In Australia, one in four pregnancies is unintended.1 Half of these pregnancies occur in Australian women using contraception at the time of conception;2 this suggests issues with patient adherence and/or failures in contraceptive methods of choice.3 Male condoms and the combined oral contraceptive pill are the most common forms of contraception used by Australian women and have typical use failure rates of 9% and 18%, respectively.4 However, intrauterine devices (IUDs) are over 99% effective at preventing pregnancy, with failure rates of between 0.05% and 0.8%.4,5 Despite their efficacy, safety and high patient satisfaction,6 the uptake of IUDs in Australia remains low, with only 6.3% of women using hormonal IUDs (also known as ‘intrauterine systems’) and even fewer using copper IUDs.7,8 This makes women vulnerable to unwanted pregnancy as they rely on less effective and less reliable contraceptive methods.
General practice is ideally placed to provide and improve access to IUD services as a first-line setting for family planning, the provision of contraceptives and for managing the sexual and reproductive health concerns of Australians. However, there are a limited number of general practitioners (GPs) who are experienced in IUD insertion in Australia,9 and those that are might have their contraceptive advice and provision influenced by their personal perceptions, misconceptions and experiences of contraception.10 Practitioner misconceptions influence service delivery by preventing eligible women from obtaining an IUD or delaying insertion. For example, practitioners might delay or extend the IUD journey due to perceptions about performing and awaiting sexually transmissible infection (STI) screening results before insertion, and their own preference in service delivery. Additionally, when consulting with adolescents, some practitioners might be hesitant to offer IUDs due to misperceptions about higher STI risk with IUD use in this demographic.11,12 However, international guidance recommends that insertion should not be delayed while awaiting STI test results and screening can occur the day of insertion.13 If a positive test result occurs, then treatment can be undertaken without removal of the IUD.13
Clinical and practitioner-based barriers (eg providers’ knowledge of the medical eligibility criteria for IUD insertion, a lack of access to IUD insertion training and costs) hinder IUD services.14,15 Best practice might be limited by complicated and outdated clinic protocols that prevent the option of same-day insertion.16,17 Studies suggest that providers who are educated about long-acting reversible contraception (LARC) misconceptions are more likely to provide same-day LARC services.16,18,19 Additionally, when same-day insertion delivery models are provided, women are receptive to this option.19,20
To understand the reasons for the low IUD uptake in Australia, models of care (MoC) must be explored. It is essential when describing MoC to understand the quality of care being delivered. This includes the extent to which current evidence and misconceptions affect service delivery. A summary of best practice for patient access to IUD services is shown in Figure 1, and will inform the quality assessment of the IUD MoC discussed by the study participants. Unlike the clinical areas of mental health and arthritis,1,24 there is little documentation about MoC for GP IUD provision in the literature. Therefore, the aim of this study was to determine and describe the MoC used in the provision of IUDs by Australian GPs.
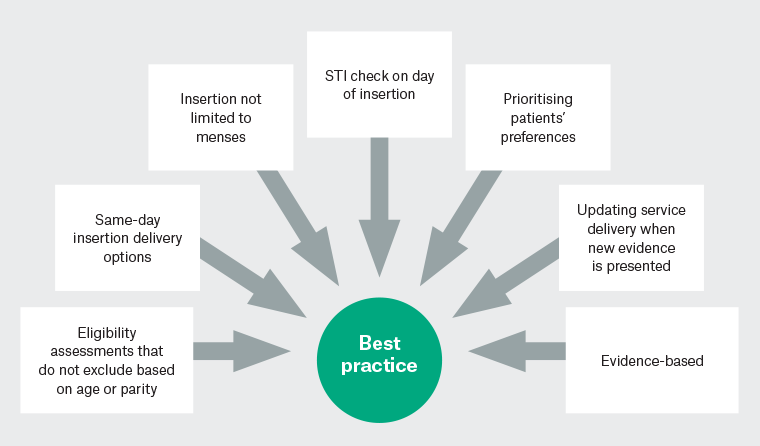
Figure 1. Best practice for general practitioner-provided intrauterine device provision services that improve patient access.10,14,21–23
STI, sexually transmissible infection.
