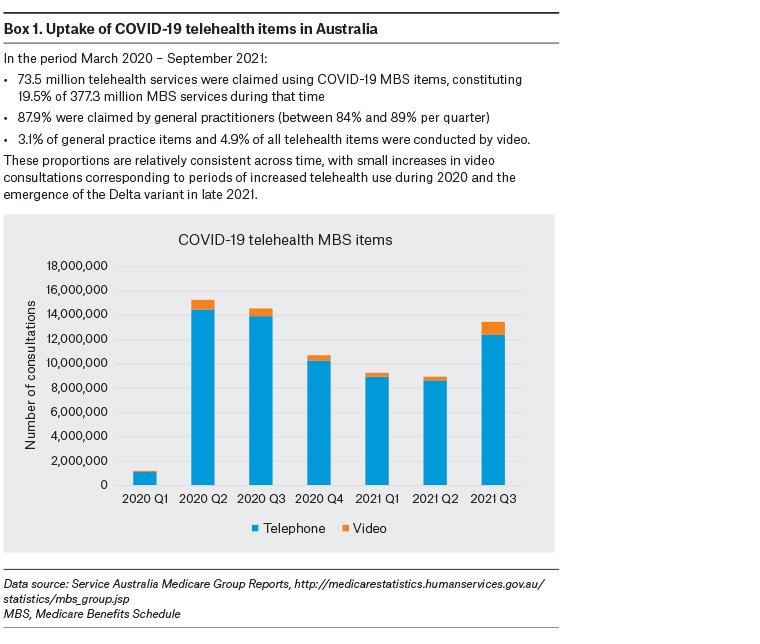
Internationally, the provision of primary care during the COVID-19 pandemic has greatly relied on remote consulting via telehealth, which has been rapidly expanded and enhanced to protect patients and clinicians from exposure to COVID-19, while ensuring ongoing access to care.1 In many jurisdictions, video consultations have been considered the preferred substitute for in-person consultations,2 underpinned by the assumption that video provides a better consultation platform than telephone, with potential to support higher quality care.3 However, primary care providers’ (PCPs’) and patients’ experiences of using telehealth during the COVID-19 pandemic indicate that this assumption may not be universally valid. In Australia, remuneration for telehealth services delivered via remote consulting was progressively introduced from March 2020,1 and it has now been made permanent.4 Telephone consultations have been consistently more frequently used than video consultations (Box 1), suggesting other factors may influence choice of consultation mode. The current draft Primary Health Care 10 Year Plan acknowledges these issues but notes the importance of visual cues in patient assessment, anticipating increased use of video consultations as technological functionality improves.3
Aim
This commentary draws on and synthesises the key findings of two rapid narrative reviews, conducted in July 2021 at the request of policymakers to inform policy decisions. We examined the international literature over the previous two years for evidence regarding the quality of telephone consultations and comparisons of video consultations and telephone consultations in order to identify emerging insights regarding the quality of both during COVID-19. While there is also value in the use of other synchronous and asynchronous telehealth modalities, such as sharing of vital signs or images within or outside of remote consultations, this exploration was chiefly concerned with comparative assessments of telephone consultations and video consultations and whether assumptions of superiority are supported. All studies cited herein were published between mid-2019 and mid-2021.
