More than 20% of Australian children are ‘developmentally vulnerable’ at school entry, with higher rates among disadvantaged groups.1 Neurodevelopmental disorders are also common, with the childhood prevalence of autism spectrum disorder (ASD) now estimated to be one in 59.2 These figures are of concern, both at individual and public health levels, given the known trajectories towards behavioural, psychosocial and educational problems throughout early childhood, and compromised health, education and social outcomes in adulthood.3,4
Given the prevalence and negative outcomes of developmental and neurodevelopmental concerns,1 and the known benefits of early intervention, childhood developmental surveillance is best practice.5 Defined as a ‘flexible, continuous process whereby knowledgeable professionals perform skilled observations of children during the provision of healthcare’,6 developmental surveillance integrates developmental screening test results within a broader picture of a child’s life, including information from medical history, current physical examination, parent input and clinician observations.7 In practice, however, developmental surveillance opportunities are often missed due to limited uptake of voluntary surveillance programs in primary care.8 Children from culturally and linguistically diverse (CALD) and socioeconomically disadvantaged backgrounds are at highest risk, and often miss opportunities for early intervention.9
General practitioners (GPs) are usually the first point of contact for families accessing services in the healthcare system,10 and barriers to developmental surveillance in primary care can include constraints on time, knowledge and/or self-efficacy with child assessment.11 Some international initiatives have increased developmental surveillance within primary care,11,12 but there have been challenges with uptake, referral pathways, and workflow procedures.8 There is a need to develop innovative approaches to promote developmental surveillance.
Advances in information technology and internet accessibility provide new opportunities to improve healthcare in the child health domain.13 Developmental surveillance/screening eHealth approaches have included apps/websites with parent-reported screening questionnaires for autism and/or developmental concerns and in-built algorithms to identify children deemed at risk;14,15 and parent-reported screening questions, with clinician review of uploaded video-taped screening data or follow-up interview.16,17 While some apps incorporate guidance and educational material for parents,18 many focus solely on screening, with few specifically developed for use within a developmental surveillance framework, and few that are evidence based and tested.
WMG-E is an online resource developed in Australia. It enhances the capacity of community-based clinicians to involve parents in monitoring their child’s development. It incorporates the ‘Learn the Signs. Act Early’ red flag items to monitor general development,19 and the quantitative checklist for autism in toddlers to monitor for symptoms of autism (Q-Chat).20 Other components include an algorithm-based guide for clinician recommendations regarding assessment and referral pathways, anticipatory guidance for parents about age-appropriate developmental milestones and measures to enhance healthy development, and electronic parent reminders for parents (to repeat the WMG-E questions six monthly, until the child is five years of age). WMG-E is designed to be brief and user friendly, thus enabling parents to regularly monitor their children’s development, and is envisaged to be used by parents opportunistically in the waiting room of a primary care service. For instance, if undertaken immediately prior to a healthy child check or a childhood immunisation visit, there will be opportunities for immediate discussion and action by the primary care clinician. WMG-E was developed by members of the study team as a freely available resource, at no cost to consumers or health professionals.
The aim of this study was to explore the perspectives that clinicians and parents had about how well WMG-E measures what it purports to measure (‘face validity’). It sought to explore and describe clinician and parent perceptions of its suitability, feasibility and accessibility.
Methods
Study design
This study used an inductive thematic analysis approach, which meant that themes were identified from surface-level data (or in other words, what the participants said) rather than using a predetermined theory, framework or structure.21 Within this broader approach, a contextualist method was used, allowing for consideration of both the meanings that participants gave to their experiences as well as the social contexts that may have impinged on these meanings.21
Context
The study was conducted in 2018 in South Western Sydney Local Health District, a large, highly populated region of Sydney, Australia. The region is highly ethnically diverse, and home to some of the country’s most vulnerable populations (eg higher than average levels of unemployment and disabilities).22
Participants and sampling strategy
Participants included parents (n = 6), GPs (n = 3), paediatricians (n = 3), and child and family health nurses (CFHNs; n = 25). For demographics, refer to Table 1. A convenience sampling method23 was used to recruit participants. Specifically, local GPs and paediatricians known to have expertise or interest in childhood development were contacted via email and invited to participate in a semi-structured interview. Teams of CFHNs in the local area were invited to participate in facilitator-led group discussions (‘focus groups’) during the allocated time slots of their regular team meeting. Parents were recruited from a residential early parenting service providing a four-night residential program for infant sleep and settling issues. All English-speaking parents attending the service within the study time frame who had a child in the given age range were approached in person by one of the study authors (JV) and invited to participate in a semi-structured interview.
