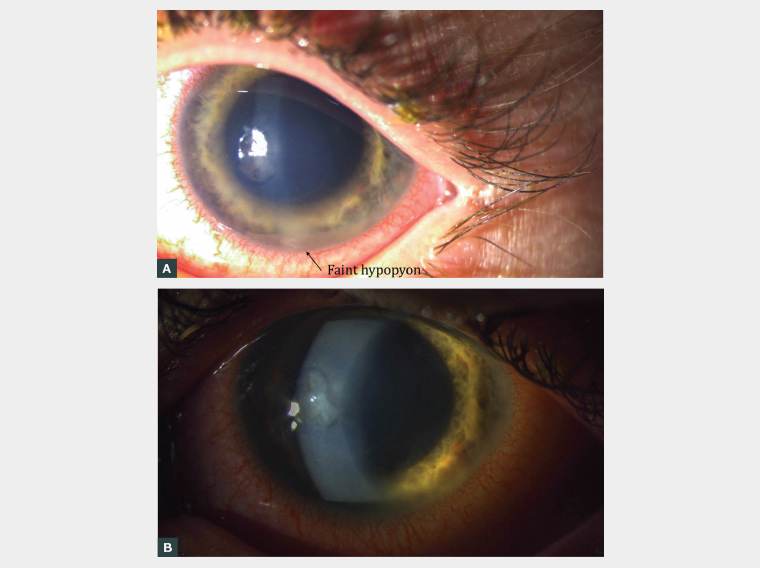
Figure 1. Left eye examination findings
A. External photograph of the left eye illustrating a small central infiltrate and faint hypopyon inferiorly; B. Slit lamp magnified photograph of the left cornea further illustrating the central stromal infiltrate, which measured 2.2 mm. On staining with fluorescein, there was a similarly sized round epithelial defect overlying the infiltrate (not imaged). Please note the pupil has been pharmacologically dilated.
Question 1
What is the most important additional question to ask regarding this patient’s ocular history?
Question 2
If this history was positive, what is the likely diagnosis?
Question 3
How would you manage this case?
Answer 1
For anyone presenting with a red eye, it is pertinent to ask about contact lens wear. This particular patient and his mother were unaware of the potential complications associated with contact lens use, and as they did not associate his contact lens use with the presenting problem and did not spontaneously mention his use until it was specifically enquired about.
It would also be important to enquire about any other ophthalmic conditions or surgery, as after trauma, these are other common causes of this condition.1
In contact lens wearers, other key history includes type of lens, schedule of use, recent misuse, lens cleaning practices (particularly any washing in tap water), recent swimming or trauma.
Answer 2
This child had a faint but clearly identifiable 2.2 mm corneal infiltrate that stained with fluorescein. He also had a subtle hypopyon. The diagnosis was contact lens–related microbial keratitis. Although the most common pathogen is bacteria, fungi, amoeba and viruses can also be responsible.2
The other clue to serious pathology was the significantly reduced visual acuity in the left eye that did not improve with pinhole; however, it must be noted that many serious ocular pathologies can initially present with normal vision, including microbial keratitis.
A red eye in a contact lens wearer should be assumed to be a microbial keratitis until proven otherwise. This is a sight-threatening emergency.
Answer 3
This patient required urgent ophthalmology assessment. It is not uncommon for such a patient early in their presentation to present to a local general practitioner (GP); however, the case should be discussed immediately with your local on-call ophthalmology registrar or ophthalmologist, and should not simply be treated with eye drops unless advised by the ophthalmologist. Chloramphenicol is not a sufficient treatment for microbial keratitis, as many common causative organisms, such as Pseudomonas aeruginosa, are resistant to this antibiotic.3 The ophthalmologist will also likely perform a corneal scrape for microbiological sampling. Commencing antibiotics prior to this could interfere with pathogen identification and is another reason to discuss the case prior to starting any drops.
Case continued
This patient was myopic and wore orthokeratology lenses (also known as Ortho-K lenses). These are a type of contact lens worn only at night, designed to temporarily flatten the curvature of the cornea, resulting in a reduction in myopia and potential slowing of myopic progression.4 The use of orthokeratology lenses is becoming more common,5,6 particularly in the younger population. Although there are studies supporting the use of orthokeratology lenses to slow the progression of myopia, further research is required to determine whether they provide a sustained long-term effect.4,7,8 Similar to any contact lens, orthokeratology lens use increases the risk of microbial keratitis, corneal scarring and irreversible vision loss. Possible mechanisms for this increased risk include a compromised ocular surface barrier, a stagnant tear pool trapped under the contact lens for long periods and corneal hypoxia.9 Two studies have reported rates of microbial keratitis in paediatric orthokeratology patients. The first found rates of 13.9 per 10,000 per year; these rates were significantly higher in children compared to adults.10 The second study found marginally lower rates.6
The child’s mother did not recall being informed of the risk of microbial keratitis, highlighting the need for prescribing practitioners to regularly discuss the uncommon but significant risks of treatment, as well as stressing the ‘red flag’ symptoms and what they should do if they occur.
This patient was admitted to the local children’s hospital under ophthalmology, underwent a corneal scrapeand was started on hourly topical fortified cefazolin and gentamicin (both day and night). Topical steroid was later added. His corneal sampling was negative for herpes simplex viruses, fungi and acanthamoebae. Although there was no bacterial growth cultured from his corneal scrapings, he responded well to topical antibiotics, which were slowly tapered off. He was left with a faint corneal scar.
Key points
- Contact lenses are a common cause of microbial keratitis. Always ask if the patient uses them in the context of a presentation of red eye or visual concern.
- Do not assume that younger children do not wear contact lenses; they can be used at all ages for various reasons.
- Any corneal abrasion seen in a contact lens wearer should be examined with a slit lamp (there might be a small infiltrate/opacity not visible to the naked eye).
- It is possible to cause a traumatic corneal abrasion when removing a contact lens; however, the history is typically clear – immediate pain on removing lens. Make sure to exclude a corneal infiltrate/opacity before diagnosing an abrasion.
- Always check visual acuity.
- If microbial keratitis is suspected, the case should be immediately discussed with your local ophthalmology service.