Common warts (Verruca vulgaris), plantar warts (Verruca plantaris) and flat/plane warts (Verruca plana), collectively known as cutaneous warts, are benign growths of the skin caused by the human papillomavirus (HPV). In Australia, up to 24% of children and 5% of adults are affected.1
A break in the epidermal barrier of the skin allows entry of HPV and subsequent infection of basal epithelial cells. HPV replicates alongside the natural lifecycle of epithelial cells, and is eventually released from desquamated keratinocytes on the surface of warts, potentially infecting other sites via direct contact or through fomites.2
Cutaneous warts generally self-resolve. Up to two-thirds of immunocompetent children experience spontaneous clearance of their cutaneous warts by two years of age.3 Adults tend to take longer. Patients might request treatment for their warts when they cause discomfort, functional impairment, social ostracism, are numerous, grow large or raise concerns regarding transmission.4
Treatment for cutaneous warts can be painful, scar, cause pigmentary disturbances and might not be effective.5 Therefore, clinicians should be wary of the evidence behind the efficacy of cutaneous wart treatment. This review summarises high-quality studies investigating the efficacy of chemical and physical destructive wart therapies.
Methods
We performed a literature review (up to June 2021) of published articles for wart management from the MEDLINE and Embase databases. No language restrictions were applied. We considered systematic reviews, randomised controlled trials (RCTs), cohort studies and case series. Case reports were excluded. For MEDLINE, we used the Boolean operation to combine MeSH terms ‘warts’ AND ‘therapeutics’. For Embase, we used the Boolean operation to combine MeSH terms ‘Verruca vulgaris’ AND ‘therapy’. We included studies that investigated chemical or physical destructive therapies.
Results and discussion
Non-pharmacological therapies
To attenuate transmission, hygienic practices need to be adopted in conjunction with any treatment. This includes not sharing personal items, wearing protective footwear in communal areas and not scratching warts. Checking the soles of feet regularly will help identify early lesions, which are easier to treat.6
Pharmacological therapies
Treatment options can be categorised into chemically destructive, physically destructive, antiproliferative or immunostimulatory. Table 1 provides an overview of the evidence supporting treatment options in the management of cutaneous warts.
| Table 1. Evidence supporting chemical and physical destructive treatment options in the management of cutaneous warts |
| Method of destruction of epithelium |
Evidence to support efficacy |
| Paediatric |
Adult |
| Common wart |
Plane wart |
Plantar wart |
Common wart |
Plane wart |
Plantar wart |
| Salicylic acid |
Yes7 |
|
Yes7 |
Yes7 |
|
Yes7 |
| Cryotherapy |
Yes8 |
|
Yes8 |
Yes8 |
|
Yes8 |
| Silver nitrate |
Yes9 |
|
Yes10 |
Yes9 |
|
Yes10 |
| Phenol |
Yes11 |
|
|
Yes11 |
|
|
| Cantharidin |
Yes12,13 |
Yes12 |
Yes13 |
Yes12,13 |
Yes12 |
Yes13 |
| Glycolic acid |
|
Yes14 |
|
|
|
|
| Pyruvic acid |
|
|
Yes15 |
|
|
Yes15 |
| Citric acid |
|
Yes16 |
|
|
Yes16 |
|
| Formic acid |
Yes18 |
|
Yes18 |
Yes17 |
|
Yes17 |
| Trichloroacetic acid |
Yes20 |
Yes19 |
|
Yes20 |
Yes19 |
|
| Monochloroacetic acid |
Yes21 |
|
Yes21 |
Yes21 |
|
Yes21 |
| Zinc oxide |
Yes22,23 |
|
Yes22 |
Yes22,23 |
Yes23 |
Yes22 |
| Laser |
Yes25,26 |
Yes25,26 |
Yes24–26 |
Yes25,26 |
Yes25,26 |
Yes24–26 |
| Surgical removal |
|
|
|
|
|
|
| Electrosurgery |
|
|
|
|
|
|
Chemical destructive therapies
Damaging or destroying the infected epithelium causes HPV cell death. The subsequent antigen exposure and presentation might also induce an immune response.
Salicylic acid
Salicylic acid chemically debrides the wart of excess keratin and induces an inflammatory response. A meta-analysis of six RCTs demonstrated that topical salicylic acid was more effective than placebo for cutaneous warts at all sites (relative risk [RR]: 1.56; 95% confidence interval [CI]: 1.20,2.03).7 In the largest study, the investigators pared down the surface of the wart before applying 40% salicylic acid daily for up to 13 weeks.8 Salicylic acid should not be applied to areas of poor healing nor the face due to risk of chemical burns.7
Cryotherapy
Cryotherapy with liquid nitrogen causes direct cell damage and subsequent inflammatory response (Figure 1B). A meta-analysis of three RCTs surprisingly found no evidence to suggest that cryotherapy was different to placebo in the treatment of cutaneous warts (RR: 1.45; 95% CI: 0.65, 3.23).7 However, the largest study achieved a cure rate of 39% and an RR of 2.49 (95% CI: 1.41, 4.41) compared with active surveillance.8 The participants received three serial applications of liquid nitrogen in one session every fortnight for up to 13 weeks.8 Side effects included pain, blistering of the affected sites, and post-inflammatory hypopigmentation or hyperpigmentation.7 Although not common if performed by a well-trained professional, clinicians should caution their patients that annular recurrence (ring wart) might occur due to damage of surrounding tissue facilitating the spread of HPV (Figure 1C).

