Chest pain is a frequent cause of presentation to primary care and emergency departments1 and is associated with significant healthcare costs.2 Timely assessment and accurate diagnosis is required because of the possibility of a life-threatening cause,3 with the most common causes of chest pain including cardiac, gastrointestinal, musculoskeletal and functional/psychiatric. Even following negative investigation for cardiovascular causes, recurrent episodes of chest pain may continue to be responsible for a significant burden of disease for both the individual involved and the healthcare system.4 Without a definitive cause being established, uncertainty persists, and patients are often left dissatisfied with the diagnosis of exclusion represented by noncardiac chest pain (NCCP).5 Despite the relatively benign prognosis once significant underlying cardiac disease has been excluded, patients with NCCP may continue to experience an impact on their daily activities and working life,4 sometimes with a lingering suspicion that they do in fact have significant underlying heart disease that has not been diagnosed, with resultant anxiety that may drive further symptoms and healthcare use.
NCCP is, by its nature, a broad term – a condition of exclusion rather than a positive diagnosis. The common clinical presentation is of recurrent, angina-like retrosternal pain that, through appropriate cardiac workup (based on risk factor profile), has not been determined to be due to a cardiac cause.1 Although the prevalence of NCCP varies between studies and populations, it is a common problem, with an estimated prevalence of approximately 13% (95% confidence interval: 9%, 16%) globally.6 Even once cardiac causes have been ‘excluded’, the differential diagnosis remains broad;1,3,7 ironically, in some cases, cardiac disease does turn out to be the cause of the symptoms.8
This review focuses on gastrointestinal conditions to be considered in patients with a diagnosis of NCCP, including gastro-oesophageal reflux disease (GORD) and oesophageal dysmotility, as well as functional causes, their workup and key management aspects (Figure 1). The focus is on issues related to primary care where, given the wide differential diagnosis and potential range of specialists/tests involved, care is appropriately coordinated and delivered.
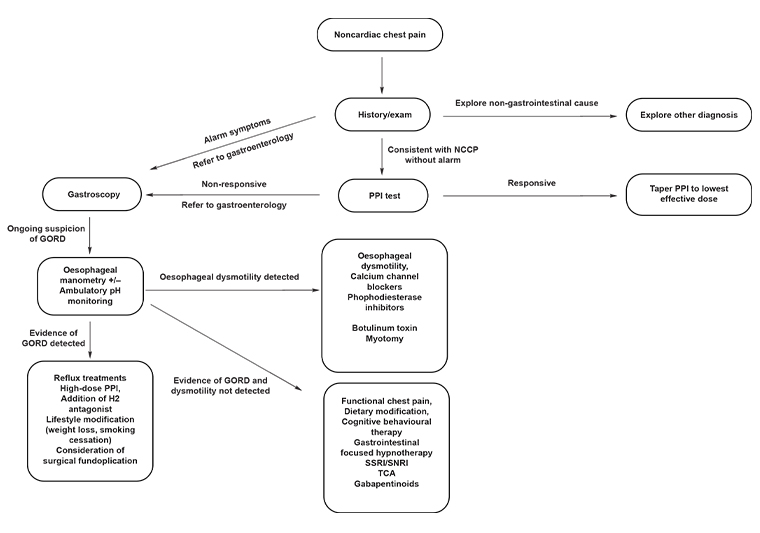
Figure 1. Diagnostic and management algorithm for noncardiac chest pain. Click here to enlarge.
GORD, gastro-oesophageal reflux disease; NCCP, noncardiac chest pain; PPI, proton pump inhibitor; SNRI, selective norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant
Evaluation of noncardiac chest pain
NCCP describes angina-like or atypical chest pain, deemed not to be caused by underlying cardiac disease, and is typically diagnosed either by an emergency physician or cardiologist.1,9 The differential diagnosis of chest pain, both angina-like and atypical, covers a broad range of possibilities including pulmonary, musculoskeletal, neurological, functional, psychiatric and gastrointestinal disorders (Table 1). The pain episode may occur as a single event or be one in a recurrent series, with the prognosis ranging from benign to life threatening.
