Case
A boy aged 11 years presented to his general practitioner with a two-day history of severe right groin pain and difficulty weight bearing. This occurred on the background of four weeks of mild, intermittent pain in the same region.
He could not recall an inciting event, had no history of hip pathology, and had not experienced similar symptoms previously. He was otherwise healthy, had no history of recent travel, and was fully immunised. His developmental history was unremarkable.
On examination, he had normal vital signs and was afebrile. He was on the 50th centile for height and the 90th centile for weight. He had an antalgic gait and held his right lower limb in an externally rotated posture. His hip was irritable with passive range of motion, particularly in flexion and internal rotation.
Question 1
What is the differential diagnosis?
Question 2
What investigations are indicated?
Answer 1
The most likely diagnosis is a slipped upper femoral epiphysis (SUFE), with other possibilities including Perthes’ disease, septic arthritis, peri-articular osteomyelitis, transient synovitis, tumours and occult fractures. Spinal, abdominal and pelvic pathology can also refer pain to the hip.
According to the Loder classification, SUFE can be classified as stable if the patient can weight bear, with or without aids, or unstable if they are unable to weight bear at all.1 Patients with stable SUFEs may present in the primary care setting, whereas patients with unstable SUFEs typically present directly to hospital via ambulance.2
In the absence of infective symptoms, an SUFE should be suspected in any child or prepubertal adolescent with groin, thigh or knee pain and altered gait, until proven otherwise. Perthes’ disease has a similar presentation but is more prevalent in younger children. In the presence of infective symptoms or signs, septic arthritis should be excluded.3
Answer 2
An antero-posterior (AP) pelvis and frog-leg lateral X-ray should be ordered to assess for bony pathology. Key radiographic features include displacement of the femoral epiphysis or physeal irregularity.
If there is clinical suspicion of a septic arthritis, serum inflammatory markers and joint ultrasonography should be ordered.
Magnetic resonance imaging (MRI) is occasionally used to detect physeal abnormalities where there is a high index of suspicion for SUFE, but X-rays are normal. MRI is also useful for investigating osteomyelitis and tumours.
Case continued
The patient was given crutches and advised not to weight bear on the painful hip. AP pelvis and frog-leg lateral X-ray views were obtained (Figure 1).
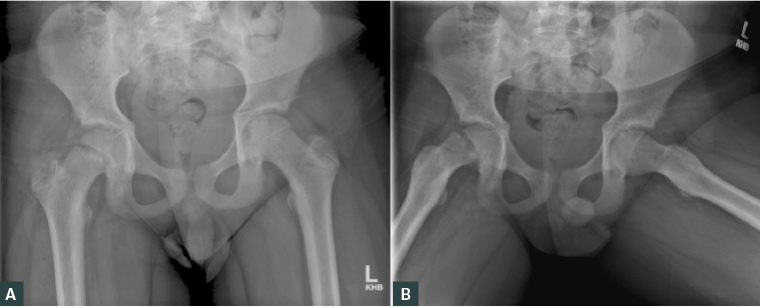
Figure 1. A. Antero-posterior pelvis X-ray; B. Frog-leg lateral X-ray
Question 3
What are the relevant radiographic findings?
Question 4
What is the recommended treatment for SUFE?
Answer 3
On an AP X-ray, a line drawn along the superior femoral neck (Klein’s line) should intersect the superolateral portion of the femoral head (Figure 2). On this child’s right hip, Klein’s line does not intersect the femoral head, consistent with an SUFE. Widening of the physis is also noted.
