Strangulation refers to external pressure applied to the neck, causing compression of and potentially injury to vital structures, and obstruction of blood and/or air flow.1,2 Strangulation is often underdiagnosed by healthcare providers and minimised by survivors.3 Patients may not recognise an event as strangulation and may use other terms such as ‘choking’ or ‘pressure on the neck’, and may minimise or not appreciate the seriousness of the incident they have survived. Strangulation may be used as a covert form of control and intimidation in intimate partner settings, sexual assault and child abuse.4 It can be used repeatedly, leaving few traces, obscuring occult brain and neck injury.5–7 In justice and healthcare settings, strangulation is increasingly recognised as a serious act of domestic violence and predictor of future homicide risk.8–12
Epidemiology and significance
Lifetime prevalence of strangulation in the community is reported as ranging 3.0–9.7%, with increased incidence in vulnerable communities,13 an incidence of up to 68% in domestic violence services,14 and up to 9.28% in sexual assault services (with up to 58% strangled by a partner or ex-partner).5,15 Approximately 8–28% of women presenting to Australian general practitioners (GPs) will have experienced domestic violence in the past 12 months.16,17 Some of these women will have experienced strangulation.
Strangulation by an intimate partner increases the risk of future homicide by that partner by 7.48 times.18 Non-fatal strangulation may also lead to injury. One small audit of 48 patients referred for imaging after forensic examination due to non-fatal strangulation noted internal injury in five patients (including three patients with neck artery dissections).19
Beyond the intimate partner violence context, we note that non-fatal strangulation is also used in consensual sexual practices,20 including chemsex and group sex subcultures, and has been used in autoerotic contexts, violent pornography and dangerous adolescent ‘choking games’,21 leading to accidental death.22 Further discussion of non-fatal strangulation in these contexts, as well as injuries seen in near-hangings and hangings in a mental health or homicidal context (addressed in the forensic medical literature),23 is beyond the scope of this article.
Pathophysiology
Pressure to the neck can be via one or two hands applying the pressure (manual strangulation), by applying pressure using a forearm from behind (chokehold strangulation), or using a ligature or object. Pressure can be gradually exerted, sudden, or on-off in nature, particularly during a prolonged struggle or dynamic assault. Research from the 1940s on institutionalised ‘volunteers’ demonstrated a consistent sequence of events during strangulation.24 Generally, loss of consciousness occurred around 6.8 seconds (range 4–10 seconds), possible anoxic seizure by 14 seconds (range 11–17 seconds) and, occasionally, urinary incontinence from 15 seconds and then faecal incontinence from 30 seconds.24 There was often a period of post-strangulation confusion, often without awareness of their loss of consciousness.
Injuries result from a variety of mechanisms (Table 1) and depend on the duration, degree and area of pressure, associated shearing forces, or forced extension of the neck. Interruption of venous return from the head with ongoing arterial supply to the head causes increased pressure in small vessels in the head and neck and resulting signs of injury such as petechial bruising or subconjunctival haemorrhage. Sudden interruption of both arterial supply and venous return can result in hypoxic or vascular injury with no external sign of injury.25 Studies of non-fatal strangulation patients reveal no visible physical injury in around 50% of patients.5,15
| Table 1. Mechanisms of injury in strangulation2,24,35 |
| Mechanism |
Clinical features |
Damage |
| Venous occlusion |
Pressure behind the eyes, ‘seeing stars’, swelling, headache and nausea, loss of consciousness |
Congestion of venous return results in capillary and small vessel leakage (petechial haemorrhages) or larger bleeds
Cerebral oedema |
Arterial occlusion
|
Pre-syncope, syncope, headache, poor memory or memory gaps |
Hypoxic brain injuries that may manifest in specific neurology or a concussive picture |
Airway occlusion
|
Hypoxia and hypercarbia, panic, pain, inability to breathe, inability to swallow or speak |
Hypoxic brain damage
Damage to the larynx
Perforations to the airway
Compression of the airway both at the time or by subsequent traumatic oedema, pulmonary oedema (from large pressure changes while fighting to breath against an obstruction)
Hypoxic injuries to organs (and fetus) |
| Psychological injury due to incident and hypoxia to hippocampus |
Fear, sense of being overwhelmed, despair, acceptance of imminent death |
