Using our limited antibiotics wisely is everyone’s concern: doctors, patients, policymakers and especially our children, who may live in a post-antibiotic future. Antibiotic resistance is a rising global threat with only two options for mitigation: 1) invent new antibiotics and/or 2) use current antibiotics more wisely. Both options will be necessary and complementary. However, a 2021 World Health Organization (WHO) report1 noted that of the 11 new antibiotics approved since 2017, only two represent a novel class, and concluded that ‘[o]verall, the clinical pipeline and recently approved antibiotics are insufficient to tackle the challenge of increasing emergence and spread of antibiotic resistance’.
Antibiotic resistance increases in proportion to total antibiotic usage. In Australia, the majority of antibiotic usage is in the community, hence primary care has a key role in optimising appropriate prescribing.2 Periodic efforts to reduce overuse have had modest and temporary effects, pointing to the need for sustained programs. Australia could learn from antibiotic stewardship programs of other countries such as Sweden’s Strategic Programme Against Antibiotic Resistance (Strama),3 which commenced in 1995 when prescribing rates were close to Australia’s. Antibiotic usage has reduced by approximately 7% per year over two decades since Strama was established and now is less than half that of Australian primary care.4 Briefly, Strama is a network of local groups (including general practitioners [GPs], infectious disease physicians, microbiologists and pharmacists) who organise a variety of programs in antibiotic stewardship (eg prescriber feedback with peer comparison, guidelines, courses and lectures). The network shares their local data and methods and meets nationally at least annually, supported by a national secretariat.5
Clinical practice guidelines for antibiotic use (eg Therapeutic Guidelines: Antibiotic) are well accepted and widely available in Australia.6 Nonetheless, the availability of guidelines alone is insufficient to ensure optimal prescribing. It is important to determine which specific policies and clinical strategies have been effective, and which might be most worthwhile and feasible in Australia. In this article, the authors examine the evidence for a range of policies and propose several recommendations for a sustained antibiotic stewardship program and research in Australia.
Evidence-based strategies for antibiotic stewardship
Prescribing and overprescribing of antibiotics occurs for many reasons; hence, there is no single ‘magic bullet’, but instead a range of approaches is needed.7–9 These can be divided into regulatory, policy and clinical (Table 1).
Regulatory interventions
Regulatory efforts are crucial to reduce antibiotic resistance. In Australia, antibiotics are nearly always supplied via prescription and written by an approved prescriber. In countries with limited regulations, antibiotics may be supplied without prescription.10 This is associated with greater use of broad-spectrum antibiotics including amoxicillin, amoxicillin/clavulanic acid, azithromycin and fluoroquinolones where more effective narrow-spectrum antibiotics could be used as first-line therapies.11
The Pharmaceutical Benefits Scheme (PBS) subsidises medications if they are prescribed for an approved indication. Prescribers can write a private prescription for unapproved indications, but patients will pay the full cost of the medication. Despite the current regulations in place in Australia, there are additional drivers that could be used to optimise prescribing.
Limiting repeat courses of antibiotics can help with reducing inappropriately long courses or later inappropriate use of the repeat script. Prior to April 2020, many GPs’ electronic medical records defaulted to the maximum number of repeats available under the PBS, potentially inadvertently encouraging injudicious overuse of antibiotics. Notably, amoxicillin, amoxicillin/clavulanic acid, cefalexin, doxycycline and roxithromycin represented 78% of all repeats prescribed on the PBS in 2019.12
A number of changes were introduced to the PBS in April 2020 to support better alignment with guideline-recommended treatment duration and to avoid inadvertent repeat prescribing:13
- new Authority Required listings for repeat antibiotic prescriptions in line with Therapeutic Guidelines6
- amendment of the maximum quantity and repeats for some listings to enable a full recommended course of antibiotic treatment for a specific indication to be dispensed in one prescription for short courses of treatment
- inclusion of an administrative note that no repeats or increases in maximum quantity are allowed, thereby maintaining access for indications not listed in Therapeutic Guidelines.