On a frog-leg lateral view, the Southwick slip angle can be measured between the axis of the femoral shaft and the epiphysis. Slip severity is considered mild when the angle is <30°, moderate when 30–50° and severe when >50°.4
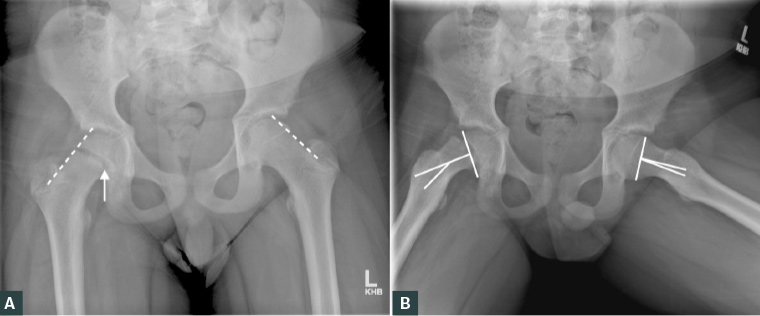
Figure 2. A. Antero-posterior pelvis X-ray demonstrating abnormal Klein’s line (dotted line) and widening of the physis on the right hip (solid arrow); B. Frog-leg lateral X-ray demonstrating an increased the Southwick slip angle (solid line)
Answer 4
To prevent further slippage, children with suspected or diagnosed SUFE should immediately be made non–weight bearing with crutches or a wheelchair.5 The local orthopaedic service should be contacted immediately, and the child referred to the emergency department unless otherwise instructed.
Surgery is required to prevent further slippage until eventual closure of the physis.4 In situ pinning of the hip using a single screw is considered the gold standard treatment. For an unstable or severe SUFE, a sub-capital realignment procedure may be considered in tertiary centres.
Prophylactic pinning of the contralateral hip may be recommended in patients with pain on the contralateral side, who are a young age at diagnosis, who are at risk of inadequate follow-up, or who have underlying endocrine disorders.4
Children with atypical SUFE (eg bilateral SUFE, age <10 or >16 years, height <10th centile or weight <50th centile) should be investigated for kidney disease and endocrine disorders, particularly hypothyroidism.6
Case continued
The patient was urgently referred to the local orthopaedic service. The affected hip was stabilised via in situ fixation, and the contralateral hip was prophylactically pinned (Figure 3).
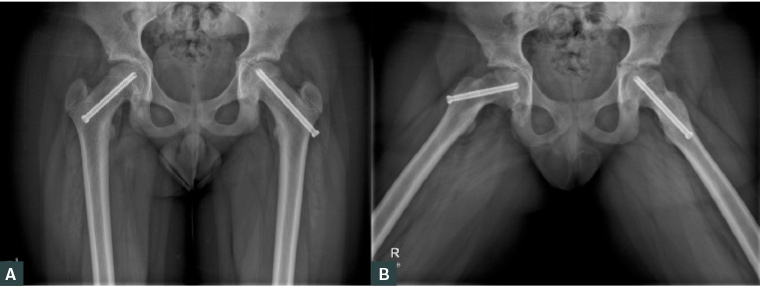
Figure 3. A. Antero-posterior pelvis X-ray; B. Frog-leg lateral X-ray demonstrating in situ fixation of the right slipped upper femoral epiphysis and prophylactic pinning of the left hip
Question 5
What is the prognosis of SUFE?
Answer 5
Provided there is early diagnosis and appropriate treatment, most patients experience good long-term clinical outcomes.7 Prognosis is principally dependent upon slip severity, associated with age at diagnosis, symptom duration and time to treatment.2,7–9 However, some literature suggests lower activity scores and persistent pain in approximately one-third of patients in the long term.10
Significant complications associated with SUFE include avascular necrosis, chondrolysis and femoroacetabular impingement.4,9,10 Reported rates of avascular necrosis are nearly 0% in patients with treated stable SUFE and 6–60% in patients with treated unstable SUFE.4
Key points
- SUFE should be suspected in any child or prepubertal adolescent presenting with a limp and groin, thigh or knee pain.
- Key investigations include an AP pelvis and frog-leg lateral X-ray.
- Patients should be made non–weight-bearing and urgently referred to their local orthopaedic service.