Figure 1. Cryotherapy for the treatment of cutaneous warts
A. Plantar wart. B. Four sessions of fortnightly cryotherapy achieving complete remission. C. Ring warts on the elbow after two sessions of cryotherapy.
Silver nitrate
Silver nitrate is a chemical cauteriser.9 A recent RCT investigating weekly applications of 95% silver nitrate for the treatment of Verruca pedis in adults found complete response in 37.5% of participants after 10 weeks.10 In a placebo-controlled randomised trial of 10% silver nitrate solution applied alternate daily for three weeks, complete regression of palmar and plantar lesions was achieved in 63% of adults and children. Participants experienced a mild-to-moderate burning sensation, itching and temporary discolouration of the skin.9
Phenol
Phenol is a caustic agent. In a trial of common warts of the hand comparing 80% phenol solution to cryotherapy in adults and children, weekly intervention demonstrated complete clearance of warts in 82.6% of phenol participants and 70% of cryotherapy patients after six weeks.11 There was no statistically significant difference between the two methods (P = 0.14). Pain and pigmentary changes were noted in the phenol group.
Cantharidin
Cantharidin is a vesicant that causes acantholysis and subsequent destruction of epithelial cells (Figure 2). A 2018 systematic review of cantharidin monotherapy for cutaneous warts found four studies evaluating topical cantharidin 0.7% monotherapy treatment of warts in adults and children, including 576 patients with 525 total lesions.12 A 2018 systematic review of topical cantharidin 0.7% for cutaneous warts found complete remission rates of up to 90.8%.12 In a 2019 case series investigating topical application of cantharidin 1% podophyllin 2% salicylic acid 30% solution (CPS1), complete clearance of warts occurred in 86.5% of children and 62.7% of adults treated with CPS1 solution.13 The solution was applied at intervals of 3–4 weeks, and blistering was common.13
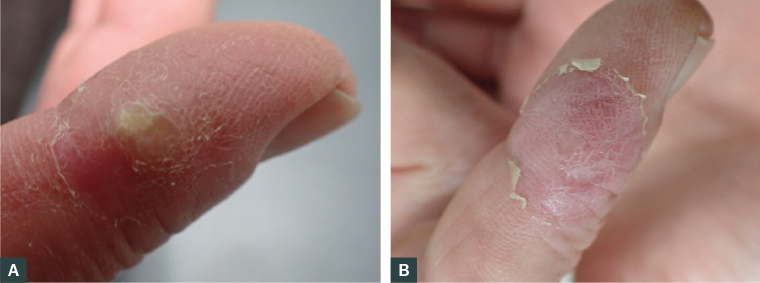
Figure 2. A. Before and B. after a single session of cantharidin treatment
Glycolic acid
Glycolic acid is an alpha-hydroxy acid with keratolytic properties. Topical 15% glycolic acid plus 2% salicylic acid gel applied once daily to recalcitrant facial flat warts in participants aged 7–16 years resulted in complete remission in 13 of 20 patients after eight weeks of treatment.14
Pyruvic acid
Pyruvic acid is an alpha-hydroxy acid with strong keratolytic properties. In an RCT investigating plantar warts in participants aged >12 years, pyruvic acid 70% was compared with compound salicylic acid solution (salicylic acid 16.7%, lactic acid 16.7% and collodion 100%) that was topically applied twice a day for four weeks. There was no difference in clearance between therapies; wart number decreased by 13% with pyruvic acid and by 23% with compound salicylic acid (P = 0.16) after treatment.15 Adverse events in both groups included pain, a burning sensation and pigmentary changes post-treatment.
