Discussion
There are a number of dietary constituents implicated in IBS, and patients’ main concerns are the trial-and-error nature of identifying triggers, uncertainty regarding food choices and reduced enjoyment of food. Despite this, dietary modifications are accepted by patients and healthcare professionals (HCPs) as an efficacious management strategy. A meaningful relationship with their HCP can improve patient adherence, treatment success and overall satisfaction for patients.
Irritable bowel syndrome (IBS) is a disorder of the gut–brain axis characterised by recurrent abdominal pain and altered defecation.1 In the absence of abnormal pathology, the Rome IV criteria can be used as a diagnostic tool based on symptom profile.2 Proposed mechanisms of IBS include psychological factors, miscommunication between the gut and central nervous system, dysmotility, altered mucosal immune and inflammatory function, genetic susceptibility, infection and gastroenteritis, alterations in gut microbiota and visceral hypersensitivity.3–5
A recent survey estimated an IBS prevalence of 3.5% in Australia and 4.1% globally.6 It is more prevalent in women, particularly those aged 18–39 years. In addition, 39% of survey respondents had visited a general practitioner (GP) for bowel problems, and patients attributed 30% of healthcare costs to visits with a GP.7 The cost of treatment is recognised by patients as a barrier to treatment, which is an important consideration for healthcare professionals (HCPs).8 IBS has a profound effect on quality of life, as social activities, employment hours and duties, leisure activity, sleep and travel can be impaired.9,10
Pharmacotherapy is often used to manage symptoms of IBS.11 However, lifestyle changes and complementary and alternative treatments are becoming increasingly popular. These alternatives to conventional treatments can offer a sense of control to patients and appeal to those dissatisfied with treatment from their HCPs.12 While there is some evidence to support these in practice, studies are limited by being short in duration or having not yet been reproduced.12,13 Encouragingly, there is now sufficient evidence of efficacy for dietary strategies in managing IBS,11 and the first large-scale controlled trial showing diet to be superior when compared with standard medical therapy in primary care–managed IBS recently published.14
Patients have described a preference for dietary modifications over medications for management of symptoms, reporting that they felt this was a more holistic approach.15 Dietary constituents implicated in IBS include high-fat foods, caffeine, spicy foods, alcohol, carbonated drinks and fermentable oligosaccharide, disaccharide, monosaccharide and polyol (FODMAP) carbohydrates. The British Dietetic Association recommends first-line dietary management for IBS to be general dietary advice inclusive of consuming regular meals and modifying intake of fluid, caffeine, alcohol, carbonated drinks, fibre and artificial sweeteners.16 Where this fails, advanced dietary interventions based on non-starch polysaccharides, FODMAPs and probiotics are considered (second line), followed by elimination and empirical diets (third line). Dietary interventions – including the specific carbohydrate diet, paleolithic diet, gluten-free diet and food chemical intolerance diet – lack high-quality studies with sufficient participant numbers to be recommended in practice.17 Symptoms may result from a single food constituent or from foods or meals with a composition containing one or more of these constituents. As a result of the number of potential food triggers and complexity of food composition, accurate identification of specific food triggers and implementation of dietary intervention by an HCP with dietary expertise is paramount.18
The aim of this narrative review was to explore the lived experience of IBS from the patient perspective with emphasis on dietary involvement and low-FODMAP diet management of the condition.
Methods
Medline and Scopus databases were searched using the terms ‘irritable bowel syndrome’ in conjunction with ‘beliefs’ or ‘attitudes’ or ‘experience’ or ‘concerns’ or ‘living’. Search terminology was combined with ‘qualitative’ or ‘quantitative’ to maximise the scope of research in this area. Relevant articles were examined, and themes relating to identifying food triggers, managing symptoms through diet and relationship with HCPs were explored for this narrative review. Fourteen studies using retrospective or prospective study designs that appraise the lived experience of IBS were included.8,15,19–30
Discussion
Dietary concerns of those living with IBS: Identifying food triggers
A high frequency of perceived food intolerance existed in patients living with IBS, where the more severe the symptoms reported, the higher the number of foods blamed,19 often resulting in a self-prescribed restrictive diet.20 Seventy-five per cent of patients believed that dietary factors are implicated in the development of IBS.15 Identifying trigger foods has been described by patients as a ‘trial-and-error’ approach that is lengthy and difficult and creates uncertainty about what foods would result in symptoms.21–23 Individuals described unpredictability of symptoms and feelings of uncertainty about what to eat and how much to eat.23 Some individuals reported the process to increase their sense of control, whereas others found this to be burdensome and increase anxiety.21 Additional anxiety was felt when dietary planning was needed, including attention to detail on food labels, grocery shopping and eating out. Individuals with IBS have described a reduction in the enjoyment of food, characterised as finding food boring, less ability to eat spontaneously and missing previously enjoyed foods.21 Furthermore, some felt that restrictions of diet affected general living through avoidance of trigger foods, high-fat foods and high-volume meals.23