NCCP is commonly attributed to gastrointestinal causes, likely because of both their high prevalence and clinical features with similarities on history to cardiac angina,9 although the differential diagnosis remains wide. A focused history and clinical examination may provide clues to the underlying cause but are frequently nondiagnostic. Features on history suggestive (but not specific) for oesophageal causes include dysphagia, regurgitation and heartburn.7,10 Other features that may suggest alternative causes include dyspnoea, pleurisy, underlying anxiety disorder, recent trauma and focal tenderness on examination.
Excluding cardiac chest pain
What defines an adequate exclusion of cardiac chest pain is beyond the scope of this review; however, excluding cardiac chest pain is the most important aspect of the diagnosis, workup and treatment of chest pain and must, by definition, have occurred before NCCP can be ‘diagnosed’.8 Atypical features on initial assessment are not sufficient to exclude chest pain of cardiac origin. Special attention should be given to patients with traditional cardiac risk factors, as patients with NCCP with these risk factors demonstrate increased rates of cardiovascular mortality than those without.11 Eslick and Talley demonstrated a reduced but still not insignificant cardiac mortality rate of 5.5% in patients with NCCP at four years, compared with 11% of patients with diagnosed coronary artery disease,10 and Mol et al12 found a prevalence of 5.1% in major cardiac events at one-year follow-up. Nonocclusive coronary artery pathology such as coronary syndrome X (microvascular angina) and vasospastic angina can be missed during cardiac workup.8 Hence a degree of diagnostic uncertainty remains, and vigilance needs to be maintained when a patient has associated cardiac risk factors and changes in pain quality or development of new associated features consistent with coronary artery disease, which could prompt reconsideration.
Gastro-oesophageal reflux disease
Atypical manifestations of GORD are the most common gastrointestinal cause of NCCP.6 The prevalence of GORD as a cause of NCCP is believed to be between 30% and 60%, depending on the population.9 As it is the most common underlying cause, and as the workup and management of GORD are low cost and low risk, this should be the first condition considered in the management of NCCP.
In the absence of red flags that would indicate more urgent referral for consideration of upper gastrointestinal (GI) endoscopy (Box 1), an appropriate initial step is to perform a proton pump inhibitor (PPI) test, which has an acceptable sensitivity and specificity (both approximately 80%) in establishing GORD as the likely underlying cause of NCCP.13 The precise details (dose of PPI and duration) are not standardised; however, the principle is to suppress oesophageal acidification as completely as possible for a long enough period to make a robust assessment of the effect, with a positive test indicated by a >50% reduction in symptom severity. The duration of the trial will need to be tailored to the frequency of the patient’s symptoms; the effect on daily symptoms will be able to be assessed with a shorter duration of trial than symptoms that occur infrequently. Generally, eight weeks of double-dose (eg pantoprazole 40 mg twice daily) PPI is sufficient in most cases. If symptoms are intermittent or the response is unclear, it may be necessary to repeat the test (with a further observation period between PPI trials) to be sure that the symptoms are indeed improved when on the PPI when compared with off the PPI (sometimes with a symptom diary).
| Box 1. Indications for endoscopy in noncardiac chest pain |
- Red flags
- Dysphagia
- Odynophagia
- Gastrointestinal bleeding/unexplained iron deficiency anaemia
- Unintentional weight loss
- Recurrent vomiting
- Failure to respond to trial of therapy
|
If patients fail to respond to PPI therapy, further investigation of the upper gastrointestinal tract is an important consideration. As the patient by definition has ongoing symptoms that have failed to respond to a trial of treatment, upper gastrointestinal endoscopy is likely to be required, unless this was previously performed on the basis of red flags. If the PPI trial has been effective, the patient may remain on the PPI for the endoscopy; if the PPI has not been effective, it should be ceased, and the patient can undergo the procedure after they stop taking the PPI (after eight weeks unless there is a red flag suggesting more urgency). In any case, the results of the endoscopy should be interpreted with consideration of the knowledge of the PPI history of the patient. During the upper gastrointestinal endoscopy, oesophageal biopsies should be taken to examine for histological evidence of gastroesophageal reflux and for eosinophilic oesophagitis, which is thought to be an under-recognised cause of NCCP.1,9,14 In addition to the reflux itself, other common associations of GORD, such as hiatus hernia, may cause intermittent chest pain. This is particularly seen with paraoesophageal hiatus hernia, where the rolling paraoesophageal component may compress the lower oesophagus or occasionally become incarcerated.
