Discussion
There are excellent alternatives to the use of gas in domestic appliances and some simple behavioural changes that can reduce exposure in situations where appliances cannot yet be removed. CO poisoning can be insidious. Mild exposure can cause headache, nausea, vomiting, dizziness, malaise and confusion, so it can be mistaken for common conditions such as influenza or gastroenteritis. The COMA mnemonic is clinically useful. Increased awareness of these issues can provide patients with safer and healthier living environments.
Sixty five per cent of houses in Australia use gas for cooking or heating, and while this was once seen as clean and cheap, we now understand that gas combustion products have substantial negative health impacts, and the widespread use of gas in domestic settings is an avoidable health risk.1 The two most important gas-related health impacts are the respiratory effects of nitrogen dioxide (NO2) and the toxicity due to acute or chronic exposure to carbon monoxide (CO). This article examines the health impacts of indoor exposure to gas combustion products and what patients could do to minimise these.
Nitrogen dioxide
In the flame of a gas stove, the gas methane combines with oxygen from air to produce both heat and light. Some of the nitrogen from the air is oxidised in the flame, producing several nitrogen oxides such as NO2, nitric oxide (NO) and nitrous oxide (N2O), sometimes collectively referred to as NOx. NO2 is a respiratory irritant, while NO is harmless to humans. Gas flames also release formaldehyde (CH2O), CO and fine particle air pollutants. In addition, any high-temperature cooking process – such as frying or using a wok – will also release fine particles regardless of the heat source.
NO2 is a respiratory irritant that can directly cause airway constriction and sensitisation to allergens.2 In population studies it is associated with both the development of asthma and asthma attacks. Based on a meta-analysis of 19 studies, the odds ratio (OR) for current asthma in children exposed to gas cooking is 1.42 (1.23–1.64); consequently, for a child with current asthma who lives in a home with a gas stove, 30% of their risk of asthma is from the stove.3 Australian researchers have estimated that, across the community, 12% of childhood asthma is attributable to the use of gas cooking stoves.4
An increased risk of asthma has also been shown for adults. In the Tasmanian Longitudinal Health Study, indoor air exposures were studied for 3314 people for 10 years, from an average age of 43–53 years. Those with gas heating and cooking had an OR 2.64 (1.22–5.70) for persistent asthma symptoms when compared with the reference group, who were least exposed to household air pollutants.5 This study also showed deleterious effects in those groups exposed to wood heating and tobacco smoke.
Gas space heating is also a source of NO2 and other pollutants.6 Heaters can be fully flued (in which case no combustion products enter the indoor air), unflued (in which case all combustion products are released into the room) or open flued (which are designed halfway between these), as illustrated in Figure 1. Use of unflued gas heaters in school classrooms was tested in an elegant randomised controlled trial in NSW schools in the cold regions of the Blue Mountains and Southern Highlands. Blinding was achieved by building each classroom an enclosure with both a flued and a modern ‘low NOx’ unflued heater. Teachers could control the heating but in each week did not know which heater was working. There was a statistically significant increase in respiratory symptoms during the weeks with unflued heaters when compared with the flued heater weeks.6 This is strong evidence of harm from unflued gas space heating, and while this study only measured short-term effects, there are also longer-term effects that would be missed by this design, so the total health effect is likely to be larger than reported.