Citric acid
Citric acid has keratolytic and disinfecting properties.16 In a blinded intraparticipant study investigating plane warts on the body, 50% citric acid aqueous solution was compared with tretinoin lotion applied twice daily.16 After six weeks, the authors found a clinically significant improvement of 64.45% in the citric acid side compared with 53.7% in the tretinoin side of the patient (P <0.05).16 Adverse events included burning or stinging sensation, erythema and pruritus.16
Formic acid
Formic acid acts similarly to formalin by dehydrating and finally destroying the infected tissue. A case series of adults with recalcitrant Verruca vulgaris treated with a proprietary product, in which the pen was applied on each wart for 30 seconds twice weekly for six weeks, reported that 42.8% of participants achieved complete remission.17 In a study of paediatric patients with common warts located on the scalp, hands, trunk and feet, 85% formic acid was applied on alternate days for up to four weeks. Complete remission was achieved in 81% of participants after the study period.18
It should be noted that chemical burns have occurred from the application of topical acid-based products, including formic acid, salicylic acid, monochloroacetic acid and glutaraldehyde. Most of these occur in the paediatric population.5
Trichloroacetic acid
Trichloroacetic acid (TCA) is a caustic agent that destroys warts by chemical coagulation of proteins. In an RCT investigating Verruca plana in children and adults, weekly applications of TCA were compared with weekly cryotherapy sessions over an eight-week period. The investigators observed total remission in 85.7% of participants treated with 10% TCA, 92.6% of participants treated with 25% TCA and 92% of participants treated with cryotherapy.19 There was no evidence to suggest a difference in treatment outcomes between the three groups. Adverse events in the TCA group included itch, pain, erythema, erosions, bullae and hyperpigmentation.
Pezeshkpoor et al compared the efficacies of 80% TCA and 35% TCA in the treatment of common warts. At the end of the six-week study, 46.7% of participants achieved a good response (>75% of lesions cleared) in the 80% TCA group compared with 12% in the 35% TCA group.20
Monochloroacetic acid
Monochloroacetic acid (MCA) is a caustic agent that destroys warts by chemical coagulation of proteins.
In an RCT investigating Verruca vulgaris and Verruca plantaris in individuals aged six years and over, 76% MCA was used every two weeks in a 13-week study. For the treatment of Verruca vulgaris, MCA achieved complete remission in 43% of patients compared with cryotherapy (54%), with no evidence to suggest a difference. In the treatment of plantar warts, MCA achieved a cure rate of 46% compared with combination therapy with salicylic acid (39%), which again demonstrated no difference.21 Blistering and irritation were common adverse events associated with MCA.21
Zinc oxide and nitric–zinc complex solution
Zinc oxide and nitric–zinc complex solution (NZCS) is a topically applied solution that induces a painless caustic effect.22 In a small case series of palmoplantar or periungual wart in children and adults, NZCS was applied every two weeks for a median of six applications. The investigators found complete resolution in 83.9% of the warts treated with NZCS with six treatment sessions with no adverse effects.22
A 2007 RCT investigating 20% zinc oxide ointment compared with salicylic acid 15% and lactic acid 15% ointment twice daily for up to three months for patients >12 years of age with cutaneous warts demonstrated 50% complete remission.23 The authors reported ‘mild and local’ side effects.
Physical destructive therapies
Laser
CO2 lasers emit infrared light at 10,600 nm and act to destroy the epidermis. A recent small RCT comparing CO2 laser with cryotherapy demonstrated no significant difference in the resolution of warts in both groups; remission rate was 89.7% in the laser group and 70.4% in the cryotherapy group (P = 0.069).24 Scarring, hypopigmentation, postoperative pain and prolonged wound healing are adverse effects of CO2.25
The erbium-doped yttrium aluminium garnet (Er:YAG) laser emits a wavelength of 2940 nm and causes direct ablation of the epidermis. In four non-randomised trials, Er:YAG lasers achieved a resolution rate of 72–100% for cutaneous warts.25 Adverse effects were limited to discomfort during treatment and erythema.25
The neodymium-doped yttrium aluminium garnet (Nd:YAG) laser emits a wavelength of 1064 nm and destroys wart dermal blood vessels. Complete response rates of 46–100% have been reported for simple and recalcitrant common, palmoplantar, periungual and subungual warts.25 Adverse events included hematoma, secondary bacterial infection and severe pain.25
Newer modalities of laser therapy, such as pulsed dye lasers (PDL), are more subtle and can destroy the dilated superficial capillaries, rather than the tissue itself, and reduce complications.25 PDL therapy has been used to treat simple and recalcitrant common, palmar, plantar and flat warts, with variable remission rates ranging from 47% to 100%.25 Complications are uncommon, but include topical discomfort and erythema.26
The number of laser passes used depends on the depth of the lesion, but studies have reported using 2–4 passes per wart.25
Surgical removal
Excisional surgery is used in certain cases, but it is generally avoided because of its invasive nature, potential for significant scarring and recurrence of lesions in up to 30% of cases.27 The primary surgical excision of a wart is not recommended.28
Electrosurgery
Removal of warts by curettage, followed by cautery, has been reported to have success rates of 65–85%, but scarring and recurrence occur in up to 30% of patients.29 To the best of our knowledge, there are no published RCTs for this treatment.7 Clinicians should be cautious while operating electrocoagulation, as HPV DNA has been demonstrated in vapours.30
Conclusion
Very few of the treatment options discussed here have been tested by RCTs. Clinicians should consider the location and type of cutaneous wart, the evidence supporting the proposed treatment, potential adverse effects of treatment, as well as patient comorbidities when considering treatment options. Appropriate and effective treatments in primary care generally include salicylic acid and cryotherapy. Resistant cases may require referral for the more specialised options summarised in this article.