Treatment
If the chest pain responds to the trial of high-dose PPI, underlying GORD is the presumptive cause for the chest pain, and the minimum effective dose of acid suppression can be determined by dose titration with ongoing maintenance at the lowest dose consistent with adequate control of symptoms. The ongoing need for PPI can be tested by intermittent withdrawal or dose reduction in 6–12 months and occasionally thereafter. In the presence of typical symptoms of reflux (heartburn +/– regurgitation), control of these will be an additional consideration in the ongoing use of acid suppression.
Lifestyle modifications such as weight loss and tobacco cessation are suggested as adjuncts for GORD, but there are only limited data informing their effect on chest pain.15 Despite being worthy of recommendation in their own right, these lifestyle medications may not be effective as sole therapy.
If patients remain refractory to treatment, referral to a gastroenterologist is recommended to consider further investigation (eg ambulatory pH monitoring) and treatment, such as surgical fundoplication16 if GORD can be convincingly established as the cause of symptoms.
Oesophageal dysmotility
Features such as dysphagia should prompt consideration of oesophageal dysmotility. Hypercontractile disorders – such as nutcracker oesophagus, achalasia and distal oesophageal spasm – have been implicated as causes of NCCP. As dysmotility may be precipitated by acid reflux, and dysphagia is an indication for endoscopy, investigation for these disorders with oesophageal manometry will usually be preceded by upper gastrointestinal endoscopy and a trial of a PPI. Estimates of oesophageal manometric abnormalities range between 6% and 33%.9 Although the most common abnormality found is hypotensive lower oesophageal sphincter tone (suggestive of GORD), oesophageal manometry has been estimated to find a specific cause of chest pain in approximately 10% of patients.9
Despite the relatively low prevalence of specific abnormalities, oesophageal manometry represents the best tool to identify oesophageal dysmotility as a cause of NCCP and may lead to more definitive therapy (eg achalasia). If the history is suggestive and oesophageal manometry is not easily available, barium swallow is an alternative. Although the diagnosis of ‘presbyoesophagus’ is a rather meaningless and ill-defined radiological term, specific features of achalasia or oesophageal spasm will be of diagnostic value.
Treatment
Medical management of NCCP due to oesophageal dysmotility (ie hypercontractile disorders such as oesophageal spasm) focuses on medications aimed at reducing oesophageal contractility; however, the quality of evidence supporting these therapies is low.17 Medications used include calcium channel blockers (nifedipine/diltiazem) and those acting via nitric oxide such as nitrates (glyceryl trinitrate) and phosphodiesterase inhibitors (sildenafil).17 In practice, these are often poorly tolerated because of their side-effect profiles; however, if the patient is taking antihypertensive medication and is not constipated, there may be an opportunity to switch to a calcium channel blocker to take advantage of the dual action. The duration of a trial of any of these medications should (similar to the PPI trial) be tailored to the frequency of symptoms. If symptoms are infrequent, a longer trial of medication will be required to demonstrate efficacy. Before committing to ongoing therapy, observation of symptoms off acid suppression may be necessary to convincingly demonstrate treatment efficacy. If symptoms are infrequent and respond to as-needed therapy, that may be all that is required, whereas if symptoms are frequent, regular medication is likely to be more effective overall.
Second-line therapies for distal oesophageal spasm and achalasia include botulinum toxin injection and/or myotomy,9 and patients should be referred to a gastroenterologist for consideration.
Functional chest pain
Functional chest pain is thought to be related to oesophageal hypersensitivity and pain sensitisation processes.9 It is often a further diagnosis of exclusion in the workup of NCCP requiring negative gastroscopy, with no evidence of gastro-oesophageal reflux or oesophageal dysmotility.9 The cause of functional chest pain is not fully understood but may relate to oesophageal hypersensitivity to physiological events (swallowing, subclinical reflux) caused or made worse by anxiety. This may cause a vicious spiral whereby the anxiety itself precipitates further chest pain, resulting in greater anxiety. This is then exacerbated by the absence of a definitive diagnosis, lack of validation of symptoms or concern that underlying disease has been overlooked. In addition to the exclusion of underlying conditions, other factors may be suggestive of functional chest pain as the underlying aetiology. Up to 20% of patients display symptoms of other functional gastrointestinal disorders, such as irritable bowel syndrome (27%) and abdominal bloating (22%).3 Contributing psychological factors are also found in up to 75% of patients, >50% of whom have panic disorder, anxiety or major depression.3 These factors are not significantly discriminatory to allow for a diagnosis without adequate workup3 but will warrant treatment in their own right.