Methods
We used a qualitative descriptive approach, which is underpinned by pragmatism, to describe participants’ experiences. A qualitative descriptive approach can be used to synthesise theories in qualitative research, which can then guide practice.25 The Quality framework for Australian general practice26 was a guiding principle to this approach. This conceptual framework has previously been used to describe MoC in the delivery of medical abortion in Australian general practice.27 The framework includes six dimensions to assess the quality of a service provided within general practice (Table 1),28–31 and informed the present study design, data collection and analysis.
| Table 1. Quality dimension definitions |
| Quality dimension |
Definition |
| Acceptability |
Patient is satisfied with the service, and their needs and preferences are met and appropriate to the social context28,30 |
| Accessibility |
Healthcare service is timely and geographically reasonable, appropriate skills and resources are present28 |
| Appropriateness |
The financial aspects of the service, such as costs to the healthcare provider and the patient, are suitable29,30 |
| Effectiveness |
The service is guided by evidence-based information and the patient’s health is improved28,31 |
| Efficiency |
The health service is not wasteful of equipment, ideas, supplies or energy31 |
| Safety |
The health service provides the least harm possible to the patient28,31 |
The lead author and interviewer (LM) is a young, female, Bachelor of Biomedical Sciences Honours student. It was possible that her characteristics and past experiences in women’s health and general practice might influence data collection, so reflexivity underpinned the research process to minimise bias.
Sampling
Participants were recruited via purposive and convenience sampling methods between June and August 2021. Purposive sampling was used to identify GP IUD providers through, for example, opt-in healthcare directories (eg 1800 My Options [www.1800myoptions.org.au] and HealthEngine [https://healthengine.com.au]); convenience sampling was also used through mechanisms such as social media advertisements, Monash University newsletters, Centre of Research Excellence for Sexual and Reproductive Health for Women in Primary Care and Monash University working groups and snowballing. GPs who currently provide IUD insertions in a general practice setting were included in the study. Those GPs who solely provide IUDs outside of the general practice setting were excluded. No participants withdrew from the study or refused to participate.
Data collection
After 18 participant interviews, no new data were identified. Two subsequent interviews were then undertaken to confirm data saturation. In all, 20 semistructured interviews were conducted one-on-one via telephone by LM with an average interview duration of 40 minutes (range 27–60 minutes). Verbal consent was obtained before interview commencement.
The development of the interview guide was informed by the quality framework26 to ensure questions focused on the quality of service delivery (Appendix 1). Two pilot interviews were undertaken with GP academics, with no modifications required after the pilot interviews. The interview guide included questions about participants’ IUD delivery models, how they initiated service delivery, difficulties with being a GP IUD provider and perspectives on how IUD services could be improved. Field notes were made after each interview and transcripts were not returned to participants for comment. No repeat interviews were required. Interviews were transcribed verbatim and deidentified by LM. Data were stored and managed in NVivo 20 (QSR International, Denver, CO, USA). Participants received $150 gift cards upon completion of the interview.
Data analysis
Data coding was completed by two researchers (LM and RS) using reflexive thematic analysis guided by Braun and Clarke32 (Appendix 2). There are six phases of thematic analysis.32 First, familiarisation occurred naturally via data through data transcription and rereading transcripts. Second, NVivo facilitated code and subcode generation, indicative of notable elements in the data, such as IUD model structure and the dimensions of the quality framework.26 LM and RS coded five transcripts independently and then discussed coding discrepancies to create a final coding scheme, which was used by LM to code the remaining transcripts. Third, codes were assigned into potential themes, which were then reviewed by all four researchers to assess whether they concurred with the broader data set (Step 4). Codes and subcodes that related to service delivery were accumulated under the IUD service delivery theme and relevant subthemes. Quality dimensions26 were listed against subthemes and used to assess the quality of each component of the MoC and the MoC overall (eg the extent to which appointment numbers of each MoC faciliated or prevented access). Themes were defined and named, and the final analysis and write-up of the report were completed in the form of the student researcher’s Honours thesis. This study was approved by the Monash University Human Research Ethics Committee (No. 28928).
Results
Twenty participants from six states were interviewed (Table 2). Interviews ranged in duration from 27 to 60 minutes (mean 40 minutes). Participants mostly identified as women, with a mean age of 38 years, a mean of 6.7 years working as a GP, a mean of 5.4 years providing IUDs and practising mostly in metropolitan areas.
| Table 2. Demographic characteristics of participants |
| Characteristic |
Variable |
n |
% |
| Gender identification |
Woman |
17 |
85 |
| Man |
3 |
15 |
| Age (years) |
25–29 |
1 |
5 |
| 30–39 |
13 |
65 |
| 40–49 |
6 |
30 |
| Remoteness of practiceA |
Metropolitan |
12 |
60 |
| Inner regional |
6 |
30 |
| Outer regional |
2 |
10 |
| State |
New South Wales |
4 |
20 |
| Queensland |
3 |
15 |
| South Australia |
3 |
15 |
| Tasmania |
2 |
10 |
| Victoria |
7 |
35 |
| Western Australia |
1 |
5 |
| Years as a registered GP |
0–<5 |
7 |
35 |
| 5–<10 |
11 |
55 |
| 10–<15 |
2 |
10 |
| Years as an IUD provider |
0–<3 |
8 |
40 |
| 3–<5 |
4 |
20 |
| 5–<10 |
5 |
25 |
| 10+ |
3 |
15 |
| General practice clinic billing typeB |
Private |
7 |
35 |
| Bulk billing |
4 |
20 |
| Mixed |
10 |
50 |
| No. IUDs inserted per month in general practice |
1–<3 |
8 |
40 |
| 3–<5 |
5 |
25 |
| 5–<10 |
4 |
20 |
| 10–<15 |
3 |
15 |
ARemoteness of practice was determined using the Health Workforce Locator Tool, with the Australian Standard Geographical Remoteness Areas 2016 classification (www.health.gov.au/resources/apps-and-tools/health-workforce-locator/health-workforce-locator).