| Table 1. Sample demographic characteristics |
| Variable |
Clinicians |
Parents |
| |
Mean (SD, range) |
Mean (SD, range) |
| Age (years) |
50.6 (8.4, 39–67) |
26.9 (4.9, 19–33) |
| Child age (months) |
– |
29.3 (1.1, 28–31) |
| Years of professional experience in early childhood healthcare sector |
13.6 (7.1, 3–27) |
– |
| |
% |
% |
| Female |
85 |
100 |
| Cultural background |
| Australian |
26 |
80 |
| Asian |
33.8 |
20 |
| African |
11.1 |
0 |
| European/British/American |
29.6 |
0 |
| Education |
| High school |
7.7 |
50.0 |
| University or higher |
92.3 |
50.0 |
| Target child first born |
– |
50.0 |
| SD, standard deviation |
Data collection
A study author (JV) conducted semi-structured interviews (30–60 minutes) with clinicians at their practice location and with parents at the parenting service. The semi-structured interview format comprised open-ended questions that invited the interviewee to engage in discussion with the interviewer. Each focus group (60 minutes) was co-facilitated by two of three study authors (JV, JK, AD), with four to 10 participants in each group, held at the health services where the clinicians were based. A schedule of questions guided both the interviews and focus groups, with probing questions used to invite participants to explicate their responses. The questions, shown in Box 1, were designed to engage participants in a discussion about WMG-E (usability, convenience, whether fit for purpose) and facilitate discussion about how WMG-E might aid developmental surveillance. All participants accessed the WMG-E app prior, including completing the questions contained in it (with an imaginary child in mind).
| Box 1. Semi-structured interview and focus group questions |
- Can you describe what services are available in your local area to screen/check children’s developmental health and wellbeing?
- For parents only: Have you accessed any of these services? How did you find them?
- What do you think about the look/presentation of the WMG-E app?
- Can you comment on the WMG-E questions (eg relevance, language, content)?
- What did you find useful in the parenting/developmental information provided to parents in the WMG-E?
- Is there anything that could improve the WMG-E?
- What do you think about the way the WMG-E app provides feedback to parents?
- Imagine that you were in a general practitioner’s office and you were expected to complete this app. What do you perceive as the potential barriers to you/other parents using the WMG-E app? What do you think would assist or facilitate you/other parents in using the WMG-E app?
- For health professionals only: What do you think about the referral guidelines/information provided by the WMG-E app?
|
| WMG-E, Watch Me Grow – Electronic |
Data analysis
Interviews and focus groups were recorded and transcribed verbatim. Data analysis was conducted in four sequential steps. First, three study authors (JK, AD, VG; clinical psychologist, psychologist, social health researcher) analysed the transcripts line by line to apply initial codes and identify themes. They then met as a group to discuss, refine and name the identified themes (step 1). Five additional co-authors (CT, SW, NO, MP, AM; expertise in early childhood nursing, paediatrics and general practice) engaged in a second round of data coding (step 2; same procedure as for step 1). The first three authors then reviewed the transcripts to extract quotes that best reflected the identified themes (step 3). Finally, extracted quotes were collated by one study author (JV) and then reviewed by the other coders to ensure consensus (step 4).
Ethical approval
The study was approved by South Western Sydney Local Health District Human Research Ethics Committee (SWSLHD HREC), project approval number HREC/17/LPOOL/150.
Results
Participants were collectively receptive of WMG-E. They spoke of its user friendliness and its potential to promote developmental surveillance in primary care:
They were good questions; easy to understand; easy to relate to. [Parent #1]
This is a good way to increase the uptake [of developmental surveillance] as they are all into technology now, on their phones and they all love their apps so and they do it. [Clinician, focus group #2]
In addition to positive general feedback, three key themes emerged: (dis)empowerment; seizing opportunities at all levels; and balancing universalism with specificity (Figure 1). These themes reveal both the perceived benefits of WMG-E and factors to consider before implementation.