Examining the experience of managing symptoms through diet in patients who live with IBS
A survey of individuals living with IBS found that 82% of respondents claimed diet to be an acceptable treatment for IBS, with those under the age of 55 years more accepting of it.24 Dietary implementation was assessed in an Australian cohort of 114 participants following the low-FODMAP diet.25 Seventy-nine per cent of participants stated that food labelling was sufficient to follow the diet, 61% of participants stated food was available at their usual place of food purchase, and 36% used speciality stores to purchase appropriate foods. Repeat consultations with a dietitian were requested by participants for advice on purchasing suitable options. Patients also reported that adherence to the low-FODMAP diet when eating out is challenging for patients fearing high-FODMAP food consumption, which can affect quality of life.20
The experience of patients living with IBS receiving dietary advice through general practitioners
Patients who have received dietary advice from their GPs have described the information as superficial, uniform and reductive in the sense of ‘allowed’ and ‘avoid’ food lists that lacked personalisation.26 Furthermore, patients advised to ‘Google’ information felt they were required to assess material themselves and found a significant amount of time was spent sourcing relevant and credible information, with much of it contradictory.26 Although patients reported feeling that their GP was a trusted source, wider implications including social effects, budget, meal planning and accommodation of family were concerns for patients receiving GP advice.26 A survey of 23 Asia-Pacific GPs acknowledged that 79% provided advice to patients about dietary habits and modification; however, not all took the time to provide an explanation.27
Relationship with healthcare professionals
Studies have examined the relationship between HCPs and patients living with IBS. Patients reported experiencing treatment scepticism from their HCPs, especially when there are no findings from diagnostic investigations undertaken and when changes in treatment pathways occur.28 A distrust of HCPs was evident among patients when symptoms did not respond to treatment,28 as well as a feeling of being fed-up and tired of the treatment process.29 In contrast, one meta-analysis showed that patients who had meaningful relationships with their doctors had reduced symptoms, improved treatment adherence and overall satisfaction.30
Dietitian involvement in implementation of dietary therapies
A comprehensive assessment of symptoms and education is integral to a positive patient response.18,31 Dietitian-guided education and implementation of dietary therapy is recommended. A recent meta-analysis showed the efficacy and success of a low-FODMAP diet in comparison to general dietary advice, sham diets and high-FODMAP diets.31 Importantly, the studies included were all clinical trials led by dietitians, emphasising the need for expert dietary support during this intervention. Between 50% and 86% of individuals respond in the initial restriction phase of the low-FODMAP diet.32 Figure 1 provides an overview of how a dietitian successfully implements the low-FODMAP diet. Dietitians can use motivational techniques to support patients, for example when re-introducing FODMAPs, by focusing on adequate fibre, micronutrients and prebiotic intake to promote short-chain fatty acid production for long-term bowel health.20,33–36 Access to dietetic services can be challenging because of cost and wait times; however, as a result of the chronic nature of IBS, patients may be eligible for Medicare Benefits Schedule rebates in Australia.37 A recent cost effectiveness analysis conducted using US consumer data focusing on psychological, pharmacological and low-FODMAP diet treatments found the low-FODMAP diet (US$1800–$1900 per year, including dietetic and overall diet adherence costs) to be cost saving to the individual and less expensive than some pharmacotherapy treatments (US$2531–$3288 per year).8
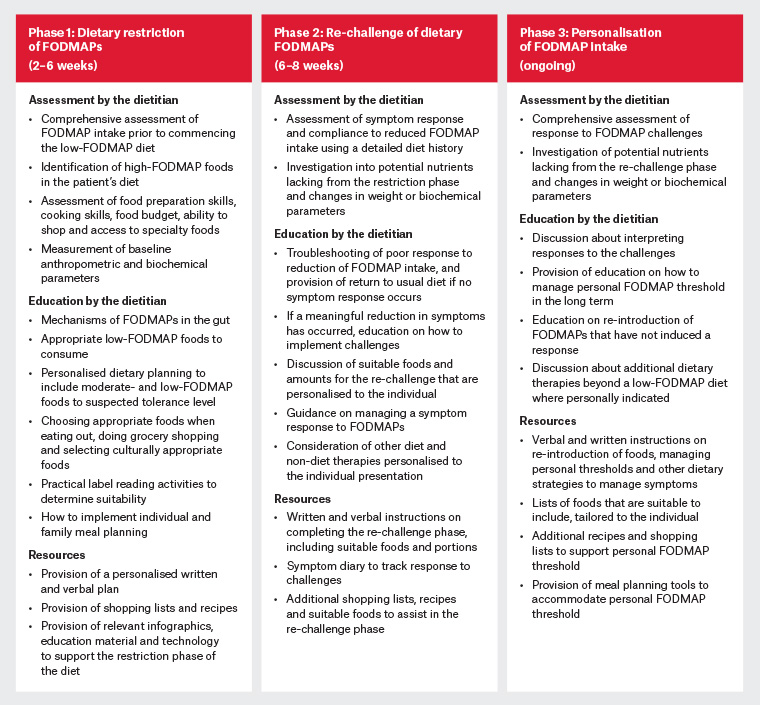
Figure 1. Dietitian involvement with each phase of the low-FODMAP diet
FODMAP, fermentable oligosaccharide, disaccharide, monosaccharide and polyol
Recommendations to general practitioners
The initial visit to a GP offers the opportunity for assessment of symptoms, including frequency, duration, severity and impact on quality of life. The British Society of Gastroenterology guidelines provide guidance on investigations to assist diagnosis.11 It is important that coeliac disease be excluded prior to dietary changes, as many dietary strategies (including the low-FODMAP diet) reduce gluten intake, which may cause a false-negative result for coeliac disease.38 Referral to a dietitian is indicated where bloating, pain or altered bowel motions occur within or up to several hours after eating; uncertainty regarding food triggers of symptoms exists; or anxiety is stemming from food choices.39 Management also includes GPs being aware of patients concurrently using dietary therapies or prolonging avoidance of high-FODMAP foods,17 which has been associated with the development of eating disorders.40 Table 1 provides resources that may be helpful to GPs when managing patients with IBS and undertaking the low-FODMAP diet as management.
