Continuity of care (or simply, ‘continuity’), which Haggerty et al define as the degree to which a patient experiences their care as ‘coherent[, …] connected and consistent with [their] medical needs and personal context’, has been recognised as a feature of high-quality medical care, especially primary care, for more than half a century.1 Recent studies have reinforced this consensus, with data associating continuity with increased patient2 and provider3 satisfaction, decreased cost of care4 and even decreased mortality.5 However, measuring, tracking and improving continuity remains a significant challenge, in part because of the subjectivity and complexity of the patient–provider relationship. In addition, technological advancements in healthcare delivery may threaten the validity of existing measures of continuity. Here we review existing measures of patient-experienced continuity of care, discuss how they are affected by technology-related changes to healthcare and suggest avenues for future research on continuity.
Components of continuity
Continuity is a subjective, multidimensional experience of patients. Haggerty et al described continuity as a combination of informational continuity (knowledge of a patient’s history), management continuity (consistent medical management) and relational continuity (therapeutic provider–patient relationship).
1 Longitudinality (frequent or sustained interaction between a provider and a patient, which may be measured objectively) is not a component of continuity per se but may be an important facilitator of or even prerequisite for a patient’s sense of continuity.
6 These terms are described in Table 1.
| Table 1. Key terms |
| Term |
Definition |
Subjective or objective? |
Collection method |
| Continuity of care |
Care connected, consistent, in line with a patient’s needs and personal context |
Subjective |
Self-report instruments* |
| Types of continuity |
Informational |
Care based on information from a patient’s prior history and circumstances |
| Management |
Consistent management in accordance with a patient’s needs |
| Relational |
Therapeutic provider–patient relationship |
| Longitudinality |
Frequent or sustained interactions between a provider and a patient |
Objective |
Self-report or utilisation data |
| *For further descriptions of self-report instruments, refer to Ball et al, 20187 |
Current measures of continuity
A patient’s subjective sense of continuity is most intuitively assessed through self-report. As reviewed by Ball et al,7 several self-report instruments have been developed, with different surveys emphasising different aspects of continuity but without the emergence of one clear gold standard. These instruments have their limitations: as with any self-reported measure of human perceptions or behaviour, it is critical to re-examine the measurement properties (eg reliability and validity) of these measures when they are applied to new populations and care settings. In addition, because they must be collected prospectively from individual patients, self-report instruments are labour intensive.
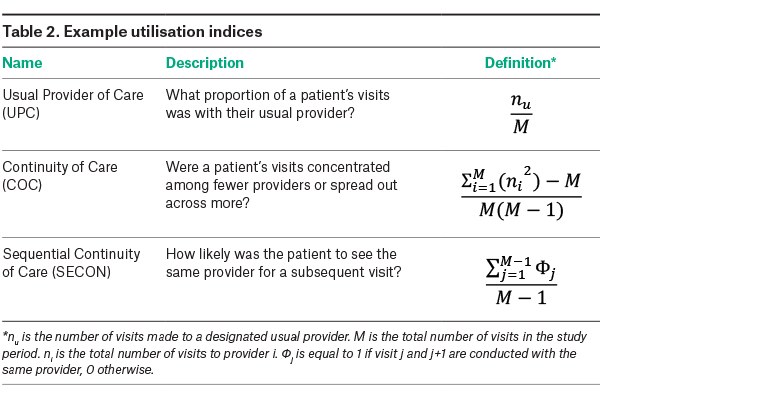
Utilisation indices are efficient methods of measuring longitudinality and are often used as an alternative means of describing continuity. These are objective measures that calculate a score on the basis of a patient’s frequency of visits with a given provider (or providers), a patient’s total visits and sometimes other factors such as duration of care. Examples of common utilisation indices are summarised in Table 2, but many more have been introduced and were well summarised by Jee and Cabana.8 Because utilisation indices for continuity can be calculated retrospectively on the basis of patient report or medical records, they can be applied relatively easily to any population or care setting.9 Although these measures of longitudinality assess continuity only indirectly, they have nonetheless been consistently shown to correlate with positive clinical outcomes.5
Continuity and technology-enabled care
Recent technology-related changes in the practice of medicine will have a profound effect on both the provision and measurement of continuity. Thanks in part to expanded telehealth support in response to the COVID-19 pandemic,10 patients today may supplement in-person consultations with telephone or audiovisual telehealth, and they may also communicate with their providers asynchronously through apps or secure text or email communication. These novel ways to connect may contribute to patients’ sense of continuity in ways that are not captured by traditional measures. Self-report measures of continuity developed before telehealth often assess continuity using questions that imply only the option of face-to-face encounters, as when the Chao Perception of Continuity scale asks how often patients ‘see the same doctor when [they] go for medical care’.11 Faced with such questions, respondents who achieve significant relational continuity through technology-enabled communication or visits may misrepresent and underrepresent their sense of continuity. Similarly, utilisation indexes generally calculate longitudinality on the basis of in-person consultations only, overlooking entirely the contributions of technology-facilitated interactions.
Shared electronic health records (EHRs) allow providers (even new ones) to provide care based on a patient’s prior history and treatment plans,12 which may increase informational and management continuity without longitudinality. These continuity benefits of shared EHRs would likely be reflected in self-reported continuity measures but would have no effect on the longitudinality calculations of utilisation indices.
Future directions
By facilitating informational and management continuity between multiple providers, and by facilitating all forms of continuity without in-person longitudinality, shared EHRs and technology-enabled doctor–patient interactions, respectively, violate some of the assumptions underpinning current continuity measures. In response, we suggest three research aims to update the measurement of continuity. First (1), self-reported measures should be adapted to become inclusive of technology-enabled care. They might ask, for example, whether patients ‘interact with the same doctor when receiving medical care’. With these updated measures, once appropriately validated, it may be possible to confidently assess patients’ sense of informational, relational and management continuity in practices that incorporate technology-enabled care and to (2) compare continuity with and without telehealth and other technologies in order to quantify the degree to which these additions contribute to continuity. Finally (3), utilisation indices should also be updated to incorporate the continuity effects of technology-enabled care. This might at first mean treating telehealth visits as ‘in-person equivalents’. However, in time the work described above would facilitate the creation of utilisation indices that ‘value’ different interactions, from in-person consultations to SMS messages, according to their contributions to continuity.
Some of the same technologies we suggest evaluating may themselves facilitate these three ambitious research aims. EHRs can compile a complete and objective log of patients’ care, facilitating the calculation of utility indices without relying on faulty patient recall. Technologies such as check-in kiosks,13 secure text messaging14 and smartphone applications15,16 are increasingly used to communicate with and collect information from patients, which might include continuity self-reports. Even with these tools, there is extensive work to be done to understand how patients experience continuity in a modern healthcare environment. We contend that these efforts will be worthwhile. As long as continuity remains an important component of quality healthcare, updated, valid tools to measure continuity should be of interest to practices, health systems and governmental organisations alike.