The Victorian government currently runs a subsidy scheme to remove gas heaters from community housing and cheaper rental properties, replacing them with reverse-cycle air conditioners. While this has been proposed on energy efficiency grounds, there will be health benefits each time an unflued or open flued heater is removed.7
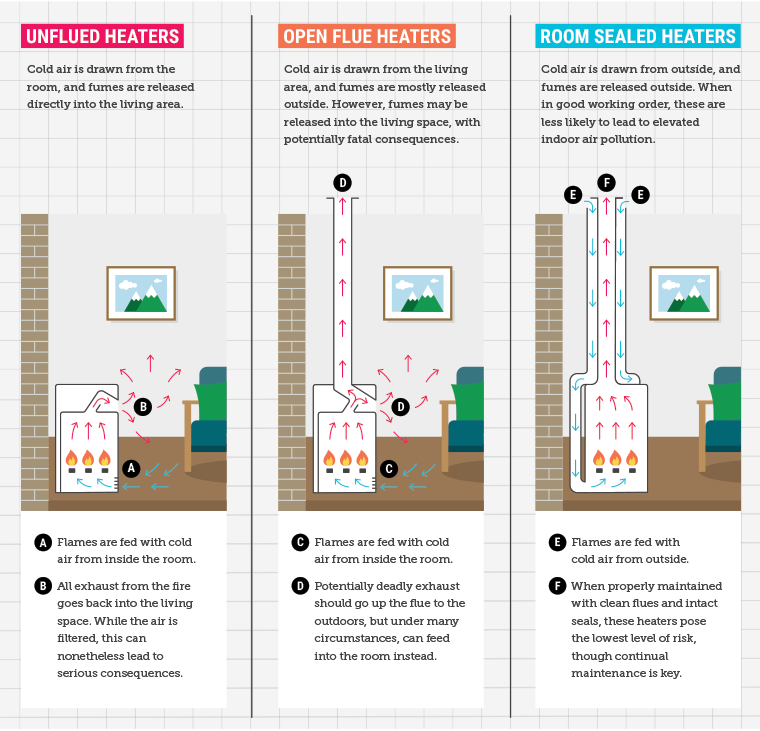
Figure 1. Types of gas space heaters
Reproduced from Bambrick H, Charlesworth KE, Bradshaw S, Baxter T, Kicking the gas habit: How gas is harming our health, Potts Point, NSW: Climate Council, 2021. Licensed under CC BY 3.0 (https://creativecommons.org/licenses/by/3.0).
Clinical implications
Questions about indoor gas exposure should be part of the clinical review of all patients with asthma. If their exposure is intermittent, symptom diaries or peak flow records can help identify those patients adversely affected by combustion products. Advocacy by their doctors may help patients in poorly maintained rental properties have their home environment improved (Box 1).
| Box 1. Patient vignette |
Alyssa, aged 14 years, attends the general practitioner (GP) with her mother, Karen. Alyssa lives with her parents and younger sister in a two-bedroom rented house. She has had asthma since early childhood, and it is always worse in winter. It is now affecting her school attendance and interfering with netball. She has had to stop playing to treat her asthma and missed some games this year.
Alyssa uses a salbutamol inhaler as needed most nights and an inhaled steroid preventer from autumn through to spring.
Her GP enquires about indoor air quality and learns that nobody smokes in the house, there is a gas stove and oven, there is a rangehood that filters but is not ducted to the outside, and heating is all electric. Alyssa does homework at the kitchen table after school and in the early evening. Windows are kept closed in winter to conserve heat.
In discussion with Karen, the GP makes some suggestions to reduce exposure. It is not possible to remove the gas stove, but Karen is interested in a bench top induction cooker that can be used for all single pot cooking and feels she can afford one of these for approximately $100. There is a kitchen window that could be opened when it is not too cold, and Alyssa suggests she could do her homework in the living room instead. The rangehood has been increasingly noisy this year, and Karen hopes it will be replaced. The GP offers to write a letter to the family’s housing provider supporting that a new rangehood should be ducted externally. |
Carbon monoxide
CO is an invisible, odourless gas produced by the incomplete combustion of hydrocarbon fuels. It binds strongly with haemoglobin, displacing oxygen, resulting in tissue ischaemia as well as direct toxicity at the cellular level.8
In developed countries, the most important source of exposure to CO in indoor air is emissions from faulty, incorrectly installed, poorly maintained or poorly ventilated cooking or heating appliances.