Post-traumatic stress disorder, domestic violence–related damage to self-esteem, impaired decision making and risk assessments |
Where physical injuries occur, they may range from bruises (particularly subtle in dark skin) and petechiae, to oedema of soft tissues and airway obstruction up to 36 hours post strangulation.26 Subtle fractures to the larynx and hyoid bone can occur.27,28 Vascular injury to the carotid arteries or jugular veins may include blunt trauma to the great vessels causing carotid artery dissection and subsequent stroke.29–32 Hypoxic-ischaemic brain injury from significant interruption of cerebral blood supply or congestion and haemorrhage causing damage is likely underdiagnosed at present and requires further research. As with traumatic brain injury and concussion, this may produce cognitive deficits of memory and executive function, affecting attention and processing speed.33
The experience of being strangled during an assault is clearly traumatic irrespective of physical injury. Patients may report a sense of imminent death and feel compelled to comply with the perpetrator’s wishes to protect themselves or their children.5,25 The 1940s study documented an inability to move to release the strangulation device, echoing patient reports of being ‘frozen’ while being strangled.24
Clinical assessment of strangulation
Patients presenting with obvious airway compromise, respiratory distress or evolving neurological deficits should be referred urgently to an emergency department (ED) via ambulance. Otherwise, a detailed history of the strangulation can be taken (Box 1). The patient may be unable to provide a linear narrative of the event due to extreme distress or fear, if there was a period of anoxia affecting memory formation at the time (even while conscious) or if they are drug or alcohol affected. The history may have to be recorded as a series of notes of what the patient can recall about the incident, without a linear narrative. As well as documenting responses to the questions in Box 1, note any sense of impending death or feeling unable to move, and any red flag symptoms.
In the sexual assault context, the sexual assault may be a distracting injury in a trauma – the patient may minimise or forget to mention the strangulation in their distress about the sexual assault, so asking about strangulation must be explicit.
Complete a targeted physical examination including rapid neurological examination. Assess for airway and neck injury, respiratory distress, arterial or vascular pressure injuries, neurological changes and other external signs of injury (Box 1).
Careful and accurate documentation are particularly important if this is a first disclosure of a recent strangulation, as your notes may be used as evidence in future if reported to police or if a death investigation follows. Document any mention of escalating patterns of threats/violence or previous strangulations, any current safety fears, and relevant positive and negative findings particularly for red flag features. Consider consulting clinical forensic medical services if available in your jurisdiction for advice on documentation and medico-legal processes.
| Box 1. History and examination41 |
Taking a history
Ask: ‘Was any pressure applied to your neck?’
Open questions:
- ‘Can you tell me what you remember about what happened?’
- ‘What concerns do you have about your body?’
Closed questions:
- ‘Can you describe how it happened (how they applied pressure to your neck)?’
- ‘When did this happen? Where? How long for? How did it stop?’
During the assault:
- ‘Did you have any trouble breathing or speaking?’
- ‘Did you feel like you were going to pass out?’
- ‘Did you notice any changes to your vision?’
- ‘Did you experience any pain anywhere?’
- ‘Do you have any gaps in your memory around this time?’
- ‘Did you experience any incontinence (of bladder or bowel)?’
After the assault:
- ‘Have you noticed any …
- pain or discomfort anywhere?
- changes to your vision?
- weakness or clumsiness in your limbs?
- dizziness/funny turns/fits?
- difficulty/change in speaking/swallowing/breathing?
- bruising or swelling?’
Approach to examination
Assess vital signs and manage any immediate compromise, particularly to the airway or level of consciousness. Then perform a targeted physical examination.
- Airway: Assess for laryngeal or neck injury – change in vocal quality (hoarse, husky, loss of voice), subcutaneous emphysema, neck swelling/deformity, tenderness, pain on swallowing).
- Breathing: Assess for serious respiratory distress/changes requiring urgent hospital transfer.
- Circulation/carotids: Assess for signs of arterial injury – look for carotid bruising and auscultate for carotid bruits. Assess for signs of increased vascular pressure injuries – examine the head and neck, including the eyes, mouth and throat, looking for petechiae, bruising, subconjunctival haemorrhages, tide mark.