Treatment
There is no universally accepted and effective treatment for functional chest pain; however, the principles of treatment are the same as for other functional gastrointestinal disorders. This includes:
- clear explanation of the diagnosis and underlying physiology (brain–gut axis)
- reassurance as to the non–life threatening nature of the underlying condition
- identification of precipitating and exacerbating factors
- appropriate non-pharmacological therapy (dietary, lifestyle and psychological – cognitive behavioural therapy or gut-focused hypnotherapy)
- appropriate low-risk pharmacological therapy with neuromodulators and non-opioid analgesics, an approach very similar to chronic pain management.
If medication is required (especially in the presence of depression and or anxiety), selective serotonin reuptake inhibitors (SSRIs), selective norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants, theophylline and gabapentinoids have all been shown to have some benefit.9,17 The SNRI venlafaxine (75 mg daily) and the SSRI sertraline (50–200 mg daily) have the strongest (moderate-grade) evidence supporting their use,17 with the most practical application in clinical practice. Theophylline also has moderate evidence of efficacy; however, the side-effect and toxicity profiles limit its use in clinical practice. Psychological therapies including cognitive behavioural therapy are also likely to be helpful, particularly (but not exclusively) where anxiety is a contributing factor. A range of alternative therapies is also available and (provided they are of low risk) may be worth trialling if more conventional therapies have not provided sufficient benefit.17
Other causes
Other causes of NCCP should be considered if features are atypical (Table 1). Musculoskeletal causes of chest pain should be considered prior to a potentially unnecessary and costly series of investigations. The diagnosis of musculoskeletal chest wall pain is reliant on good clinical history and examination, given the lack of a gold standard diagnostic test. Useful features include tenderness to palpation and positional changes in symptoms.
| Table 1. Potential conditions that can be associated with atypical ‘noncardiac’ chest pain* |
| Gastrointestinal |
Common:
- Gastro-oesophageal reflux disease†
- Oesophageal spasm/dysmotility†
- Functional chest pain†
- Biliary pathology†
Rare:
- Other causes of oesophagitis (pill, eg doxycycline; infective)
- Oesophageal rupture (Boerhaave syndrome)‡
|
| Musculoskeletal |
Common:
- Intercostal muscle strain†
- Costochondritis
- Fibromyalgia
|
| Respiratory |
Common:
- Pneumonia
- Pleurisy
- Pulmonary embolism‡
- Pneumothorax†,‡
|
| Neurological |
Common:
Rare:
|
| Cardiovascular |
Common
- Coronary artery disease†,‡
- Pericarditis
Rare:
|
| Psychiatric |
Common:
Rare:
- Somatisation symptom disorder†
|
*List is not extensive, and relative prevalence or significance is not implied by order.
†More likely to be recurrent, potentially mimicking atypical angina
‡Potentially acutely life-threatening causes |
Other gastrointestinal causes not discussed in this article include oesophagitis, oesophageal rupture (Boerhaave syndrome) and biliary pathology (biliary colic). These are usually clinically distinct with suggestive features on history and examination (varying extensively on the basis of underlying pathology) but can present with lower retrosternal symptoms.
Conclusion
NCCP is a challenging condition characterised by diagnostic uncertainty and may be associated with considerable morbidity and healthcare use. Once cardiac disease has been (as far as possible) excluded with appropriate investigations based on risk factor profile, common causes include GORD, oesophageal hypercontractility (spasm), musculoskeletal causes, functional disorders and anxiety, which are often treated empirically as investigation is commonly non-contributory. Upper gastrointestinal endoscopy may be indicated on the basis of symptom profile or response to treatment. Oesophageal manometry has a low yield but may show features of hypercontractile disorders.
Key points
- Excluding a cardiac cause of chest pain is essential prior to the ‘diagnosis’ of noncardiac chest pain, and even then remains a diagnostic possibility.
- Gastroscopy is only required in the presence of red flags.
- A trial of PPI therapy is often a helpful first step in patients without features indicating early gastroscopy and can be managed in the primary care setting.
- If the PPI trial is positive, the dose of PPI should be optimised/minimised.
- Management of functional chest pain follows the same principles as for other functional gastrointestinal disorders and chronic pain syndromes.