BOne general practitioner (GP) provided intrauterine devices (IUDs) in two separate practices, both within the same suburb but with different billing types. |
GP MoC for IUD provision
Three models of IUD provision were identified: common, streamlined and same-day insertion models (Figure 2). Participants also described task-sharing arrangements and model adaptations that facilitated service delivery and flexibility for both providers and patients. Although each participant identified using one main MoC for IUD provision, some operated multiple models concurrently within their practice. Participants also discussed task-sharing arrangements and adaptations to service delivery.
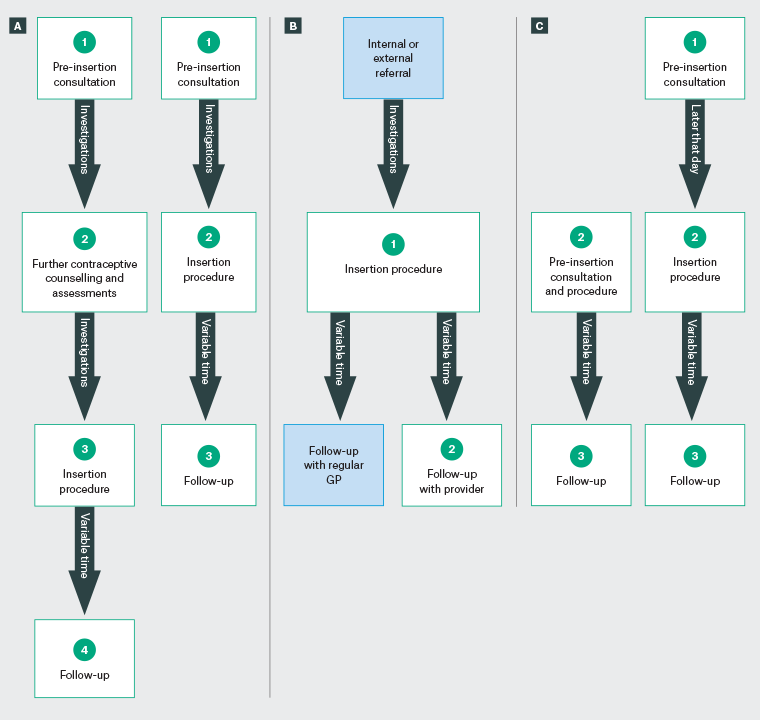
Figure 2. Appointment flow for three models of care for the provision of intrauterine devices in general practice, namely (A) common, (B) streamlined and (C) same-day insertion. Click here to enlarge
Pre-insertion assessments discussed by participants include urine and blood tests, cervical screening, pap smears, sexually transmissible infection checks, internal examinations, tolerance to a speculum and visual cervical os assessment. ‘Variable time’ represents the time between the insertion procedure and the follow-up appointment, which varied between two and six weeks.
GP, general practitioner.
Model 1: Common model (three to four appointment pathways)
The common model (Figure 2A), used by all participants, comprised three to four appointments: one or two pre-insertion consultations, the insertion procedure appointment and one follow-up appointment:
So, it’s one consultation, insertion, one follow-up. Some people need two if they have questions or are unsure and that’s fine. It’s a long consult for the counselling, it’s a long consult for the insertion and a short consult for follow-up. (GP3)
Some GPs would try to fit the IUD journey into three appointments. However, it was often necessary to split the pre-insertion consultation over two appointments due to time constraints and to conduct eligibility assessments, resulting in four appointments in total. Some participants indicated that some women might be discouraged by multiple appointments. Therefore, to prevent this, some participants would book longer insertion appointments to perform the pre-insertion assessments on the day.
All but three participants discussed poor Medicare rebates and how this affected their service delivery. Many acknowledged that four appointments might discourage women due to associated costs but that, because of low rebates, more appointments allowed practices to provide a profitable service. Consequently, many described the rebate as, ‘terrible’ (GP3), ‘ridiculous’ (GP1, GP5, GP12 and GP17), ‘disrespectful’ (GP16) and discouraging for current and new providers.
