Case
A woman aged 36 years who worked as an accountant presented to her general practitioner (GP) because of an episode two days prior of sudden-onset vertigo, left ear tinnitus, right arm numbness and weakness, difficulty speaking and headache. With the exception of the headache, all symptoms receded within thirty minutes. She had a history of mild dyslipidaemia, controlled with lifestyle modification; was a non-smoker; and reported a nine-hour flight four days prior. Her father had a myocardial infarction at the age of 58 years. She did not recall signs or symptoms suggestive of deep vein thrombosis and did not satisfy any Wells criteria. Vital signs were normal. Neurological examination disclosed a positive Romberg test, normal Weber and Rinne tests, and no other neurological deficits. Heart sounds were dual with no murmurs. The patient’s primary concern was that this episode would affect her plans for pregnancy in the near future. She had no children and no past pregnancies.
While best practice recommends urgent referral of such cases to an appropriate stroke unit for inpatient work-up, after consultation with a multidisciplinary team and because of a serendipitous immediate availability, a logistical decision was made on the radiologist’s recommendation to urgently order magnetic resonance imaging/magnetic resonance angiography. A verbal report was obtained within hours, with results showing a subacute infarct of the superior right cerebellum (Figure 1). The patient was immediately referred to emergency and admitted under neurology on the same day, where she underwent a thorough young stroke work-up, including vasculitic and thrombophilic screens, computed tomography angiography and echocardiography, each revealing no abnormalities. The D-dimer blood test was within the normal range. Transoesophageal echocardiography (TOE) revealed a patent foramen ovale (PFO) with a mobile interatrial septum and a right-to-left shunt identified on colour Doppler and agitated saline bubble study (Figures 2 and 3). No appendage thrombus was visualised on TOE. The patient was commenced on aspirin 100 mg daily as routine secondary prevention and atorvastatin 20 mg daily for her dyslipidaemia. Closure of the PFO to reduce risk of recurrent stroke was discussed. She was discharged for regular review with her GP to monitor cholesterol levels and tolerance of the statin.
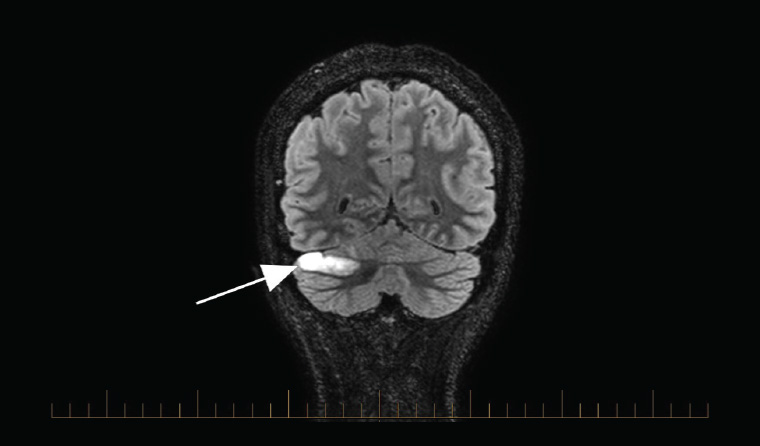
Figure 1. Coronal T2-weighted fluid-attenuated inversion recovery (FLAIR) magnetic resonance imaging demonstrating superior right cerebellar infarct (white arrow)
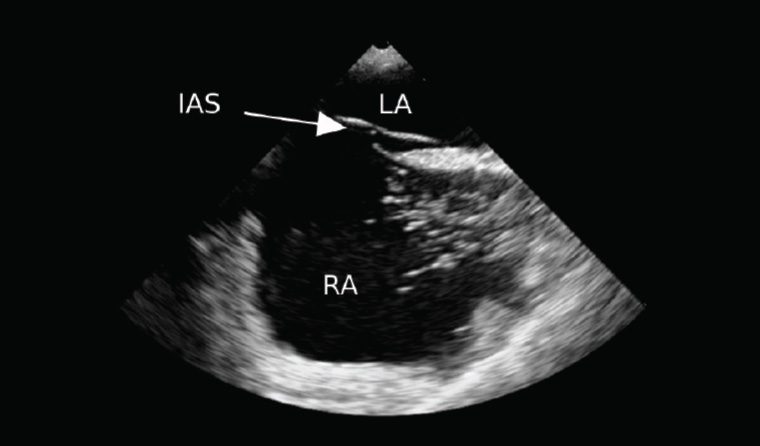
Figure 2. Transoesophageal echocardiography short-axis view prior to filling by agitated saline
IAS, interatrial septum; LA, left atrium; RA, right atrium
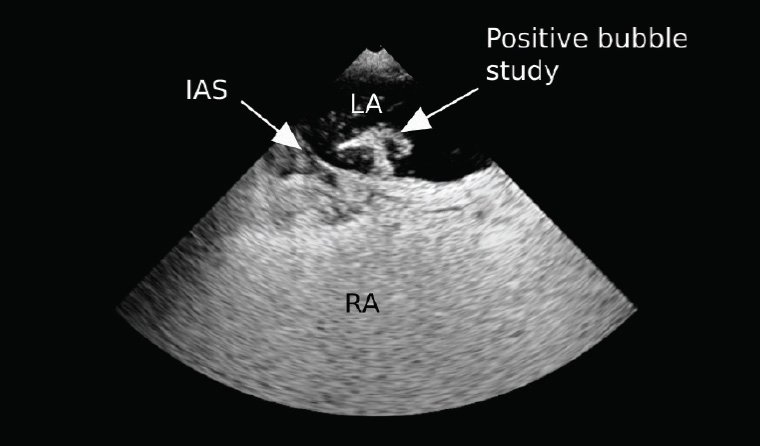
Figure 3. Transoesophageal echocardiography short-axis view after filling by agitated saline, demonstrating positive right-to-left shunt (white arrow labelled ‘Positive bubble study’)
IAS, interatrial septum; LA, left atrium; RA, right atrium
Question 1
What is the incidence and prevalence of PFO? How is it implicated in this patient’s cryptogenic stroke?