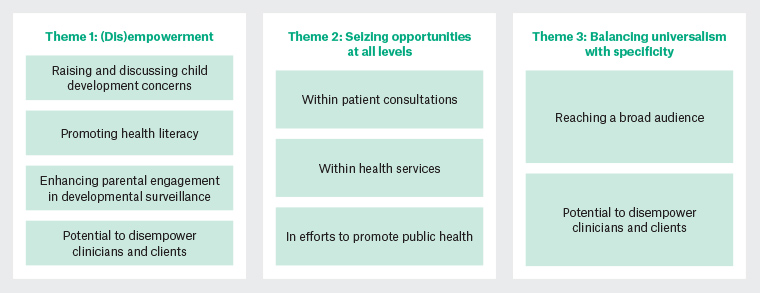
Figure 1. Themes and sub-themes
(Dis)empowerment
Both clinicians and parents commented that WMG-E might empower clinicians and parents. Many recognised that the resource would enable both parties to raise and discuss child development concerns. Furthermore, a personalised outcome summary might encourage parents to perceive a greater sense of control to direct the care their child received:
The parent might walk in and say, ‘It is great that this … has been done … I am really worried about my child’s eye contact. He is not yet responding; he is not yet following instructions’, and then the GP would say, ‘Alright, yes, looks like there are issues here and I will give you a referral to this paediatrician’ … These results … initiate a conversation. [Clinician #3, interview]
Participants agreed that information on normal child development, which is offered at the end of WMG-E completion, promoted health literacy. The ease of access and the opportunity to share information with others made it convenient:
I’d like to read that, just to make sure that he is ticking all those things that it … I could just forward that email to my husband or to someone else … that would be really good. [Parent #4]
Most participants identified the need for health services to adapt to the current trends and valued the convenience of technology. Several noted that WMG-E could motivate and increase parental engagement in ongoing developmental surveillance.
I forget about things like this … So, when I get the email, it’s just a reminder that maybe I should go and have another look. [Parent #1]
However, some participants advised that WMG-E could disempower clinicians:
It is disempowering the GP … By saying… ‘It is strongly recommended that referral for further assessment and early intervention through paediatrician or other child health professional is done’, you are not asking them, ‘What do you think?’ You should ask them, ‘Please do a check from the developmental perspective of child and suss out more issues and then arrange appropriate referral’. [Clinician #3, interview]
Others indicated that WMG-E might disempower clients, particularly those from disadvantaged groups, such as parents with an intellectual disability, those from a CALD background, or those of low socioeconomic status:
We’ve got to think about the kind of people that’s going to use this … Most of our ladies with the intellectual delay or in low socioeconomic areas… keep telling me… ‘Don’t tell me about stuff on the internet’; they don’t have data on their phone. [Clinician, focus group #1]
If English wasn’t necessarily your first language and somebody just asked you to go over there and do this particular app, it could become difficult. [Parent #1]
Seizing opportunities at all levels
According to participants, WMG-E would need to be introduced and sustained in a strategic and purposeful way. Opportunities could be seized at a number of different levels, including within the confines of patient consultation; within a health service; and, more broadly, during efforts to promote public health.
At the level of the patient consultation, participants noted that, if used effectively, WMG-E could prompt parent–clinician discussion, thus encouraging (at least some) parents to seek healthcare:
There’s always times that you forget to ask … So, if they read through [the WMG-E results] … they could say, ‘Oh look, I’ve noticed this’… and then you can discuss it. [Parent #5]
At the health service level, participants indicated that WMG-E usability could be improved if implementation was accompanied by strategic health promotion efforts. Many considered regular immunisation checks and waiting areas as great avenues for this. Additionally, participants commented that if WMG-E was encouraged by a whole service, it could enhance user acceptability:
The waiting room [offers] … a lot of opportunities that we can harness … [as the] waiting period is generally wasted … [Clinician #1, interview]
Some participants recognised the complexities of working within health services and suggested that appropriate systems are needed to support the implementation and use of WMG-E:
My worry is, when are we gonna look at emails; how much time are we gonna look at the emails; how much time are we gonna have to assess the emails and then book the client in and then follow them up? [Clinician, focus group #1]
At the broader, public health level, participants suggested it would be helpful to align the introduction of WMG-E with government initiatives such as the National Disability Insurance Scheme (NDIS):
Once … the GP makes a call that this child has significant developmental delays, he can … provide … early intervention … through the NDIS. This is an ideal time for this work with the NDIS rollout. [Clinician #3, interview]
Two participants stressed the importance of universal systems of developmental surveillance. Cognisant of the complexities involved in implementing a WMG-E universal system, another suggested that the endorsement of a regulatory body could be a significant strategic move:
If it is part of the accreditation of practices, why would it be a barrier? ... The practice would actually vie for it; they would say, ‘Yep, this is fantastic; it’s our mandatory requirement’. [Clinician #3, interview]
Yet several participants acknowledged that the universal implementation of WMG-E is unattainable without an awareness campaign and improved electronic systems:
Having an education rollout … educating the doctors as well as the public. [Clinician #5, interview]
Balancing universalism with specificity
Participant comments indicated that the value of WMG-E is likely to be aided by its capacity to balance universalism and specificity – that is, its capacity to reach a broad audience while also having perceived relevance to individuals. Several clinicians and parents advised that while the WMG-E would have universal appeal and accessibility, they particularly valued the customised approach. The app’s personalised commentary on the specific child’s development would help parents to relate to the content, find meaning in it and potentially alleviate anxiety:
I was a parent who was worried that bit [advice on when to speak further with a health professional] would be helpful for me. [Parent #1]
Others, however, reported that the advice provided at the end of the WMG-E app to ‘speak further with a health professional’ might in fact increase parental anxiety:
I was thinking my child was completely normal; so, now I’m freaking out because I was thinking they were normal, and it hasn’t told me where the deficits are that I then could be working on, as a … highly anxious mother. [Clinician, focus group #1]
Discussion
This study suggests that WMG-E holds promise as an online resource to enhance parental and clinician engagement in developmental surveillance. To enhance viability and efficacy, however, results suggest that three major issues should be considered prior to implementation in primary healthcare settings.