After providing contraceptive counselling, the patient might decide not to have the insertion or be deemed ineligible, wasting valuable time and being cost-prohibitive for the practice. Participants had different opinions about having additional pre-insertion appointments for investigations for STI checks, blood pregnancy tests, pap smears and internal examinations, and/or to discuss the results of the test and provide further contraceptive counselling. Those ‘in the country (that are) very pressed for time’ (GP19) would use telehealth to decrease in-person appointment numbers. In addition, only one GP limited insertion to during menses as they ‘follow the guidelines’ (GP6). They did, however, acknowledge that because they only insert during menses they had to be ‘flexible’ (GP6) to not further delay insertion.
Most participants delivered follow-up appointments. The length between insertion and follow-up varied, from two to six weeks, with most participants arranging a follow-up consultation at least four weeks after insertion. For the common model, follow-up was in-clinic with the inserter and not their regular GP or referring practitioner for safety checks and to ‘make sure it’s all alright’ (GP11).
Model 2: Streamlined model (maximum two appointments)
The second most operated approach by GPs, the streamlined model, consisted of a maximum of two appointments with the GP IUD provider (Figure 2B). Patients would be referred to a GP IUD provider for insertion after their pre-insertion consultation and would either have a follow-up appointment with the inserting GP or the GP they initially presented to:
If the other doctors have already spoken to them, then I will just see them for the procedure … As a follow-up, I want to see them. I prefer them to see me rather than their regular doctor. (GP9)
This model required the involvement of other GPs to minimise appointments with the IUD provider, typically in the form of referral. Both internal (eg other GPs within the participants’ clinics) and external (eg local hospitals or family planning centres) referrals were reported. Referrals could increase the number of appointments where duplication of pre-insertion consultations occurred. For follow-up, most participants who got referrals would refer back to the initial GP. One participant explained that this promoted more referrals because the initial doctor would feel more involved in the process and less scared of ‘patient poaching’ (GP18). However, one participant stated that they always ‘prefer (patients) to see (themselves) rather than their regular doctor’ (GP9) to make sure all appropriate checks are conducted.
Model 3: Same-day insertion (two or three appointments)
Five participants delivered a same-day insertion service (Figure 2C). This model had two pathways: one where the GP IUD provider has two appointments (a pre-insertion consultation and the insertion procedure) with the patient in one day, and another where the participant delivers the service in one appointment:
If (patients) already have a script from their own doctor and they’re certain they want it inserted, they book for a 40-minute appointment with me. So, I can meet them, take their full history, go through the consent process in addition to inserting the IUD on the same-day. (GP15)
For same-day insertion to be feasible, participants required availability in their schedule for that day, which can be rare. Same-day insertion with a single appointment was more common. This occurred on a case-by-case basis, where some providers would only perform same-day insertion for specific reasons, such as using the copper IUD as emergency contraception or the provider believing the patient was at risk of an unintended pregnancy.
Task-sharing model
Most GPs used task sharing to assist IUD service provision. Task sharing involved other GP providers, non-providing GPs and nurses. Where task sharing occurred, it generally used nurses to assist throughout the procedure, with 11 (55%) participants describing nurse assistance to complete the insertion. Only one participant described a nurse-led MoC. The nurses’ scope of practice, as perceived by the participants, included undertaking investigations and examinations, such as pregnancy testing and cervical cancer screening, as well as observations and continuous monitoring, applying local anaesthetic to the patient’s cervix, completing patient information and insertion set-up and clean-up. Some participants described limited task-sharing arrangements:
(The nurses) literally just stand at the other end of the bed and squeeze the patient’s hand, and that’s it. (GP11)
Others described working as a ‘team’ (GP6, GP16) with the nurse.
Adaptations to IUD service delivery
Participants discussed several adaptations they often made to service delivery (Figure 3). Changes in participants’ service delivery were primarily due to COVID-19, newly available research evidence and to suit patients’ needs (eg distance from practice and socioeconomic status). COVID-19 caused some participants to move from the common model to a streamlined approach that included pre-insertion telehealth consultation(s), and investigations being conducted on the day of the insertion. This model was facilitated by ‘electronic scripts as well because (they) can just send (the patient) the script’ (GP14). Another example of telehealth facilitating MoC adaption was using it for pre-insertion consultations, particularly when GPs provided three pre-insertion appointments. This model was typically followed when patients were younger, having their first IUD inserted or unsure about the insertion and therefore required further counselling.