In January 2021, the cautionary advisory label attached by Australian pharmacists to antibiotic packaging was changed to state, ‘Take for the number of days advised by your prescriber’. Previously the label advised patients to continue taking the antibiotics until they were all finished, which may have contributed to the excessive use of antibiotics.14
Pack sizes can have an impact on appropriate antibiotic use. A Croatian study comparing marketed antibiotic package size for treatment of sore throat and urinary tract infections with three international guidelines (Intersectoral Society for Antibiotic Resistance Control, National Institute for Health and Care Excellence, and The Infectious Diseases Society of America) found poor concordance of antibiotic package size with treatment recommendation duration.15 In Australia, trimethoprim 300 mg per night for three days or nitrofurantoin 100 mg six-hourly for five days are the first-line treatments for uncomplicated urinary tract infection for non-pregnant women.6 However, the currently available pack sizes for trimethoprim and nitrofurantoin contain enough tablets for seven days. This can result in increased treatment duration or unused antibiotics, which may be used subsequently by patients. While it is possible to request pharmacists to break packs, alignment of pack sizes to recommended treatment duration would be optimal.
Additional regulatory strategies that may optimise antibiotic stewardship include ensuring all prescribers have access to guidelines, restriction of antibiotic prescribing that is consistent with guidelines, and working with manufacturers to align pack sizes with indication where there is international consensus on dose and treatment duration.
Policy: Externally administered interventions
Some national programs of coordinated interventions have been used in efforts to decrease antibiotic use in primary care. No single intervention strategy is sufficient, and programs should ideally be sustained over the long term.
The selection of intervention combinations should be based on known barriers and enablers to changing behaviours informed by evidence-based implementation frameworks (ie Theoretical Domains Framework and behaviour change techniques).16
Audit and feedback
Audits of practice and feedback to clinicians is a fundamental quality improvement activity, but the impact on improving patient care can vary depending on the characteristics of the feedback and the nature of the targeted behaviour change. The process of audit and feedback is more effective when it is delivered by a credible source, repeatedly, using multiple formats and providing explicit targets and an action plan.17,18
NPS MedicineWise has been providing feedback to GPs on their prescribing and test ordering for a range of therapeutic areas for over 20 years, including a periodic focus on antibiotics. The Prescribing Practice Review provides graphical personalised and confidential feedback to all GPs in Australia on how their prescribing of selected PBS medicines for a therapeutic area (eg antibiotic for upper respiratory tract infections [URTIs]) compares with other GPs in the same Rural, Remote and Metropolitan Areas (RRMA) classification.19 The feedback is provided with points of reflection adjacent to the data. The most recent PBS feedback reports were on antibiotic prescribing in 2015 and urine microscopy, culture and sensitivity testing in 2017. Evaluation of a program of interventions, including audit and feedback along with academic detailing and other interventions, estimated a reduction of 18.4% of all antibiotics prescribed by GPs and dispensed under the PBS between 2012 and 2017.20
The MedicineInsight program includes more than 650 participating general practices across Australia, with more than 2500 GPs, representing more than 2.5 million patients. The program provides practice-level reports to support practice-led quality improvement. Real-time data are collected regularly, analysed and reported to practices to provide insight into a range of clinical indicators grouped under specific conditions, including indication for an antimicrobial prescription. The reports can also be presented to practices by an NPS MedicineWise educational facilitator in a whole-of-practice meeting.
Letters to high prescribers
A variant of audit and feedback was undertaken by the Department of Health’s Behavioural Economics and Research Team in 2017. Letters were sent by the Australian Government’s Chief Medical Officer targeting GPs with the highest antibiotic prescribing rates (top 30%). Letters with different presentations of prescribing data were tested in a randomised controlled trial. The best performing letter – which used peer comparison with graphic – reduced prescription rates by 12.4% over the six-month period and 9.4% over 12 months.21
Educational visiting
Australia is the only country with regular national educational visiting programs for general practice. The programs are provided by NPS MedicineWise, are available to any GP and cover a range of priority topics on quality use of medicines. There are generally two different programs per year; however, the last educational visiting program that focused on antibiotics was in 2012/13 – more than 9200 GPs participated.20
The academic detailing approach is based on the principles of social marketing and adult learning. The trained educational visitor is from outside the practice setting but meets with GPs in their practices either in person or virtually. This can be done on a one-to-one basis or as a small group. The content and approach in the visit are based on previously identified barriers to change, and delivery is tailored to the needs of the individual. The information discussed may include visual/graphical representations of evidence, practice data and case studies.