Question 2
What is a risk of paradoxical embolism (RoPE) score?
Answer 1
PFOs are very common and are present in up to 25% of adults, although this number reaches 50% in those with classical migraine.1 For adults aged 35–40 years, the incidence of PFO has been measured to be 17%.1 In the absence of significant vascular disease, atrial fibrillation, structural heart disease or thrombotic diathesis, the cryptogenic stroke is most likely due to an embolic event associated with the patient’s PFO. The PFO can disturb blood flow, forming thrombi that may embolise, or can act as a conduit for the migration of a venous embolus into the left atrium, with subsequent systemic embolisation.1 The presence of a hypermobile atrial septum further increases the risk of recurrent strokes.2 An estimated 10% of all ischaemic strokes in young patients aged <55 years are attributable to a PFO, although the incidence of ischaemic stroke in young patients remains low, affecting only eight per 100,000.3,4 However, PFO remains an important aetiology to consider in cases of cryptogenic stroke, responsible for 42% of cryptogenic strokes in patients aged ≤55 years and 15% in patients aged >55 years.3
Answer 2
While PFO is a common cause of cryptogenic stroke, there remains the possibility that a PFO discovered on stroke evaluation is an incidental finding. The RoPE score is a 10-point scale used to determine the risk of a PFO being pathogenic in a cryptogenic stroke, and it can also estimate the risk of stroke recurrence in the following two years.5 The RoPE score is outlined in Tables 1 and 2.5
| Table 1. Risk of paradoxical embolism (RoPE) score calculator |
| Patient characteristic |
Points |
| No history of hypertension |
+1 |
| No history of diabetes |
+1 |
| No history of stroke or transient ischaemic attack |
+1 |
| Non-smoker |
+1 |
| Cortical infarct on imaging |
+1 |
| Age (years) |
|
| 18–29 |
+5 |
| 30–39 |
+4 |
| 40–49 |
+3 |
| 50–59 |
+2 |
| 60–69 |
+1 |
| ≥70 |
0 |
| The RoPE score is calculated on the basis of clinical features of the patient’s presentation.5 |
| Table 2. Patent foramen ovale (PFO)–attributable fraction and estimated two-year stroke recurrence risk by risk of paradoxical embolism (RoPE) score strata |
| RoPE score |
PFO-attributable fraction (%) |
Estimated two-year recurrence risk (%) |
| 0–3 |
0 |
20 |
| 4 |
38 |
12 |
| 5 |
34 |
7 |
| 6 |
62 |
8 |
| 7 |
72 |
6 |
| 8 |
84 |
6 |
| 9–10 |
88 |
2 |
Case continued
The patient had a RoPE score of 9, indicating that the risk of the stroke being attributable to her PFO was 88%, with a 2% risk of recurrent cryptogenic stroke in the next two years.
The patient underwent non-urgent PFO closure, with continued aspirin therapy and instructions for antibiotic prophylaxis in the event of dental work or surgery. Both the aspirin and antibiotic prophylaxis could safely be ceased six months post procedure. Her statin was ceased six months later, on account of her plans to fall pregnant. Over a year later, she returned for regular cardiology review with no issues and reported returning almost completely to baseline neurological function.
Question 3
How could a PFO affect pregnancy, had it remained undetected?
Answer 3
It is likely that the hypercoagulable state during pregnancy would further increase the risk of PFO-related complications.6 One review showed that in pregnant patients with stroke, presence of a PFO was associated with a higher National Institutes of Health Stroke Scale score.7 However, despite the higher risk of stroke, the majority of these patients with PFO-associated stroke had good neurological outcomes and uneventful deliveries of healthy newborns. For women presenting with stroke in pregnancy, the finding of a PFO would be an indication for anticoagulation.8 PFO closure during pregnancy is not routinely recommended, although several case reports show it can be performed with trivial radiation exposure as an alternative to anticoagulation.9,10
Key points
- In a young, healthy patient with a cryptogenic stroke, it is important to consider investigations for a PFO.
- Many PFOs remain asymptomatic throughout adulthood.
- The RoPE score can provide insight into whether a PFO discovered on cryptogenic stroke work-up was pathogenic.
- The presence of a PFO during pregnancy is of concern and may warrant cardiologist assessment.