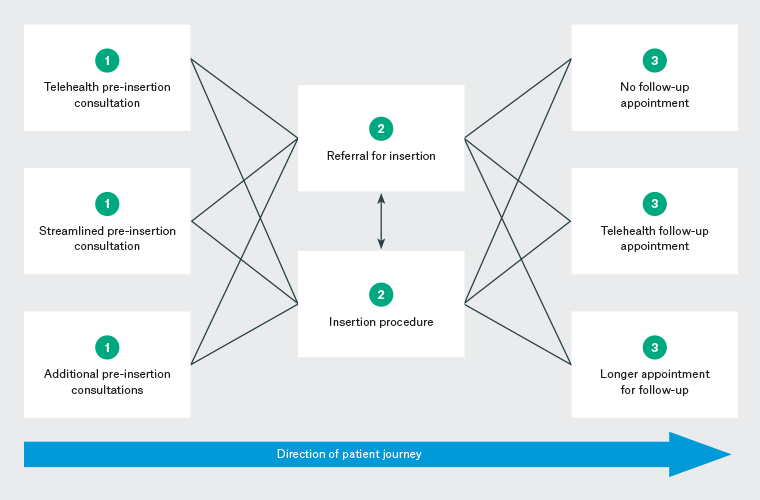
Figure 3. Diagrammatic representation of the adaptable model of care for the provision of intrauterine devices. Click here to enlarge
Follow-up appointments were also moved to telehealth, lengthened to a long consultation, both or dismissed altogether. Longer follow-up consultations were usually for patients who were younger, had concerns or symptoms and/or had their first IUD inserted. Conversely, those who were older, felt confident, had no symptoms and/or had had an IUD before were not ‘pushed’ (GP14) into attending their follow-up appointment, but were still generally ‘encouraged’ to attend (GP15).
All but two participants regularly referred their patients to specialists, external organisations and both public and private hospital systems, for difficult or failed insertions. One also did so for sexually inactive patients because the patient could be directly scheduled to see them at the local hospital for insertion under sedation. Although reasons for referral were varied (ie for those wanting sedation or anaesthesia, those with a cervical stenosis, difficult insertions or those who were sexually inactive), participants followed ‘the first rule, you need to be safe’ (GP4) and patients’ preferences.
Discussion
Three models of IUD provision were generally used by participants: common, streamlined and same-day insertion. Participants also described the use of task-sharing arrangements and adapting service delivery to facilitate IUD provision. Both provider and patient factors, such as practitioner preferences and a patient’s age and parity, as well as external factors, such as appointment availability and the COVID-19 pandemic, affected which model was used. However, this study also identified that when applying the quality framework,26 Australian GP IUD services do not always prioritise acceptability, accessibility, appropriateness, efficiency and effectiveness.
Most participants used the common model for IUD provision due to the organisation of general practice appointments, where the IUD patient journey is spread over three to four appointments and where individual appointment times might be shorter. Therefore, this model might be considered high quality for providers. However, it might be of the lowest quality in terms of meeting patients’ needs due to the need to attend multiple appointments. Participants indicated that some women are discouraged by multiple appointments, a finding consistent with data from the US, where almost half the women who wanted an IUD after their first consultation did not return for insertion.33 Increasing the quality of IUD MoC will facilitate women’s ability to access the service; however, quality is not the only barrier to IUD insertions in Australian general practice. The limited number of GP IUD providers in Australia9 increases the workload of current providers and limits women’s access.
Misconceptions surrounding IUD services and limited training availability reduces GPs’ ability to learn to and provide IUD insertions.15 One GP in this study limited insertion to menses. This might be due to misinterpretation of current guidelines provided by The Royal Australian College of General Practitioners (RACGP)34 limiting women’s access to 5–12 days of the month.22 In addition, these RACGP guidelines describe the IUD journey in a two- to three-stage process (an initial consultation, which might include insertion, the insertion appointment and follow-up). Other literature and some GPs in this study felt that the need for a follow-up appointment might have little benefit and in some cases could be managed by telephone if needed.23 Further, additional appointments can burden women with extra out-of-pocket costs, such as those for the appointment/s, travel and time off work, adding to the cost of the device and insertion, acting as a barrier to IUD services.10 In some countries, such as the UK and Sweden, insertion procedures are free, and devices are free in the UK.35 Overall, participants attributed high out-of-pocket costs due to inadequate Medicare rebates. Due to costs and multiple appointments, the acceptability, accessibility, cost-appropriateness and efficiency of this service are diminished.26 However, recent changes in funding, and the Medicare Benefit Schedule (MBS) IUD rebate increasing, might help the sustainability and cost-effectiveness of IUD provision.36 Changes in telehealth Medicare item numbers for sexual or reproductive services can decrease in-person appointments for a more streamlined approach,37 such as completing follow-up via telehealth, to enhance patient acceptability, access and efficiency.23 This flexibility in service delivery supports women’s needs, particularly during a pandemic or other life stage demands.