Clinical assessment and communication
In 2019, prior to the onset of COVID-19, general practitioners (GPs) in the UK felt that video consultations offered distinct advantages over telephone consultations and were particularly useful when physical examination was not required.5,6 Internationally, in the pandemic context between March and August 2020, PCPs, patients and nurses also believed video consultations provided better capacity than telephone consultations for visual assessment:7 to observe visual nuances and cues,8 reduce the risk of miscommunication and build rapport.5 This was considered particularly valuable for consultations with the elderly, multidisciplinary team assessments, dynamic assessments (eg observing gait and respiratory movement)9 and delivering women’s health programs.8 However, lack of visual clarity via video consultations at times made in-person assessment of wounds preferable.10
A US study of frontline worker perspectives from March to July 2020 considered video consultations superior to telephone consultations in facilitating clinical assessment of patients in their home environment and understanding challenges that may warrant referral for home care or medical equipment – information that may not be captured via telephone consultations or in-person consultations in the clinic.11 Previous research, published in 2019, found that video consultations were useful for watching patients exercise and draw up medications, although some PCPs expressed concern about using video consultations for observing living spaces because of the potential for patients to fall over while walking around and holding an iPad.12 A study examining a geriatric clinic’s conversion to video consultations in March – May 2020 found that some platforms made it possible for distant family members to join the consultation and meet the broader interdisciplinary team.10
While some PCPs expressed a preference for video consultations, others reported that video consultations and telephone consultations were equivalent, and they only used video consultations if they needed to see something (eg the face of a patient with depression, or a rash). In studies conducted from April to August 2020,13 and May to July 2020,9 some Danish and UK GPs preferred to combine telephone consultations and photographs,13 particularly for ‘static problems’ that required visual assessment (eg rash).9 UK GPs also found it challenging to know how or when to switch from telephone to video, with concerns related to missing physical signs of disease.9
Studies examining patients’ perspectives in 2017–18 found it was considered easier to converse while looking at someone, with video consultations perceived as more interactive,12 personal and reassuring than telephone consultations.5 Australian patients with multiple sclerosis interviewed in June – July 2020 believed video consultations were better than telephone consultations at facilitating communication, including observing body language, and for getting to know a clinician at a first-time visit.14 Research conducted prior to the pandemic found that UK patients and GPs alike felt that video consultations provided a more formal and focused setting than telephone consultations.5
Technology set-up and usability
While many PCPs and patients indicated preferences for video consultations, this was contingent on usability. Studies conducted between March and May 2020 found that although video consultations and telephone consultations were often comparable in terms of performance and user acceptance,15 many patients and PCPs experienced substantial challenges in using video consultations, finding them difficult and stressful7 and time-consuming to set up.10 In research conducted prior to the pandemic5,6 and between May and August 2020, 8,9 both UK GPs and Australian nurses highlighted the need for infrastructure to enable the seamless integration of video consultations into clinical practice.5,6,8,9 Technical problems were more commonly reported with video consultations than telephone consultations, with some PCPs reporting having to end consultations sooner than intended8 or refusing to use video consultations again.6 Patients interviewed in April – May 2020 for a New Zealand study described substantial technological barriers to using video consultations, including insufficient broadband speed, unstable internet connection, poor image resolution and poorly angled cameras.7 In a US study conducted prior to the pandemic (2017–18), older veterans found visual cues supported interaction, but those unfamiliar with technology also found the use of video consultations very frustrating.12 Similarly, research in the UK prior to the pandemic found that patients who were confident using video consultations were more likely to feel confident using other modes of internet communication.6
Quality and safety
One study conducted in April – May 2020 rated the quality of video consultations significantly higher than telephone consultations for developing the patient–clinician alliance, meeting patients’ needs, providing care that is equal in quality to face-to-face care and being able to freely talk about patient issues.15 However, this same study found telephone consultations comparable to video consultations in terms of technological performance and user acceptance,15 as did two other studies conducted between May and August 2020 when considering the content and quality of patient–clinician interactions.8,16 The evidence for satisfaction was mixed; both patients and providers interviewed in May – June 2020 were satisfied with telephone consultations for simple issues such as prescription renewal, discussing test results and chronic condition follow-up.16 One study of interprofessional care providers in the USA conducted in April – May 2020 indicated that both PCPs and patients were more satisfied using video consultations than telephone consultations,15 whereas other research conducted in a geriatric clinic in the USA in March – May 2020 indicated that patients and PCPs were equally satisfied using both modalities.10
Despite the apparent advantages of video consultations, the pronounced prevalence of telephone consultation use in comparison to video consultation use during the COVID-19 pandemic was a common pattern internationally.1,16 This was linked to availability, acceptability and patient16 and provider preference. Telephone consultations enabled continued access to clinical care and were acceptable to patients, with engagement dependent on access, confidence, perceived safety and value.8,15,16 The limitations of telephone consultations were acknowledged; they did not support complex clinical assessment8 and were considered less personal, with less capacity to read body language, build rapport and meet patient needs.14,15 However, between March and September 2020, telephone consultations were considered a valuable, safe and resource-friendly alternative to in-person visits when following up and monitoring suspected COVID-19 patients in domiciliary care;17 for the short-term provision of direct-to-patient medical abortion services, including assessment and counselling;18 and for maintaining glycaemic control in patients with suboptimal control of type 2 diabetes.19
Research conducted between April and July 2020 found that the quality of consultations was influenced by a variety of factors, including mismatches between patient preferences and provider perceptions of suitability, patient multitasking while undertaking consultations, interoperability challenges and equipment availability and performance issues.20 PCPs had mixed views on the safety of patient assessment via both telephone consultations and video consultations, noting virtual consultations were most safe for existing patients and simple tasks. While they were an important enabler of frequent connection with and monitoring of patients, they were routinely preferable only when infection risk was high.20 There were particular quality issues for certain patient groups, especially those with communication challenges and poor technology access and those deprived of suitable spaces in which to conduct virtual consultations.20 Ensuring the quality of video consultations among these groups often required particular supports and new workflow configurations from primary care practices and staff, creating substantial additional administrative burden. For example, video consultations may require more complex scheduling arrangements, wait times in virtual rooms and longer consultation length than in-person or telephone consultations, especially when patients are unfamiliar with the technology.