- Disability/deficits/decreased level of consciousness: Assess for neurological deficits with rapid screening neurological examination (cranial nerves, gross upper and lower limb examination, Mini-Mental State Examination or Montreal Cognitive Assessment [MoCA]*) and note any confusion/impairment to level of consciousness.
- External signs of injury: Examine for any further signs of struggle or injury – for example, ligature marks, bruising or abrasions on the neck (either from the offender’s hands or ligature, or from the victim’s own fingernails trying to remove the offender’s hands).
|
| *MoCA printable test sheet is available at www.parkinsons.va.gov/resources/MOCA-Test-English.pdf; scoring instructions are available at www.parkinsons.va.gov/resources/MoCA-Instructions-English.pdf |
Management
Immediate management
If the patient has presented immediately after the strangulation event and physical red flags are identified on assessment (Figure 1), referral to an emergency department (ED) is recommended for imaging and observation for delayed oedema or evolving neurological deficits (as for a head injury) and for social worker input.
Not all patients require referral to EDs after a recent strangulation. A well patient without red flags or presenting several days after the event may be managed in primary care, including risk assessment for child safety and domestic violence safety red flags, with support of relevant services (Figure 1).
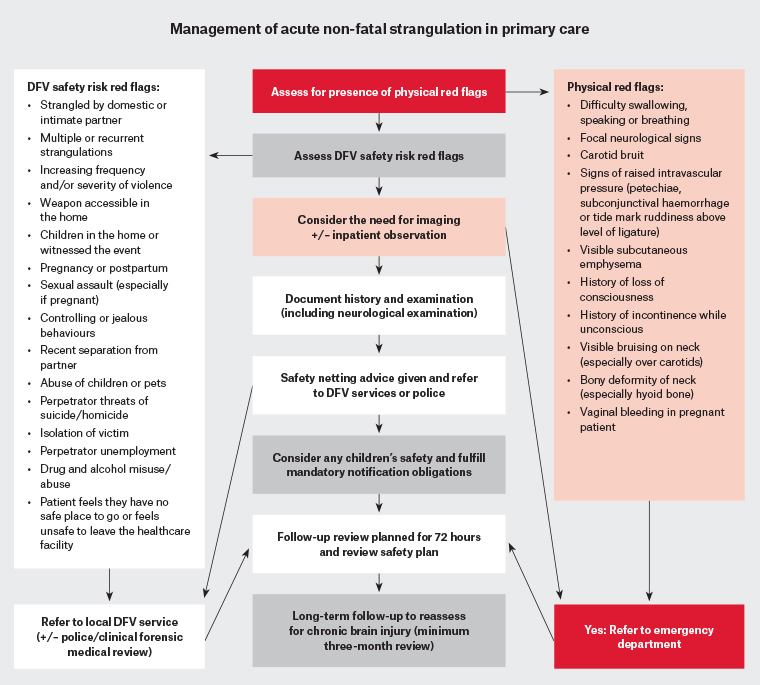
Figure 1. Management of acute non-fatal strangulation in primary care. Click here to enlarge.
DFV, domestic and family violence
Imaging and other investigations
Recommendations regarding imaging are evolving rapidly as new research emerges. The type and utility of imaging depends on the injury suspected. Currently all patients presenting after recent strangulation with new or evolving neurological deficits, carotid bruits or neck bruising over the carotids, particularly with a history of loss of consciousness, should be referred to an ED for assessment and urgent computed tomography (CT). CT angiography is currently the modality of choice for assessment of the great vessels to exclude carotid dissection, and CT of the brain for cerebral oedema and intracerebral haemorrhage.34,35 Consider radiation load on the thyroid in patients presenting recurrently after strangulation.
Airway injury can be assessed by nasendoscopy, CT or both, depending on availability. Nasendoscopy may be used for assessment and documentation of bruising and swelling of the larynx and vocal cords.27 Consider magnetic resonance imaging (MRI) or CT of the neck where laryngeal trauma or cervical spine injury are suspected.36 CT may indicate where air has left the airway after a perforation. MRI may be more appropriate in the pregnant patient or to evaluate less serious soft tissue injury, but it has drawbacks in sensitivity and specificity in vascular injuries, duration, cost, comfort and accessibility.