Public awareness and education campaigns
Whether or not an antibiotic is prescribed is partly driven by the patient’s expectations in a consultation with a GP, as well as by the prescriber’s perceived expectation of the patient. Sometimes these are not matched – prescribers can overestimate consumer expectations of receiving an antibiotic and might go too far in meeting those expectations.22,23
Public education is one essential component of antibiotic stewardship that can raise awareness of antimicrobial resistance (AMR) and reduce consumer demand for antibiotics (Figure 1). In Australia, public health campaigns have sought to improve understanding of: 1) how AMR is driven by overuse of antibiotics and how that affects individuals as well as the community, 2) the low benefit and potential harm from using antibiotics for low-risk and limited-duration conditions, 3) the natural history of URTIs and 4) when the illness is serious and when they should seek further medical attention.
Public campaigns are best combined with the availability of patient resources to be used during consultations with health professionals.22
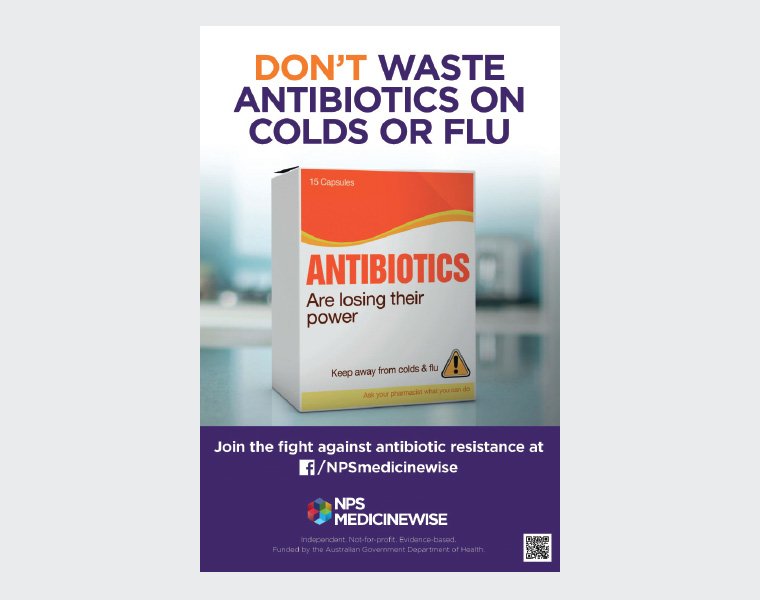
Figure 1. An example of media campaign materials for public awareness
Clinical: Activities that general practitioners can individually implement
What can we, as GPs, do to improve antibiotic prescribing when overloaded by short consultations and faced with patients who appear to just want an antibiotic prescription? Fortunately, there has been considerable research internationally to examine and compare different strategies. These clinical strategies are described more fully in another article in this issue of Australian Journal of General Practice,24 but their effects are shown in Table 1 and described briefly here.
| Table 1. Policy and clinical strategies, and their potential for reduced antibiotic usage |
| Regulatory strategies |
| Strategies |
Current responses and recommendation |
Limiting repeat courses of antibiotics
|
New Authority Required listings for repeat antibiotic prescriptions in line with Therapeutic Guidelines6 |
| Appropriate pack size for the correct number of antibiotics prescribed |
Align pack sizes to recommended treatment duration |
| Increase appropriateness of prescribing consistent with guidelines |
Ensuring all prescribers have access to guidelines, restriction of antibiotic prescribing that is consistent with guidelines and working with manufacturers to align pack sizes with indication where there is international consensus on dose and treatment duration |
| Policy strategies |
| Strategy |
Description |
Effectiveness
(reduction in antibiotics) |
Uptake/reach29,30 |
Comments |
| Audit and feedback letter |
CMO letter to highest 30% of GP prescribers21 |
8.4–9.4% reduction over 12 months |
30% (high prescribers) |
|
| Academic detailing |
NPS MedicineWise runs visiting programs (last in 2012–13) as part of a multifaceted program including PBS feedback reports20 |
18.4% reduction over five years for all GP prescribers for all interventions including academic detailing |
>9000 GPs received visit
|
All GPs received PBS feedback report |
| Media campaigns |
NPS MedicineWise has previously run intermittent media campaigns for consumers integrated with prescriber activities31 |
Unclear impact on antibiotic use
|
National |
Integrated nationwide prescriber and consumer program associated with modest but consistent positive changes in consumer awareness, beliefs, attitudes and behaviour to the appropriate use of antibiotics for upper respiratory tract infections |
| Clinical strategies |
| Strategy |
Description |
Effectiveness
(reduction in antibiotics) |
Uptake/reach29,30 |
Comments |
| Delayed prescribing |
Antibiotic script given as ‘wait and see’26 |
64% reduction |
72% always/often
20% occasionally |
Reduction depends on mode of ‘delay’ |
| Patient information sheets |
Handouts on symptom self- management and red flags32 |
47% |
20% always/often
27% occasionally |
For viral upper respiratory tract infection and bronchitis |
| Shared decision making |
Decision aid showing benefits and harms of antibiotics22 |
39% |
N/A |
For otitis media, sore throat |
| Clinical prediction rules |
feverPAIN rule predicting strep25 |
29% |
N/A |
For sore throat only |
| Near-patient testing |
C-reactive protein, procalcitonin and strep test kit29 |