Some participants used a streamlined model via internal referral. These referrals can increase the number of appointments and, although there might be a need for opportunities to ask additional questions and establish rapport prior to the procedure, practitioners should consider conducting this second appointment via telehealth. This option been shown to be feasible and convenient for contraceptive counselling.38 In addition, the introduction (July 2021) of the telehealth Medicare item numbers for the provision of sexual or reproductive health services has enhanced the feasibility of telehealth in Australian general practice.39
Same-day insertion is a high-quality IUD MoC that prioritises acceptability, appropriateness, accessibility and efficiency while being both safe and effective.8 Same-day insertion reduces potential barriers, such as referral, costs associated with multiple appointments, travel and long wait times.10,40 In addition, this model follows best practice by reducing additional appointments, such as for STI checks, which would otherwise deter some women from receiving this service.33 Our data also correspond with Australian literature that referral and long wait times are barriers to IUD uptake.40 Current workforce pressures, time and workplace organisation are potential practitioner obstacles for same-day insertion. However, initiatives such as the ‘rapid referral pathways’, which can reduce time between service initiation and IUD insertion,8 might help.
Few participants described task-sharing arrangements. This MoC could enhance clinic and procedure efficiency. Although most participants used nurse assistance to expedite the insertion, only one participant described a nurse-led MoC. Although the general practice funding model affects nursing scope of practice,41 both nurse practitioners and registered nurses are well placed to undertake IUD training and provide this care, because procedural outcomes have been found to be comparable to those for GPs.42
A novel finding of the present study was that GPs will regularly swap MoC for IUD provision and adapt them to suit patients’ needs and preferences, increasing the acceptability of the service. Practitioners adapting service delivery, particularly during the pandemic, has been observed elsewhere, such as using telehealth for domestic violence support.43 With the minority of our participants providing streamlined, same-day insertion or optional follow-up, increasing the availability of IUD insertion appointments through task sharing or nurse-led or adaptable MoC might generate more acceptability for and efficiency with this service.
Limitations
The recruitment of participants from six states and metropolitan, inner regional and outer regional locations is a strength of the study. In addition, two coders were used to analyse the results, adding further rigour to the results. Reflexivity and self-awareness of personal factors and past experiences with general practice underpinned the research process to minimise bias. Participants were recruited via convenience and purposive methods, not maximum variation sampling, which might have caused data saturation to be reached prematurely. However, the impact of this was mitigated by the variation in participant demographics. A potential limitation of the study was the sample size (n=20) and that we were unsuccessful in recruiting participants from remote locations or from any territories, and therefore might have missed perspectives from this group of GPs. We did not perform member checking and did not triangulate the results, such as conducting telephone interviews with patients or observing participants’ IUD service delivery, due to the geographical dispersion of participants in relation to the research team and the COVID-19 pandemic. Finally, asking providers about the acceptability of the services is only a proxy measure and legitimate acceptability can only be ascertained by interviewing those who receive the service. Therefore, we suggest future research with patients about their preferred GP IUD MoC.
Conclusion
We identified three models for delivering IUD services currently used by Australian GP IUD providers: common, streamlined and same-day insertion. The quality of current models is non-standardised and largely inadequate, preventing uptake and service provision. The common model was most operated; however, it was not of the highest quality, particularly compared with streamlined and same-day insertion models. In addition, operating only one model can be limiting and does not allow for service adaptation, which is often required in general practice. Overall, quality can be improved, with fewer appointments, providers following current best-practice evidence and the prioritisation of patients’ preferences. Focusing on operating high-quality models, task sharing and adaptability, access to IUD services in general practice can be enhanced.
Key points
- Informed by the quality dimension framework, current IUD models of care are of a low quality.
- GP IUD models of care with fewer appointment numbers and same-day insertion models are feasible and can increase women’s accessibility to this service.
- Practitioners should operate several or adaptable models of care to ensure that they are prioritising both their and their patients’ preferences and needs.
- This study focused on GP IUD providers about IUD models of care. However, interviewing patients about their preferred IUD MoC would add weight to this research.
References
- Taft AJ, Shankar M, Black KI, Mazza D, Hussainy S, Lucke JC. Unintended and unwanted pregnancy in Australia: A cross-sectional, national random telephone survey of prevalence and outcomes. Med J Aust 2018;209(9):407–08. doi: 10.5694/mja17.01094.
- Read C, Bateson D, Weisberg E, Estoesta J. Contraception and pregnancy then and now: Examining the experiences of a cohort of mid-age Australian women. Aust N Z J Obstet Gynaecol 2009;49(4):429–33. doi: 10.1111/j.1479-828X.2009.01031.x.
- Richters J, Grulich AE, de Visser RO, Smith AM, Rissel CE. Sex in Australia: Contraceptive practices among a representative sample of women. Aust N Z J Public Health 2003;27(2):210–16. doi: 10.1111/j.1467-842X.2003.tb00810.x.