A stable patient without red flag features may not need imaging, and a delayed presentation may have imaging in the community if available promptly. Note that carotid Doppler ultrasound is not currently recommended in screening for dissection after blunt trauma, due to poorer sensitivity and sonographic inaccessibility of the upper carotid segment (more likely to be injured from trauma).34,35
Monitoring
Guidelines recommend monitoring for at least six hours after strangulation,1 but delayed oedema has been reported up to 36 hours.26 Irrespective of whether monitored in hospital, all patients should only be discharged into the care of another safe adult who is aware of red flags and when to return, similar to post–head injury care. They should be aware to re-present to an ED should any difficulty in breathing, upper airway swelling or neurological changes emerge (refer to safety netting advice in Box 2). Socially isolated or vulnerable patients may require admission for monitoring.
| Box 2. Discharge and safety netting advice1 |
Give verbal discharge instructions. Offering a concrete resource is also important, as memory may be affected by strangulation and psychological distress – a discreet hard copy SOS card that can be ordered in multiple languages and does not mention domestic violence or use the word ‘strangulation’ is available at https://aci.health.nsw.gov.au/search?query=strangulation
Advise patient to return for a routine follow-up in 48–72 hours with you/their general practitioner.
Also advise patient to report to an emergency department or call 000 if they notice or experience:
- difficulty breathing or shortness of breath
- confusion
- loss of consciousness or ‘passing out’
- changes in voice or difficulty speaking
- difficulty or pain when swallowing, a lump in the throat, or muscle spasms in throat or neck
- tongue swelling
- swelling to throat or neck
- seizures
- behavioural changes or memory loss
- escalating distress and urgency of thoughts of harming self or others.
Advise patient that if it is safe to do so, to keep a log of any of these symptoms over the next few weeks for legal reasons. |
Follow-up
All patients should be provided with GP follow-up, given support and validation around their experience and offered warm referrals for domestic violence and counselling services as relevant. Risk assessment and safety planning should be undertaken for all patients where there is an ongoing risk of harm (refer to Lynch et al37 in this issue of Australian Journal of General Practice for more on safety planning).
Follow-up appointments should be made for review within 72 hours to check for evolving neurological deficits, and again at three months to assess for cognitive impairment (or sooner if there are ongoing domestic violence or mental health concerns). While the first two weeks are considered the highest risk time for stroke after traumatic and spontaneous dissection,38 case reports exist of stroke several months after strangulation.39 Ensure all patients receive safety netting advice (Box 2) at every visit.1,38,40
If the patient experiences persistent memory loss or subtle cognitive deficits, consider formal assessment for brain injury, particularly in the context of repeated strangulation or head injuries7 (Box 3). Avoid raising expectations of rapid legal resolution if in the setting of ongoing domestic violence legal processes.
| Box 3. Traumatic brain injury |
Consider traumatic brain injury if evidence of:
- ongoing poor concentration or memory difficulties
- new communication difficulties (difficulty following conversations)
- persistent altered mood
- persisting cognitive impairment
- personality or behavioural changes.
Perform Montreal Cognitive Assessment or Mini Mental State Examination.
Refer for formal assessment for traumatic brain injury by neurologist, brain injury service, neuropsychology or neuropsychiatry service. |
Balancing the desire to maintain a therapeutic relationship with the patient against concerns about serious risk of harm can be difficult, so seek advice from specialist domestic family violence services or medicolegal indemnity providers if unsure. The patient’s wishes regarding police referral should be respected unless they or any children involved are at imminent risk of serious harm or homicide, in which case a duty of care to protect the patient and children overrides confidentiality. Legislative definitions and requirements around information sharing and mandatory reporting of domestic violence and children at risk of serious harm vary across jurisdictions. If in a situation where reporting must occur, it is good practice to inform the patient beforehand, as reporting may increase their immediate safety risk.
Conclusion
Non-fatal strangulation is potentially under-recognised as a contributor to morbidity in general practice. Identifying higher risk strangulation features such as loss of consciousness (particularly if associated with incontinence), neurological deficits, visible bruising and pain or difficulty swallowing or speaking can aid clinical decision making. The context of the strangulation is important to ascertaining ongoing safety risks for the victim and their children. Informing patients of future homicide risk if strangled by an intimate partner and connecting them to the wider domestic and family violence supports may prevent a future homicide.