Medico-legal risks
Rapid uptake and increased use of telehealth exposed several emerging medico-legal risks that may require added vigilance or action by PCPs. These include clinical risks related to remote consultations, such as the absence of physical examination; structural issues, such as adequate and reliable bandwidth;21 and the potential for declared or undeclared, and intended or unintended, third parties witnessing consultations.22 Some authors have suggested the onus is on practitioners to ensure the integrity of communications in addition to obtaining informed consent (including risks, limitations and alternative modalities).23 Others have highlighted the need for specific consent for clinician-led recordings, and the possibility of patient-generated recordings that may be disclosed or undisclosed, as it is legal to record without participant knowledge in some jurisdictions.22 Such recordings have clinical, research and education benefits but can carry liability risks in terms of future use. As they constitute health information, they also generate ongoing obligations related to legislative and regulatory requirements for data management, including privacy, storage and security compliance.
Equity
In research conducted from April to July 2020, barriers to the use of telehealth modalities for patients who struggled with digital health were commonly highlighted.20,24 Similar to research conducted prior to the pandemic,25 this digital divide affected access to and utilisation of technology among population groups such as the elderly, people who were homeless or on low incomes, those with chronic conditions and those with low digital or health literacy. Research conducted between April and August 2020 found that these difficulties were compounded by societal inequities such as poverty and differences between rural and urban access to technology and internet infrastructure.7,8 The critical need for video consultation platforms that enabled interpreters to be involved for people from culturally and linguistically diverse backgrounds was noted by Australian primary care nurses in June – August 2020.8 A 2016–17 evaluation of professional interpreter services via video consultations found that the quality was high.26
Conclusion
The evidence base comparing the effectiveness of video consultations and telephone consultations during the COVID-19 pandemic is limited and evolving, with mixed findings. While video consultations can offer distinct advantages over telephone consultations under some circumstances, PCPs and patients have reported both positive and negative experiences and preferences in relation to each modality. Emerging evidence emphasises inequities in access to and utility of video consultations for some members of the community. However, task complexity, timing and purpose are likely to be a determinant of effective telephone consultations, the value of which may be highly context dependent.
While available evidence for the quality of care arising from each modality is currently inadequate to form firm conclusions, these insights provide critical knowledge to inform improvements to existing models of telehealth and shape future interventions.
The COVID-19 pandemic has demonstrated that, for video consultations to be seamlessly incorporated into day-to-day clinical practice, technical infrastructure should enable integration of video consultations with appointment systems, the capability of staff and patients to use it effectively may need development, and clinical workflows might require redesign. Widespread use of video consultations and telephone consultations has created new obligations and risks related to data management and security that PCPs should be aware of. Continuing research and evaluation efforts should examine the outcome of care delivered via telehealth and explore the role and purpose of different delivery modes and the ways in which they support high-quality patient care. While disparities in access and utility remain, telephone consultations may be the most readily available and appropriate telehealth modality for many people or situations, enabling access to effective and continuous clinical care that is acceptable to PCPs and patients alike.
Key points
- Video consultations offer distinct visual advantages for evaluating patients’ health and wellbeing.
- Technical infrastructure is essential to enable integration of video consultations into practice.
- Many clinicians find telephone consultations equally effective as video consultations in most situations.
- Access inequities to video consultations for some members of several at-risk groups have emerged.
- Evidence regarding the quality of both telephone and video consultations is sparse but evolving.