First, although WMG-E could empower clinicians and parents, participants highlighted the importance of following established recommendations about developmental surveillance.7 That is, clinicians should use information from WMG-E in combination with clinical observations and their understanding of the context of the child to make decisions about access to further supports and interventions. For this, appropriate training and suitable care pathways are important. Without such support, WMG-E might be disempowering for clinicians. The potential for WMG-E to disempower parents was also raised, particularly for families from CALD backgrounds. Future work should translate WMG-E into commonly spoken languages, to increase accessibility for families from CALD backgrounds.
Second, participants advised that WMG-E should be implemented strategically at the levels of the patient–clinician consultation, the primary healthcare practice, and more broadly of public health policy. This could be conceptualised within Bronfenbrenner’s24 ecological systems theory framework. That is, the WMG-E app should be implemented in such a way that it enhances opportunities for individuals at a micro level – for example, so that parental awareness of childhood development is enhanced and both clinicians and parents are empowered to engage in developmental surveillance. At a meso level, health services would need to make use of WMG-E in a way that facilitates uptake for families – for example, implementing it opportunistically in the waiting room prior to well-baby checks. Finally, at the macro level, WMG-E needs to be aligned with policies that support developmental surveillance and are duly connected with related initiatives such as the NDIS.
Third, participants recognised a need to balance widespread appeal with perceived relevance. Although opportunistic use of WMG-E during planned clinic visits (eg a healthy child check or childhood immunisation visits) was identified as an acceptable option, participants felt that it would be important to customise information for individual recipients and provide additional support for families when required. There were mixed views, for example, on whether the app would alleviate or exacerbate parental anxiety about child development concerns. As discussed above, it is vital that WMG-E is used within the developmental surveillance framework within which it was designed, as is the role of the health professional in using WMG-E to start conversations and work with parents to track and support healthy child development. Future work should investigate whether it is possible to use WMG-E within a ‘proportionate universalism’ framework, combining universal coverage with targeted approaches commensurate with need.25
This study had a number of strengths including use of a sample that was ethnically diverse, professionally varied, and which included both parent and clinician perspectives. It was only the clinicians who commented about strategic implementation at health service and policy levels, but there was a general agreement between parents and clinicians about the other identified themes. Despite these strengths, various limitations warrant mention.
First, convenience sampling meant that most clinicians had expertise or an interest in child health, which may have led to biased results. Future studies should seek to recruit a more representative sample of clinicians by using a random sampling approach. Similarly, all of the parents in the study were recruited from a residential parenting service and so were, by definition, struggling with an aspect of parenting, which may have impacted their perceptions of WMG-E. It is also possible that having sought health service support, these parents may in fact be a more motivated group of parents, which again may have influenced their opinions about WMG-E. It is also noted that data was collected from parents via one-on-one interviews and it is possible that a focus-group format may have resulted in richer discussion and reflection from these participants. The failure to include non–English speaking parents in the study is a further limitation, particularly given the CALD nature of the study setting. Future studies should use interpreters to garner perceptions from parents from CALD backgrounds.
Second, the number of parents interviewed was small (n = 5), and while saturation was reached by the fifth interview, further research conducted with a larger and more diverse sample of parents would be worthwhile. The number of clinicians included in the study was also low, and future work would benefit from larger samples to ensure diversity of perspectives and true data saturation.
Third, the study was conducted in one region of Sydney, and so applicability to wider Australia or internationally is unknown. Future work should examine perceptions of clinicians working in a more diverse range of geographical settings.
Conclusion
This study suggests that WMG-E may assist primary healthcare clinicians and parents to engage in developmental surveillance. The anticipatory guidance presented to parents about healthy development and the regular electronic reminders for ongoing surveillance may also empower parents to actively engage in better understanding and tracking their child’s development. Many positive outcomes may thus ensue from the use of WMG-E, including the quelling of parental anxiety, optimising healthy child development and reducing the risk that developmental vulnerabilities will cascade into a trajectory of life-long adverse outcomes. Future research should test the validity of the WMG-E as a screening tool for developmental issues in young children, and its effectiveness in promoting use of developmental surveillance in primary healthcare settings.