| Table 1. Resources available to general practitioners |
| Intended audience |
Resource |
Description |
URL |
| Healthcare professional |
The Rome IV diagnostic criteria |
The Rome IV criteria is a diagnostic tool that provides guidance to healthcare professionals on symptom presentation and duration for an IBS diagnosis in patients. |
https://theromefoundation.org/rome-iv/rome-iv-criteria |
| Healthcare professional |
British Society of Gastroenterology guidelines on the management of irritable bowel syndrome |
This comprehensive guideline provides recommendations for doctor–patient communication; diagnosis; investigation and education in IBS; and first-line, second-line and psychological therapies. Refractory IBS management is discussed as well as themes for future research in IBS. |
https://gut.bmj.com/content/70/7/1214 |
| Healthcare professional |
The SCOFF questionnaire |
The SCOFF questionnaire is a screening tool that healthcare professionals can use to identify risk of disordered eating. Each ‘yes’ response equals one point, where more than two points suggests an underlying eating disorder. |
http://cedd.org.au/wordpress/wp-content/uploads/2015/04/SCOFF-Questionnaire.pdf |
| Healthcare professional |
Food avoidance questionnaire |
This self-administered questionnaire allows for screening of food avoidance and rationalisation of these behaviours. The results can be used to assist healthcare professionals with a diagnosis of avoidant/restrictive food intake disorder. |
https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-017-0160-4 |
| Healthcare professional and patient |
Monash University patient information sheets |
An A4 sheet with illustrations to assist the explanation of IBS and how to use the Monash University FODMAP Diet app. Healthcare providers can include additional notes for their patient on this handout. |
www.monashfodmap.com/shop |
| Healthcare professional and patient |
Monash University smartphone application |
An app that presents a guide to low-, moderate- and high-FODMAP foods using a traffic light system; low-FODMAP recipes; and a guide to following the low FODMAP diet. The app includes a food and symptom diary to help identify trends in IBS triggers. The app is available in English, Spanish, French and German. It can also be a useful aid for practitioners during FODMAP education. |
www.monashfodmap.com/ibs-central/i-have-ibs/get-the-app |
| Healthcare professional and patient |
Gastroenterological Society of Australia information about irritable bowel syndrome |
This leaflet is an educational resource providing an overview of IBS symptoms, potential causes of IBS and treatments and holistic management, including stress and lifestyle factors. |
www.gesa.org.au/education/clinical-information |
| Patient |
Monash University Low FODMAP Certified logo |
The Monash low-FODMAP certification logo provides reassurance to individuals with IBS that brands or products have undergone FODMAP testing. |
www.monashfodmap.com/product-and-recipe-certification-program |
| FODMAP, fermentable oligosaccharide, disaccharide, monosaccharide and polyol; GP, general practitioner; IBS, irritable bowel syndrome; SCOFF, sick, control, one, fat, food |
Conclusion
IBS is a complex and chronic condition with a profound effect on quality of life. Patients report experiencing uncertainty and anxiety when identifying food triggers; however, dietary modification has been widely accepted by patients and GPs as a treatment modality. Individuals living with IBS have asserted the need for personalised management advice. Ensuring a good relationship between the patient and HCP can improve treatment outcomes for those living with IBS.
Key points
- Identification of food triggers in IBS can be complex, and patients find this to be burdensome and a cause of anxiety.
- Meaningful relationships with the HCP can improve treatment success and overall satisfaction for patients.
- Referral to a dietitian is warranted where food is thought to be implicated in a patient’s presentation of symptoms.
- The three-phase low-FODMAP diet, involving initial restriction followed by re-challenge and long-term maintenance, is a cost-effective and efficacious strategy when delivered by a dietitian.