- Sundaram A, Vaughan B, Kost K, et al. Contraceptive failure in the United States: Estimates from the 2006–2010 National Survey of Family Growth. Perspect Sex Reprod Health 2017;49(1):7–16. doi: 10.1363/psrh.12017.
- Jatlaoui TC, Riley HEM, Curtis KM. The safety of intrauterine devices among young women: A systematic review. Contraception 2017;95(1):17–39. doi: 10.1016/j.contraception.2016.10.006.
- Yoost J. Understanding benefits and addressing misperceptions and barriers to intrauterine device access among populations in the United States. Patient Prefer Adherence 2014;8:947–57. doi: 10.2147/PPA.S45710.
- Grzeskowiak LE, Calabretto H, Amos N, Mazza D, Ilomaki J. Changes in use of hormonal long-acting reversible contraceptive methods in Australia between 2006 and 2018: A population-based study. Aust N Z J Obstet Gynaecol 2021;61(1):128–34. doi: 10.1111/ajo.13257.
- Mazza D, Watson CJ, Taft A, Lucke J, McGeechan K, Haas M, et al. Increasing long-acting reversible contraceptives: the Australian Contraceptive ChOice pRoject (ACCORd) cluster randomized trial. Am J Obstet Gynecol 2020;222(4S):S921.e1–e13. doi: 10.1016/j.ajog.2019.11.1267.
- Stewart M, Digiusto E, Bateson D, South R, Black KI. Outcomes of intrauterine device insertion training for doctors working in primary care. Aust Fam Physician 2016;45(11):837–41.
- Garrett CC, Keogh LA, Kavanagh A, Tomnay J, Hocking JS. Understanding the low uptake of long-acting reversible contraception by young women in Australia: A qualitative study. BMC Women’s Health 2015;15(1):72. doi: 10.1186/s12905-015-0227-9.
- El Ayadi AM, Rocca CH, Averbach SH, et al. Intrauterine devices and sexually transmitted infection among older adolescents and young adults in a cluster randomized trial. J Pediatr Adolesc Gynecol 2021;34(3):355–61. doi: 10.1016/j.jpag.2020.11.022.
- Committee on Practice Bulletins-Gynecology, Long-Acting Reversible Contraception Work Group. Practice bulletin no. 186: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol 2017;130(5):e251–69. doi: 10.1097/aog.0000000000002400.
- Grentzer JM, Peipert JF, Zhao Q, McNicholas C, Secura GM, Madden T. Risk-based screening for Chlamydia trachomatis and Neisseria gonorrhoeae prior to intrauterine device insertion. Contraception 2015;92(4):313–18. doi: 10.1016/j.contraception.2015.06.012.
- Black KI, Lotke P, Lira J, Peers T, Zite NB. Global survey of healthcare practitioners’ beliefs and practices around intrauterine contraceptive method use in nulliparous women. Contraception 2013;88(5):650–56. doi: 10.1016/j.contraception.2013.06.005.
- Turner R, Tapley A, Sweeney S, Magin P. Barriers to prescribing of long-acting reversible contraception (LARC) by general practitioner registrars: A cross-sectional questionnaire. Aust N Z J Obstet Gynaecol 2021;61(3):469–73. doi: 10.1111/ajo.13320.
- Kelly PJ, Cheng AL, Carlson K, Witt J. Advanced practice registered nurses and long-acting reversible contraception. J Midwifery Womens Health 2017;62(2):190–95. doi: 10.1111/jmwh.12578.
- Harper CC, Speidel JJ, Drey EA, Trussell J, Blum M, Darney PD. Copper intrauterine device for emergency contraception: Clinical practice among contraceptive providers. Obstet Gynecol 2012;119(2 Pt 1):220–26. doi: 10.1097/AOG.0b013e3182429e0d.
- Thompson KM, Rocca CH, Kohn JE, et al. Public funding for contraception, provider training, and use of highly effective contraceptives: A cluster randomized trial. Am J Public Health 2016;106(3):541–46. doi: 10.2105/AJPH.2015.303001.
- Rocca CH, Thompson KM, Goodman S, Westhoff CL, Harper CC. Funding policies and postabortion long-acting reversible contraception: Results from a cluster randomized trial. Am J Obstet Gynecol 2016;214(6):716.e1–e8. doi: 10.1016/j.ajog.2015.12.009.
- Langston AM, Rosario L, Westhoff CL. Structured contraceptive counseling – A randomized controlled trial. Patient Educ Couns 2010;81(3):362–67. doi: 10.1016/j.pec.2010.08.006.
- Lanzola EL, Ketvertis K. Intrauterine device. StatPearls, 2023. Available at www.ncbi.nlm.nih.gov/books/NBK557403/ [Accessed 12 September 2023].