21–61% |
18% for pharyngitis or ‘flu |
Cost of tests not covered by MBS |
| ‘NUDGE’ poster in practice |
Practice display of poster signed by GPs33 |
19% reduction in inappropriate antibiotics |
Uncommon |
Only one trial done (in USA) |
| Voluntary audit and feedback |
Prescribing data compared to others |
|
10% have done some time and received feedback |
Note: lower than CMO letter and NPS MedicineWise reach |
| Computer decision support |
Automated into GP electronic medical software34 |
Variable
Choice and duration of antibiotics improved |
Uncommon |
Under active investigation; 88% of GPs wanted better integration30 |
| CMO, Chief Medical Officer; GP, general practitioner; MBS, Medicare Benefits Schedule; N/A, not available; PBS, Pharmaceutical Benefits Scheme |
The first hurdle is to distinguish those patients who clearly need antibiotics from those who do not. Some clinical prediction rules, such as the ‘sore throat’ rules25 or near-patient testing – such as strep test kits, near-patient C-reactive protein, or procalcitonin – can help. However, using such near-patient tests may be unnecessary for most self-limiting URTIs and may be counter-productive. In addition, these aids often leave a large ‘grey zone’ of clinical uncertainty, where delayed prescribing and/or shared decision making can help. Delayed prescribing of antibiotics is probably the single simplest and most effective strategy, as only approximately one-third of patients given a delayed script end up using it.26
For patients who do not need an antibiotic, such as those with a simple viral URTI or uncomplicated bronchitis, an information handout provides a useful alternative ‘prescription’ that also reduces antibiotic usage.
These clinical strategies require some skill development, practice and the needed materials. Comparing notes with colleagues and having a practice policy and waiting room poster are also helpful, together with monitoring progress through audits of antibiotic usage.
Conclusion
While Australia has good regulation of antibiotic usage, and there have been some improvements in antibiotic stewardship, we have not had a sustained program.7 By contrast, Strama in Sweden has resulted in a steady reduction in antibiotic usage of approximately 7% per year.4 The Royal Australian College of General Practitioners (RACGP) position statement27,28 on antibiotic stewardship stated that ‘AMS programs … are currently underdeveloped in general practice, and will require a different approach from hospital-based antimicrobial initiatives. Specific resourcing is needed to develop AMS programs for primary care’. This will require a nationally coordinated program that provides for appropriate local resources in surveillance, quality improvement, training, consumer information and research (Box 1).
| Box 1. Recommendations to improve antibiotic stewardship in primary care |
A comprehensive, coordinated and effective surveillance of antimicrobial resistance and antibiotic use in primary care including: 1) usage, 2) antibiotic resistance, 3) patient safety indicators such as mastoiditis and quinsy rates, which may be avoidable with appropriate antibiotic use and 4) antibiotic stewardship activities that can be implemented in practice.
Regularly provide information for consumers to raise awareness of antibiotic resistance to reduce patient demand for antibiotics for upper respiratory tract infections in consultations with general practitioners (GPs).
Support training for general practice registrars and all GPs in antibiotic stewardship.
Support a regular audit and peer feedback program for all GPs.
Develop better mechanisms to ensure ready access by GPs to consumer materials and self-management resources at the point of consultation.
Invest in research into the above programs, including rigorous evaluations of their impact to inform further program direction and content. |
In the face of an impending antibiotic crisis,21 the Australian healthcare systems would be wise to invest in sustained stewardship programs on the basis of the above recommendations. Of course, there are unanswered questions, and the stewardship program should include a research and evaluation element. Meanwhile, there are many means for individual GPs to improve their own practice. GPs are also powerful advocates for helping colleagues and health system funders to support a national effort.