Case
A man aged 80 years presented with a one-day history of widespread tender skin lesions and malaise. He had a background of longstanding anti-N-methyl-D-aspartate receptor encephalitis that was managed with six-monthly rituximab and 5 mg of prednisone daily. He did not have any arthralgias, fevers or recent viral symptoms. Clinical examination revealed tender, nodular indurations over his chest and limbs, with sparing of his palms and plantar surfaces (Figure 1). The nodules were not ulcerating, discharging or weeping. He had no mouth ulcers. He was afebrile, and his observations were within normal limits. He was anaemic on presentation, with a haemoglobin of 99 g/L (reference range 130–170 g/L). His full blood examination and biochemistry were otherwise unremarkable.
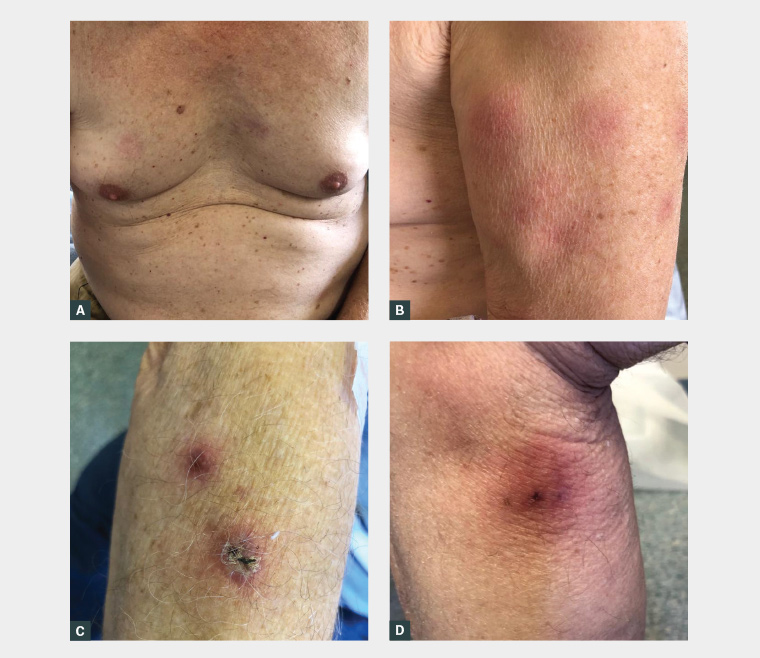
Figure 1. Photographs of the patient’s widespread tender skin lesions
A. Tender erythematous plaques on the upper chest; B. Multiple erythematous nodules on the bicep; C. Scaly and erythematous plaque on the forearm; D. Large erythematous nodule on the lower limb
An incisional biopsy of a lesion on his shoulder was performed, and this showed a predominantly septal panniculitis with neutrophilic infiltrates and no evidence of vasculitis. Periodic acid–Schiff (PAS), tissue culture and Gram stains for infections were unremarkable. At this stage, subcutaneous Sweet syndrome was suspected, and the patient’s regular oral prednisone was increased from 5 mg to 25 mg daily. He responded rapidly to the increased prednisone, with significant improvement of the lesions within a week and resolution within three weeks. A week after his initial presentation, his blood film showed dysplasia with promonocytes and a new thrombocytopenia. A bone marrow biopsy confirmed acute myeloid leukaemia (AML), and he was not offered treatment because of his age and comorbidities. The patient died shortly after his diagnosis in the context of febrile neutropenia.
Question 1
What is subcutaneous Sweet syndrome?
Question 2
What is the clinical importance of subcutaneous Sweet syndrome?
Question 3
How is subcutaneous Sweet syndrome diagnosed?
Question 4
How is subcutaneous Sweet syndrome managed?
Question 5
What are the other differential diagnoses?
Answer 1
Subcutaneous Sweet syndrome is an idiopathic neutrophilic dermatosis.1 It is characterised by tender erythematous plaques and nodules that tend to follow a symmetric distribution on the trunk and extremities.1,2 Other common clinical features of subcutaneous Sweet syndrome include fever and malaise.3 These clinical features are similar to those found in Sweet syndrome. However, the two syndromes are histologically distinct. In Sweet syndrome, neutrophilic infiltrate is found in the dermis and subcutaneous layers, whereas in subcutaneous Sweet syndrome, neutrophilic infiltrate is limited to the subcutaneous layer.1 Sweet syndrome is often idiopathic, but it can also be associated with malignancy, infection, pregnancy, autoimmune disorders and medications.2 In contrast, subcutaneous Sweet syndrome has a particularly strong association with haematological malignancies.
Answer 2
Subcutaneous Sweet syndrome is associated with haematological malignancies including AML, myelodysplastic syndrome and multiple myeloma.4 The presence of subcutaneous Sweet syndrome in patients with myelodysplastic syndromes is notably associated with a poor prognosis.5,6 This case report outlines an example of subcutaneous Sweet syndrome signalling the onset of AML, where the appearance of cutaneous lesions preceded the biochemical findings of myelodysplasia. There was a subsequent rapid progression of the patient’s AML. It is noteworthy that lesions often precede the diagnosis of malignancy in Sweet syndrome.2 It is therefore essential that a work-up for haematological malignancies be performed once a diagnosis of subcutaneous Sweet syndrome is established.
Answer 3
Histopathological confirmation is required to make a diagnosis of subcutaneous Sweet syndrome. Features include neutrophilic infiltrate that is limited only to the subcutaneous tissue, including either the lobules, septa or both, with no evidence of vasculitis.1,3 Other criteria that are found in most of the reported cases in the literature include: 1) plaques or nodules; 2) fever, arthralgia and malaise; 3) an association with myelodysplasia; and 4) a response to steroids.1,3,7
Answer 4
Subcutaneous Sweet syndrome is responsive to steroids, which result in a rapid resolution of lesions, as observed in multiple previous reports.1,7 There have also been isolated reports of successful treatment with dapsone and adalimumab.1,8 However, the key to managing Sweet syndrome is treating the underlying pathology.6 In the present case, the patient showed a rapid response to corticosteroids, with an improvement in his skin lesions seen within a week and a complete resolution in three weeks. It is noteworthy that the patient was on rituximab, which is associated with lymphopenia.9 However, lymphopenia in the context of rituximab is self-limiting and not known to be associated with serious infections or other adverse outcomes.9
Answer 5
Erythema nodosum is a major differential to consider. It is often difficult to clinically distinguish from subcutaneous Sweet syndrome as it is also characterised by tender and erythematous nodules.1 However, erythema nodosum most commonly presents as multiple lesions on the bilateral lower limbs.10 Histologically, early erythema nodosum has similar features to subcutaneous Sweet syndrome as it commonly demonstrates a neutrophilic infiltration within the septa. This later evolves to show granulomatous lesions, which can help distinguish erythema nodosum from subcutaneous Sweet syndrome.10 Therefore, multiple deep incisional or excisional biopsies are sometimes required to establish a diagnosis.
Other less likely differentials to consider include pancreatic panniculitis, anti-trypsin 1 deficiency panniculitis, infective panniculitis and erythema induratum.
Key points
- Subcutaneous Sweet syndrome has a strong association with haematological malignancy and can signal a poor prognosis.
- Subcutaneous Sweet syndrome requires histopathological confirmation.
- Once a diagnosis of subcutaneous Sweet syndrome has been made, a careful evaluation for haematological malignancy should be performed, and the underlying pathology should be treated.