In some homes with an open flued gas heater, using a bathroom exhaust fan or kitchen rangehood can generate enough negative pressure to draw into the indoor living area exhaust gases that would otherwise go up the flue. Installing a CO alarm is a positive step for prevention, but this is not a substitute for regular servicing of heaters. Lower income households may be at greater risk of exposure, as shown by research in the UK, which found those in rural, disadvantaged or ethnically diverse areas at greater risk for CO poisoning–related hospital admission.9 In Victoria, landlords are required by law to have gas heaters in rented homes serviced every two years.
It is thought that CO poisoning in general may be responsible for more than half of all fatal poisonings worldwide.10 Problems of underdiagnosis and underreporting are well recognised, and accurate data on morbidity and mortality from household CO poisoning in Australia are difficult to obtain. However, there is no doubt that avoidable deaths and hospitalisations continue to occur. One of the most tragic incidents in recent memory was the death of two brothers from Victoria, aged six and eight years, who died after going to sleep in a bedroom with an open flued gas heater.11
Clinical implications
CO poisoning can be a challenge to diagnose, as symptoms are often non-specific and can be confused with common conditions. Furthermore, symptoms may fluctuate over time, lessening when leaving and worsening when re-exposed to the source.
Symptoms vary depending on the level and duration of exposure. Mild exposure can cause headache, nausea, vomiting, dizziness, malaise and confusion so can be mistaken for common conditions such as influenza or gastroenteritis.8,10,12–14 Severe poisoning can lead to chest pain, cardiovascular disease, coma and death.8 Headaches are the most common symptom of CO poisoning, with CO exposure found in approximately 6% of people presenting with headache to an emergency department.13 In approximately 10–30% of patients with acute CO poisoning, a delayed neurological syndrome – including cognitive and personality change, dementia and parkinsonism – may develop after a period of initial recovery.8,15
Diagnosing CO poisoning relies on having an index of suspicion, taking a thorough history and asking about the patient’s environment. Victorian Department of Health advice provides the mnemonic COMA, in asking the patient:14
C Are Cohabitors or other occupants of the building affected (including pets)?
O Does the Outdoors improve symptoms?
M Have gas appliances been Maintained/serviced?
A Do they have a working CO Alarm, and did it alert the person?
The problem of poor indoor air quality is exacerbated by measures to seal air leaks to reduce heating costs, so modern housing is less leaky and retains indoor pollutants. There is low community awareness of the health risks from gas, and many people have grown up with it as a ubiquitous exposure to which they never give a second thought. Gas has been marketed to the community as ‘natural’, as if it was any more natural than other material mined from the earth, such as oil or iron ore. As there are now excellent alternatives for all previous domestic uses of gas, it is time to reconsider the widespread use of this product in people’s homes.
Practical measures to reduce exposure
- Improve ventilation by opening windows or doors and turning on a rangehood every time the stove is used.
- Beware of the dangers of negative pressure when using exhaust fans and open flued gas heaters without adequate ventilation.
- Replace gas stoves with induction stoves.
- Remove unflued gas heaters.
- Make sure flued gas heaters are serviced regularly.
- Install and maintain CO alarms.
Summary
The current suggestion to ‘electrify everything’ on climate grounds will have substantial health benefits if it leads to the reduction in gas use in people’s homes. As 2.7 million Australians have asthma, even a small reduction in incidence or severity will be of great value.16 With highly efficient reverse-cycle air conditioning for heating and induction stoves for cooking, there is no ongoing need for new houses to have a connection to a gas supply, and some jurisdictions are planning gas free suburbs. The problem of CO poisoning is a diagnostic challenge that needs greater awareness by clinicians to avoid preventable illness and deaths.
Implications for general practice
Asking patients about indoor gas use will help some people minimise their exposure and reduce their asthma symptom burden. Awareness of low-level CO poisoning is important as the symptoms mimic many common conditions. Questions about heating should be routine for patients with vague symptoms during winter months.
Patient resources