- Whiteman MK, Tyler CP, Folger SG, Gaffield ME, Curtis KM. When can a woman have an intrauterine device inserted? A systematic review. Contraception 2013;87(5):666–73. doi: 10.1016/j.contraception.2012.08.015.
- Bernard A, Satterwhite CL, Reddy M. Frequency of 6-week follow-up appointment scheduling after intrauterine device insertion. BMJ Sex Reprod Health 2018;44(1):33–36. doi: 10.1136/bmjsrh-2017-101791.
- Australian Bureau of Statistics (ABS). National health survey: First results. ABS, 2018. Available at www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/2017-18 [Accessed 12 September 2023].
- Morse J, Hutchinson S, Penrod J. From theory to practice: The development of assessment guides from qualitatively derived theory. Qual Health Res 1998;8(3):329–40. doi: 10.1177/104973239800800304.
- Booth BJ, Snowdon T. A quality framework for Australian general practice. Aust Fam Physician 2007;36(1–2):8–11.
- Deb S, Subasinghe AK, Mazza D. Providing medical abortion in general practice: General practitioner insights and tips for future providers. Aust J Gen Pract 2020;49(6):331–37. doi: 10.31128/AJGP-01-20-5198.
- World Health Organization (WHO). Quality of care: A process for making strategic choices in health systems. WHO, 2006. Available at https://apps.who.int/iris/bitstream/handle/10665/43470/9241563249_eng.pdf?sequence=1&isAllowed=y [Accessed 12 September 2023].
- Gardner K, Mazza D. Quality in general practice – definitions and frameworks. Aust Fam Physician 2012;41(3):151–54.
- International Planned Parenthood Federation (IPPF). Quality of care framework. IPPF, 2016.
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. National Academies Press, 2001.
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 2019;11(4):589–97. doi: 10.1080/2159676X.2019.1628806.
- Bergin A, Tristan S, Terplan M, Gilliam ML, Whitaker AK. A missed opportunity for care: Two visit IUD insertion protocols inhibit placement. Contraception 2012;86(6):694–97. doi: 10.1016/j.contraception.2012.05.011.
- The Royal Australian College of General Practitioners (RACGP) Specific Interests Sexual Health Medicine and RACGP Expert Committee. Intrauterine devices/systems – resources for general practice. RACGP, 2020. Available at www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/iuds-systems-resources-for-general-practice [Accessed 12 September 2023].
- Buhling KJ, Zite NB, Lotke P, Black K; INTRA Writing Group. Worldwide use of intrauterine contraception: A review. Contraception 2014;89(3):162–73. doi: 10.1016/j.contraception.2013.11.011.
- Australian Government Department of Health. March 2022 news: News containing information on changes to the MBS for 1 March 2022. Australian Government, 2022. Available at www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/news-220301 [Accessed 12 September 2023].
- Australian Government Department of Health. There are 24 new MBS telehealth items for blood borne viruses, sexual and reproductive health services. Australian Government, 2021. Available at www.servicesaustralia.gov.au/organisations/health-professionals/news/there-are-24-new-mbs-telehealth-items-blood-borne-viruses-sexual-and-reproductive-health-services.
- Liotta M. In Practice: MBS changes from 1 March. newsGP, 2022. Available at www1.racgp.org.au/newsgp/racgp/in-practice-mbs-changes-from-1-march [Accessed 6 October 2023].
- Stifani BM, Avila K, Levi EE. Telemedicine for contraceptive counseling: An exploratory survey of US family planning providers following rapid adoption of services during the COVID-19 pandemic. Contraception 2021;103(3):157–62. doi: 10.1016/j.contraception.2020.11.006.
- The Royal Australian College of General Practitioners (RACGP). Changes to MBS telehealth items from 1 July 2021. RACGP, 2021. Available at www.racgp.org.au/running-a-practice/practice-resources/medicare/medicare-benefits-schedule/changes-to-mbs-telehealth-items [Accessed 6 October 2023].
- Lodge G, Sanci L, Temple-Smith MJ. GPs perspectives on prescribing intrauterine contraceptive devices. Aust Fam Physician 2017;46(5):328–33.
- McInnes S, Peters K, Bonney A, Halcomb E. The influence of funding models on collaboration in Australian general practice. Aust J Prim Health 2017;23(1):31–36. doi: 10.1071/PY16017.
- Kemeny F, Digiusto E, Bateson D. Insertion of intrauterine contraceptive devices by registered nurses in Australia. Aust N Z J Obstet Gynaecol 2016;56(1):92–96. doi: 10.1111/ajo.12427.
- Cortis N, Smyth C, Valentine K, Breckenridge J, Cullen P. Adapting service delivery during COVID 19: Experiences of domestic violence practitioners. Br J Soc Work 2021;51(5):1779–98. doi: 10.1093/bjsw/bcab105.